
Last year, I ended my annual message by noting: “In the coming months, elections will transform the nation once again, with still unforeseeable consequences for the U.S. health system.”
Well, the 2016 national elections have come and gone, and the long-term consequences for U.S. health care are still potentially profound and uncertain. As I write, Congress debates repeal of the Affordable Care Act, or ACA. Most of the proposals for its replacement would leave many Americans less confident about their health care and financial security.
Meanwhile, new threats from foreign powers, continuing terrorist incidents, global hacking events, and even the latest projections for climate change leave many of us feeling uneasy—as if we walk on trembling ground.
At times of dramatic change, fear and anxiety can become pervasive and overwhelming. Troubling visions of authoritarianism or chaos, of political persecution, and even civil war disturb our waking thoughts and nightly dreams. It can be emotionally, almost physically, paralyzing.
As Mark Twain allegedly quipped, "History doesn’t repeat itself, but it often rhymes." Looking for those historical rhymes can provide perspective at times of disquiet. This may be particularly true for younger members of our attentive public, who have not lived through, and emerged safely from, some of the dark periods we have experienced as a country.
America’s 241 years of nationhood have been tumultuous. Events have repeatedly challenged the viability of our democracy. In the Civil War, an estimated 650,000 Americans died, the equivalent of 1 in 43 citizens. During the Great Depression, unemployment reached 25 percent, compared to 10 percent at the height of the 2007–2009 recession. Economic pain gave rise to extremist movements. Communism and fascism both had large followings in the United States, as they did in Europe.
World War II constituted a truly mortal threat to the future of Western civilization. From 1939 to 1942, the allies suffered repeated defeats at the hands of fascist forces. Nevertheless, except for the shameful internment of Japanese Americans, our democratic institutions continued to function, with regular elections and the rule of law.
In the turbulent 1960s, a president, a presidential candidate, and leading civil rights leaders and activists were assassinated. Inner cities burned. A protracted, bloody war in Southeast Asia divided and demoralized the nation.
And in the ‘70s, when a rogue White House burgled the offices of the opposing party and the president ordered a cover-up, the media, Congress, and the judiciary combined to force his resignation.
Varied as these events were, they show how frequently crises test our nation, and how resilient our democracy has proven over time. They also show how important it is for defenders of our freedoms to remain vigilant. No civilization—no matter how mighty or seemingly stable—is invulnerable.
Only the values and courage of a free citizenry and its leaders can assure that we continue to rise to the challenges we will inevitably encounter.
A critical role in preserving our values and our institutions falls to the nongovernmental bodies that constitute our civil society. These include our houses of worship, our schools and universities, and our many charitable and philanthropic organizations. The Commonwealth Fund is one of these.
As an endowed philanthropy, The Commonwealth Fund has for 99 years enjoyed the extraordinary privilege of economic independence. Currently, the Fund is dedicated to creating a high-performance health system in the United States. The principal way we work to achieve that mission is by conducting and supporting research that produces evidence—facts—to focus reforms that will help more people afford high-quality health care.
In service of that mission, in 2016 we continued to track the rollout of the ACA, and documented historic progress in the numbers of Americans with health coverage and the ability of people to buy health insurance on their own.
We teamed with four other foundations to create a new resource for health professionals—The Playbook—dedicated to providing better care for the sickest and frailest among us, who also drive most of the spending in our health care system.
We examined the health care proposals of the presidential candidates and, after the election, looked at the likely effects of ACA repeal and replacement.
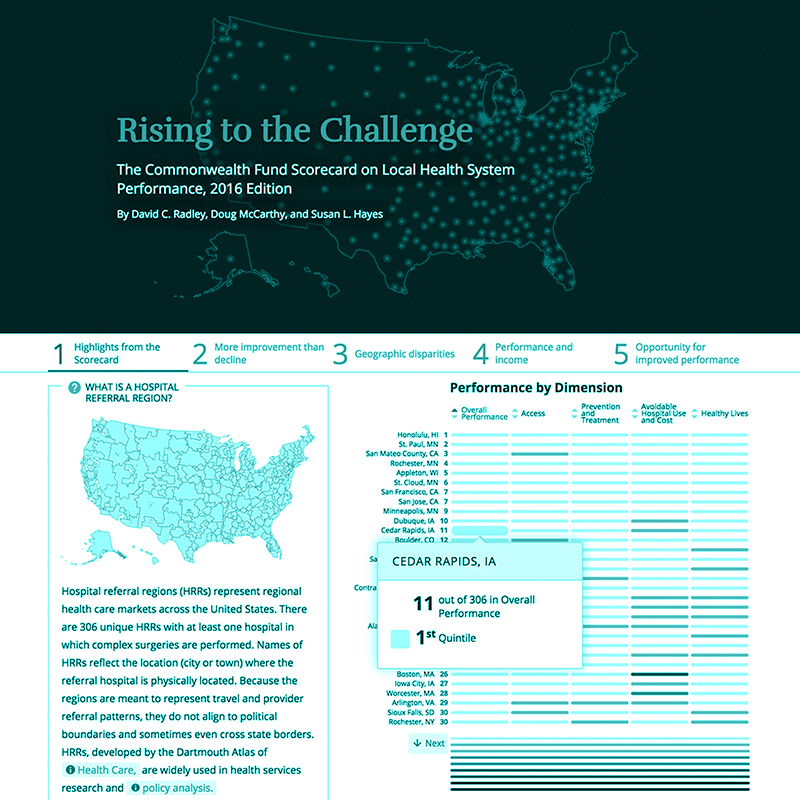
We released the latest in our health system scorecard series, which found great improvement in access to care but wild variation in progress among local communities.
We continued to promote learning from abroad through our case studies of health care delivery models, from programs helping the sickest and costliest patients to frugal innovations pioneered by developing countries.
In this report, you will learn more about these and many other projects, the people and communities who benefit, and the dedicated individuals who do the work.
As The Commonwealth Fund nears completion of a century of action in pursuit of a high performing health care system for all Americans, we commit to a redoubling of our efforts. To the Fund, that means providing an objective, evidence-based view of our health care system. It means identifying and supporting new and effective models for improvement. And it means striving for consensus and innovation rather than yielding to partisanship and the status quo.

Focus on High-Need, High-Cost Patients

The Affordable Care Act’s Impact: Just the Facts

Medicaid and the Safety Net: What’s at Stake
Health Trends: Probing Deeper
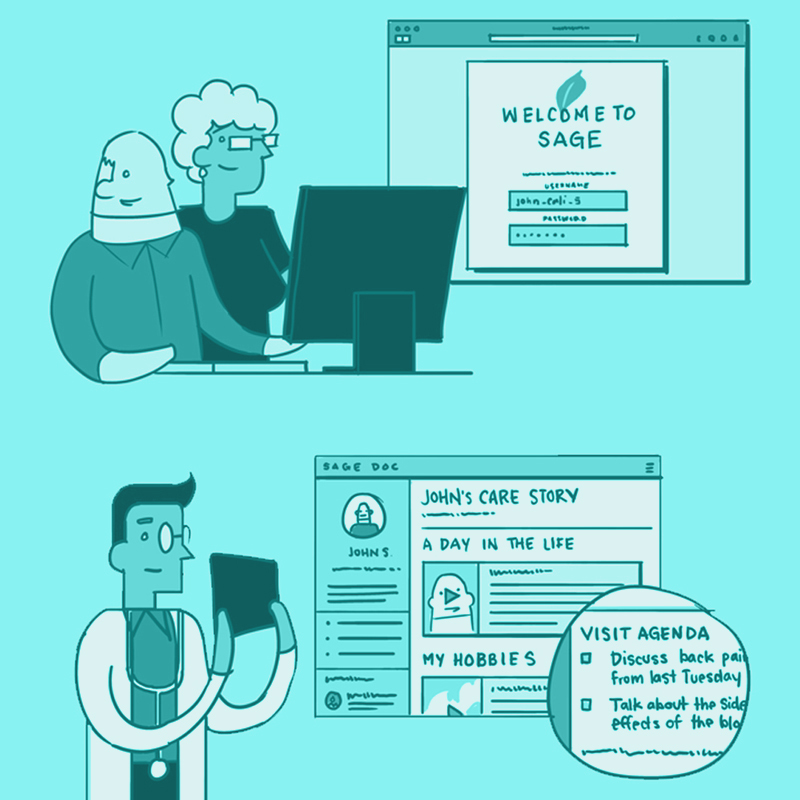
Empowering Patients Through Technology

The Cost of American Health Care

Looking Abroad

Taking on the Issues of the Day
Over the course of the fiscal year ending June 30, 2016, the average market value of The Commonwealth Fund endowment fell from $747 million to $711 million.
Over the last decade, The Commonwealth Fund has been able to preserve the purchasing power of its endowment, benefiting from robust investment returns over the majority of the period since the 2008–09 financial crisis. The investment environment in FY2016 was challenging, however, particularly so for managers pursuing active investment strategies. The performance of the Fund’s endowment is measured against both a passive benchmark reflecting target portfolio allocations and a benchmark consisting of the foundation sector’s target spending rate plus inflation. Over the one-year, three-year, five-year and 10-year periods ending on June 30, 2016, the net return on the Fund’s endowment has been −4.4 percent, 5.0 percent, 5.0 percent, and 5.2 percent, respectively. These returns compare unfavorably to benchmarks.
Prudent management of expenses and the investment returns on the endowment has enabled the Fund to maintain modest growth expenditures to support its mission over the past four years. During FY2015–16, the Fund increased its expenditures by 4 percent, to $33.7 million, and maintained a distribution ratio of just under 5.0 percent.
As a value-added foundation, The Commonwealth Fund seeks to achieve an appropriate balance between its external grantmaking activities and its active intramural research, communications, and program management work. To maintain its role in informing health policy and promoting a high performance health system, the Fund increased its budget to $35 million for the current 2016-17 fiscal year.
In FY2015–16, The Commonwealth Fund made 113 grants, totaling $21.5 million. The products of these grants resulted in more than 350 publications and more than 700 mentions in the media. The geographic distribution of grants during the past year is as follows: Mid-Atlantic: 59%, Northeast: 14%, Midwest: 10%, West: 8%, Southeast: 4%. Approximately 4% of the projects are international.
Lois Quam, CEO of Pathfinder International, a champion for sexual and reproductive health and rights worldwide, was elected to The Commonwealth Fund’s Board of Directors in July 2016. She began her term in April 2017.
Since 1957, Pathfinder has partnered with local governments, communities, and health systems to expand access to contraception, promote healthy pregnancies, save women’s lives, and stop the spread of new HIV infections. Quam joined the organization in February 2017 after serving as the Nature Conservancy’s chief operating officer.
From 2011 to 2014, Quam was a special advisor to Secretary of State Hillary Rodham Clinton. She launched and led President Barack Obama’s Global Health Initiative, working on solutions to health challenges facing people across 80 countries. She has also held executive positions with UnitedHealth Group and on three occasions was named one of Fortune’s “50 Most Powerful Women in American Business.” A former Rhodes Scholar, Quam earned a B.A. and M.A. from Oxford College and a B.A. from Macalester College.
“Lois Quam brings to The Commonwealth Fund’s Board a wealth of experience in health care coverage and delivery in both the private and public sectors,” said Commonwealth Fund Board Chairman Benjamin K. Chu, M.D., at the time of Quam’s appointment. “Her insights will be invaluable to informing our deliberations as the Fund continues its work to move the U.S. to a high performance health system.”
Laura Walker, president and CEO of New York Public Radio, also joined The Commonwealth Fund’s Board of Directors in April 2017. Under Walker’s leadership, New York Public Radio’s audience has grown from 1 million to 23.9 million monthly, and more than $100 million has been raised for long-term investment.
In 2008, Walker received the Edgar R. Murrow award from the Corporation for Public Broadcasting, the industry’s highest honor. She also received a Peabody Award for Broadcast Excellence during her tenure as a producer at NPR.
“We are fortunate to have Laura Walker join our Board as The Commonwealth Fund pursues its goal of ensuring our health care system can provide high-quality care to everyone, especially the most vulnerable in our society,” said Commonwealth Fund President David Blumenthal, M.D.
Earlier in her career, Walker worked at Carnegie Hall, the Sesame Workshop, the Boston Consulting Group, and Eurasia Press, as well as in print journalism. She graduated with a B.A. in history, magna cum laude, from Wesleyan University, and has an M.B.A. from the Yale School of Management.
Two long-serving Commonwealth Fund directors retired from the Board in July 2016.
Jane Henney, M.D., who joined the Fund’s Board in 2001 and chaired its audit and compliance committee, was “a terrific advocate for governance as a key attribute of effective philanthropy,” said Commonwealth Fund President David Blumenthal, M.D. Henney served as the commissioner of the U.S. Food and Drug administration from 1998 to 2001 and earlier was deputy director for the National Cancer Institute.
Henney’s many academic leadership positions have included senior vice president and provost for health affairs at the University of Cincinnati, vice president for health sciences at the University of New Mexico, and vice president for health programs at the University of Kansas Medical Center. In 2014, she became the National Academy of Medicine’s home secretary.
Robert C. Pozen also joined The Commonwealth Fund’s Board in 2001 and was a key member of the investment committee. The chairman emeritus of MFS Investment Management, the oldest mutual fund company in the United States, he was critically important in helping the Fund navigate smoothly through the treacherous waters following the 2008 U.S. financial crisis.
Pozen has a long record of public and nonprofit service, including tenures as Secretary of Economic Affairs for the state of Massachusetts under Governor Mitt Romney and member of President George W. Bush’s Commission to Strengthen Social Security, for which developed two models for closing the program’s deficit. He is a senior lecturer at the MIT Sloan School of Management and a senior fellow at the Brookings Institution.
Shawn Bishop was named The Commonwealth Fund’s new Vice President for Cost Control and Medicare in February 2016. Bishop oversees two programs: Controlling Health Care Costs, which monitors and analyzes spending in the public and private health care sectors; and Advancing Medicare, which identifies ways the Medicare program can better serve its beneficiaries and perform as a testbed for health system improvement.
A former senior vice president of research with the Marwood Group, a health care consultancy, Bishop has held a variety of posts at the Congressional Budget Office and the Centers for Medicare and Medicaid Services. Earlier, as a U.S. Senate Finance Committee staff member, she advised on legislation and policy oversight related to Medicare Advantage, Medicare Part D, comparative effectiveness research, and health care reform. She also developed and negotiated major provisions of the Affordable Care Act and other key health legislation.
Lovisa Gustafsson joined The Commonwealth Fund in September 2016 as the program officer for Breakthrough Health Care Opportunities. She is responsible for developing and managing all aspects of the program, identifying new breakthrough opportunities, and developing a strategy to build on initiatives already under way.
Prior to joining the Fund, she was a senior vice president for the Marwood Group, for which she managed outsourced private equity due diligence and strategy consulting engagements. She has also held positions with McKesson, Kaiser Permanente, the Commonwealth of Massachusetts Office of Medicaid, and Avalere Health.
Dr. Chu is president and CEO of Memorial Hermann Health System and former executive vice president of Kaiser Foundation Hospitals and Health Plan, Inc.
Ms. Russell is an award-winning freelance journalist who has written about science, health, and the environment for more than three decades.
Ms. Bisognano, a prominent authority on improving health care systems, is president emerita and senior fellow of the Institute for Healthcare Improvement.
Dr. Blumenthal is president of The Commonwealth Fund. Prior to joining the Fund in 2013, he was the Samuel O. Thier Professor of Medicine at Harvard Medical School and Chief Health Information and Innovation Officer at Partners Healthcare System in Boston. From 2009 to 2011, he served as U.S. National Coordinator for Health Information Technology.
Dr. Blutt is founder and chief executive officer of the health care investment firm Consonance Capital. He is also clinical assistant professor of medicine at Weill Cornell Medical College and the Graduate School of Medical Sciences of Cornell University.
Ms. Burke is a faculty member and former executive dean at the Harvard Kennedy School of Government.
Dr. Drake, a physician-scientist, administrative leader, and teacher, is the 15th president of Ohio State University. He is a former chancellor of the University of California, Irvine.
Dr. Hamburg, former commissioner of the U.S. Food and Drug Administration, currently serves as foreign secretary for the National Academy of Medicine (formerly the Institute of Medicine) and sits on several other boards and advisory committees.
Ms. Haslanger, who has spent more than 30 years in health care policy, research, and delivery, is chief executive officer of JASA (Jewish Association Serving the Aging), a New York-based nonprofit.
Ms. Quam is the chief executive officer of Pathfinder International and is on the faculty at Columbia University’s Mailman School of Public Health.
Dr. Smith is a member of the clinical faculty of the University of California, San Francisco, and an attending physician at the Positive Health Program for HIV/AIDS care at San Francisco General Hospital. He was the founding president and chief executive officer of the California HealthCare Foundation.
Mr. Stevens is the CEO of National Health Service, England. He previously served as executive vice president of UnitedHealth Group.
Ms. Walker is president and chief executive officer of New York Public Radio.
Mr. Yun is president of Franklin Templeton Investments and president of Fiduciary Trust, with overall responsibility for all investment management and research activities.
Benjamin K. Chu, M.D., Chairman
Maureen Bisognano
David Blumenthal, M.D..
Cristine Russell
William Y. Yun
Sheila Burke
Sheila Burke, Chairman
Kathryn Haslanger
Mark Smith, M.D.
Laura Walker
William Y. Yun
William Y. Yun, Chairman
Maureen Bisognano
David Blumenthal, M.D.
Mitchell Blutt, M.D.
Benjamin K. Chu, M.D.
Lois Quam
Simon Stevens
Cristine Russell, Chairman
David Blumenthal, M.D.
Sheila Burke
Benjamin K. Chu, M.D.
Michael V. Drake, M.D.
Margaret Hamburg, M.D.