Every state has opportunities to improve health care for its residents, according to The Commonwealth Fund’s latest Scorecard on State Health System Performance, 2017 Edition. But what kinds of advances could states expect to see for their efforts? To help answer that question, we’ve updated our interactive tool that illustrates the gains states could make by performing at the level of leading states on 14 measures of health care access, quality, and outcomes.
Say, for instance, leaders in Georgia wanted to know how expanding Medicaid for low-income residents could reduce the number of adults who say they skip needed care because of cost. Using our tool, they could explore the experiences of other states that have already expanded Medicaid and see how Georgia lines up and could benefit.
Let’s look at an example.
The Scorecard tells us that in 2015, insured rates among working-age adults (i.e., those ages 19 to 64) averaged 91 percent in states that had expanded their Medicaid programs under the Affordable Care Act,1 compared to 84 percent in states that had not expanded. On average, 11 percent of adults in expansion states reported not getting care when needed because of cost, compared to 14 percent in nonexpansion states.
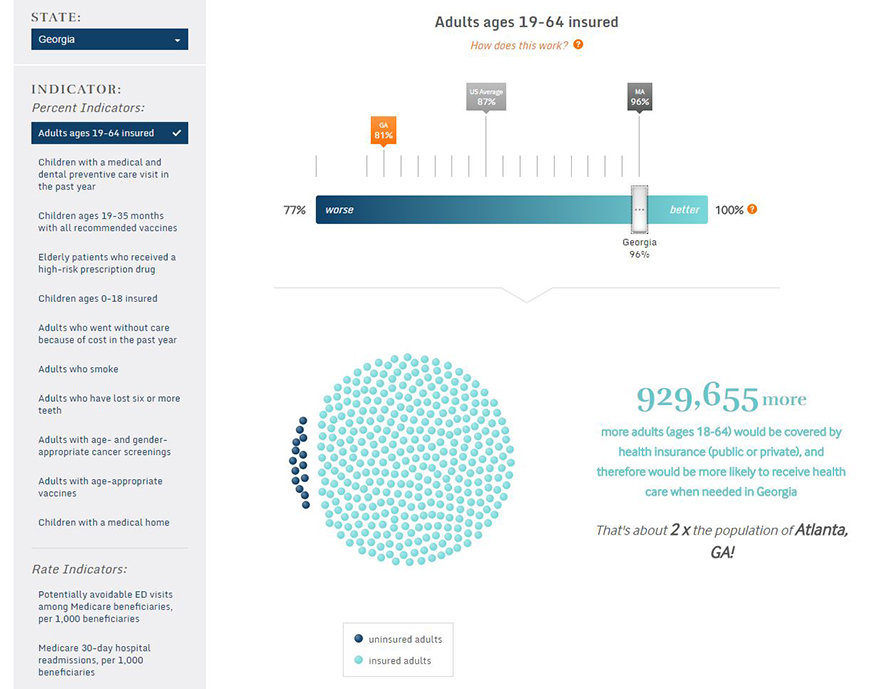
Using our example of Georgia, which as of April 2017 had not expanded Medicaid, we can see that the state still made gains in insurance coverage under the ACA. The share of insured adults rose from 74 percent in 2013, the year before the ACA’s major coverage expansions took effect, to 81 percent in 2015. Accompanying this increase, fewer adults in Georgia reported not getting needed care because of cost in 2015 (16%) than in 2013 (20%). These gains were likely driven by the ACA’s premium subsidies available to low- and moderate-income individuals and families who purchase private insurance in the marketplace. Many Georgians benefited from the increased coverage options available under the ACA; still more could benefit if the state expanded its Medicaid program.
Using the interactive tool, you can see that if the insured rate among working-age adults in Georgia rose to the expansion-state average of 91 percent, an estimated 619,770 more adults in Georgia would be insured. Similarly, if the share of adults not able to get care because of cost in Georgia dropped to the expansion-state average of 11 percent, about 382,207 fewer Georgians would skip needed care.
The table below highlights the gains that would be realized in other nonexpansion states that performed below the average rates achieved in states that expanded Medicaid.
This same approach can be used to estimate the impact of other improvements in health and health care. For example, if Virginia, where the rate of adult smokers matches the adult smoking rate in the U.S. as a whole (17%), improved to the level of a better-performing state, like California, there would be nearly 380,978 fewer Virginians who smoke cigarettes. If California improved to the level of Utah—the best-performing state on this indicator—599,101 fewer Californians would smoke.
We encourage you to use this tool—and the Scorecard—to explore performance in your state, learn from other states’ experiences, and set achievable goals for improvement. As always, we welcome your feedback and suggestions.