Introduction
After a bad fall landed Dianna Boggs in a wheelchair, she needed more help than nearby family members could provide. At age 75 and living alone in rural Virginia, Boggs might have ended up in a nursing home like many others in her situation. But instead she opted to join Mountain Empire’s Program of All-Inclusive Care for the Elderly (PACE), allowing her to stay in her own home, within view of the mountains she loves.
Mountain Empire PACE staff equipped Dianna’s home so she can use the bathroom and bathe on her own. A transit service brings her to a day center five days a week for medical checkups and social activities with other elders, as well as to the grocery store and outings with friends. Since enrolling three years ago, Boggs has regained enough strength in her legs to use a cardio machine for a mile, cook most of her meals, and care for herself. “If it wasn’t for PACE, I would just sit home and dry up,” she says.
Mountain Empire is one of the newest of more than 100 independent PACE organizations across the nation that serve both as health plans and as medical and long-term service providers to elders — offering meals, checkups, rehabilitation services, home visits, and many other supports that enable enrollees to preserve their independence. The model for PACE dates back to 1971, when a public health dentist and social worker from the San Francisco Public Health Department working in Chinatown-North Beach noticed that as their clients aged, many needed extra support but dreaded moving into nursing homes. They founded On Lok Senior Health Services as an alternative to institutional care that would allow elders to “age in place” in their homes; on lok is Cantonese for “peaceful, happy abode.”1
On Lok’s founders were particularly concerned about elderly clients who suffered when their various clinicians failed to work together, sometimes leading to complications that necessitated moves into institutional care. They designed On Lok to promote what was then an innovative approach: coordinating care from an interdisciplinary team of professionals who provide all primary care services and oversee specialists’ services.
A Medicare-funded demonstration spanning 1979 to 1983 found this approach had many benefits. Care teams were able to prevent or quickly address problems, resulting in better health and quality of life and producing 15 percent lower costs than traditional Medicare. In the decades since, the model has spread slowly, though enrollment has grown nearly 40 percent in the past three years. As of January 2016, there were 118 PACE organizations in 31 states serving some 39,000 elders.2
Below we examine the PACE model of care, focusing on On Lok as the original program and exploring the potential for the model to be adapted and spread.
On Lok's Target Population

With 700 full- and part-time staff, On Lok serves more than 1,400 elders in seven PACE centers and in elders’ homes in the San Francisco Bay Area. Many are women with multiple chronic health conditions and some mental impairment, and many are in their last few years of life. They may need help with tasks such as getting dressed, bathing, eating, and taking medications.
About 90 percent of those enrolled in On Lok are “dual eligibles” — eligible for Medicare because of their age or permanent disability and eligible for Medicaid because of their low income. Many face socioeconomic challenges, such as having poor living conditions or little access to healthy foods, in addition to having complex medical conditions. To recruit participants, On Lok targets its outreach efforts to family caregivers as well as to discharge planners at hospitals and rehab facilities.
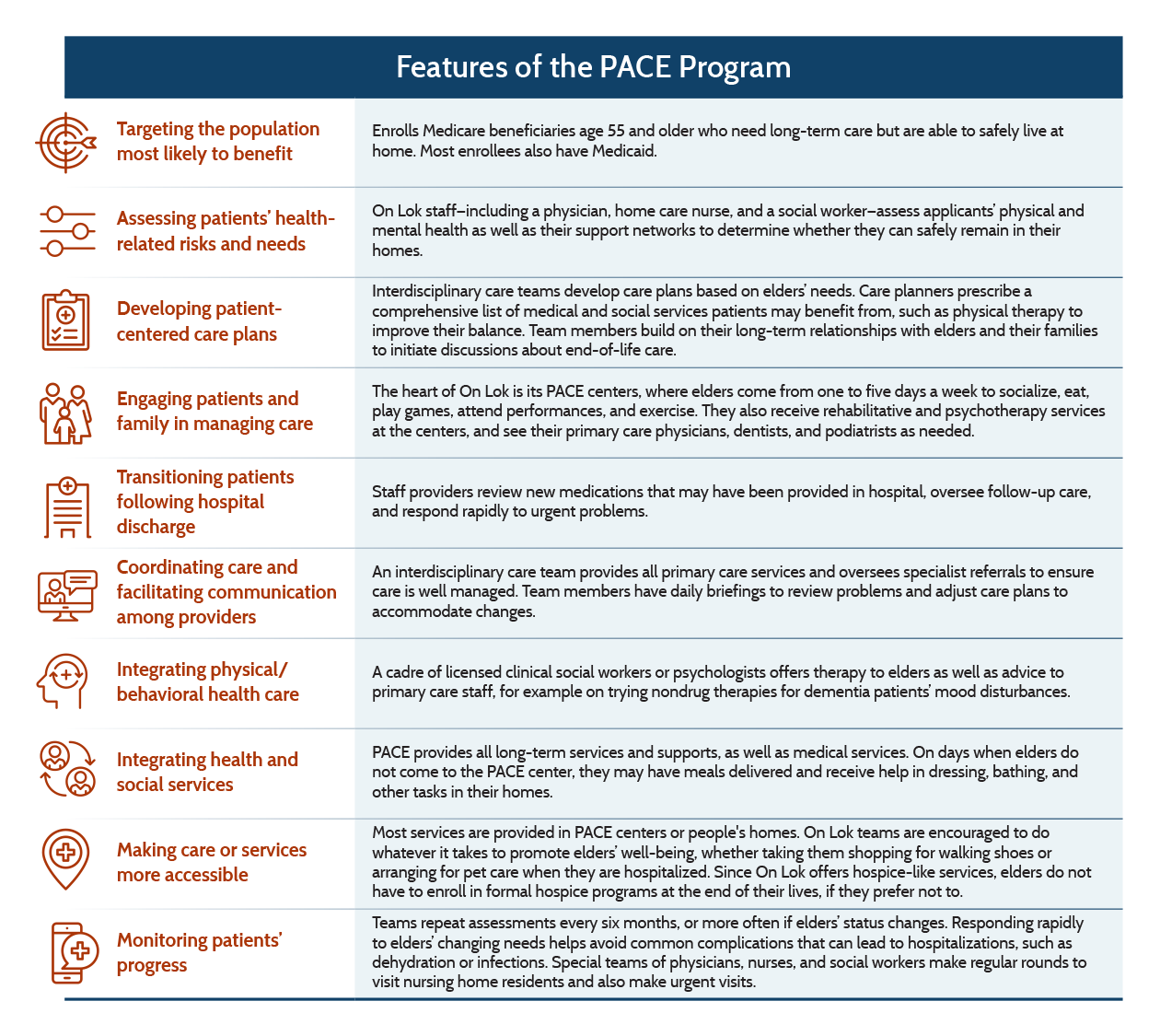
PACE is designed for those who need long-term care and are certified as eligible for nursing home care. In addition, PACE enrollees must be able to live safely at home at the point of enrollment. As part of the enrollment process, On Lok staff, including a physician, home care nurse, and social worker, perform physical and mental health exams on applicants to make a preliminary assessment of nursing home eligibility and determine whether they can safely remain in their homes. Based on their assessments, the state makes a final determination of nursing home eligibility and approve elders for enrollment.
Key Program Features
Comprehensive Medical and Social Services
There is nothing better than exercise for aging. It’s the single best intervention. It’s the best therapy for diabetes. It’s the best therapy to prevent falls. It’s the best from a cardiovascular standpoint. But probably most importantly, it’s the best for your mood.
Like other PACE organizations, On Lok provides a comprehensive range of medical and long-term services and supports. Many are provided at its day centers, where elders come from one to five days a week to socialize, eat, play games, attend performances, and exercise. They also receive rehabilitative and psychotherapy services at the centers and, as needed, see their primary care physicians, dentists, and podiatrists. Some elders are bathed and have their laundry done there as well. On days when elders do not come to the day centers, they may have meals delivered to their home, where they can also receive help with dressing, bathing, and other tasks.
In addition to providing most medical and support services, the centers are designed to keep elders’ minds and bodies active. Some On Lok elders begin exercising regularly, helping to ward off muscle deterioration and improve their mood. Other efforts aim to preserve functional health: podiatrists focus on simple tasks, like clipping nails, to make sure elders can walk, and dentists seek to preserve their gums and teeth so they can chew healthy foods. Games such as mah-jongg — a favorite among Chinese elders — offer exercise for the hands and mind. Bringing elders to day centers also provides respite to family caregivers.
Care Coordination by Interdisciplinary Teams
Interdisciplinary care teams develop care plans based on elders’ needs, beginning with a careful review of their housing and support network. Is their home safe? Or do they have thick rugs that pose a tripping hazard? Might their neighbors or family members be willing to check in on them? Care planners prescribe a comprehensive set of medical and social services patients may benefit from, such as physical therapy to improve their balance. Teams repeat the assessments every six months, or more often if elders’ health or emotional status changes.

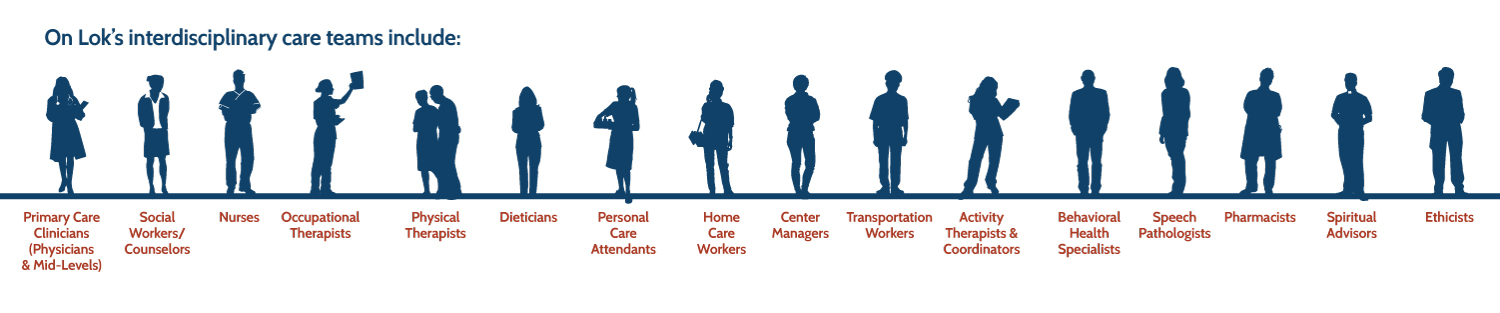
The teams, each of which is responsible for about 150 elders, include two primary care providers, nurses, behavioral health providers, occupational and physical therapists, dieticians, activity therapists, and social workers, as well as personal care attendants and drivers. Notably, team members have daily briefings to review problems and adjust care plans to accommodate changes — for instance, increasing skin checks when a person becomes less mobile.
Carving out time for all team members to meet daily is difficult, but doing so helps to ensure that no warning signs are missed, says Jay Luxenberg, M.D., chief medical officer. “The first sign of a decline in function might be that the person had more trouble getting from their home down the stairs to the van,” he says. “The driver might clue you in to something that really could take weeks or months before the doctor would notice.” Teams also collaborate using a shared electronic health record.
Rather than having one person, such as a nurse care manager, lead the team, all members work together to develop consensus on care plans. Key decisions are made by whoever is best positioned to make them: primary care physicians advise elders and their families on such issues as whether to pursue cancer surgery, while physical therapists assess whether elders can remain safely in their homes after a fall. On Lok teams are encouraged to do whatever it takes to promote elders’ well-being. This might mean taking them shopping so they have good walking shoes or arranging for pet care when they need to be hospitalized.
On Lok’s primary care providers are core team members with dedicated time to consult with other staff or make visits to elders’ homes to respond to urgent problems. Responding rapidly to elders’ changing needs helps avoid common complications such as dehydration or infections that can lead to hospitalizations. And since On Lok providers oversee all specialist referrals, they are able to ensure care is well managed, for example by carefully reviewing all new prescriptions to avoid medication problems.
Integrated Care Through End of Life

Dementia has become a leading cause of debility among elders.3 In response to the shortage of geriatric psychiatrists willing to accept Medicare or Medicaid rates, On Lok has developed a behavioral health program that relies on a cadre of licensed clinical social workers or psychologists. These behavioral health providers offer therapy to elders as well as advice to primary care staff on dementia care, including nondrug therapies for patients’ mood disturbances. The focus, Luxenberg says, is on “fewer pills, more words.”
Elders can choose to remain enrolled in On Lok for life, even if they eventually need to move to nursing homes. Special teams of physicians, nurses, and social workers make regular rounds to visit nursing home residents and also make urgent visits. Team members build on their long-term relationships with elders and their families to initiate discussions about end-of-life care.
And since On Lok offers hospice-like services, elders do not have to enroll in formal hospice programs at the end of their lives if they prefer not to. More than half of On Lok’s elders die at home, rather than in a hospital or nursing home. Nationally, only 25 percent of Americans die at home — even though that’s what the vast majority say they’d prefer.4
Financing
After operating for its first decades under waivers, PACE became a permanent part of Medicare and an option for all state Medicaid programs through the Balanced Budget Act of 1997. On Lok and other PACE organizations operate as managed care plans, pooling the fixed monthly payments they get from Medicare and Medicaid to purchase an array of services for members — not just those that are reimbursable under these programs. They use Medicaid dollars to pay for nonmedical services.
PACE organizations take on full financial responsibility for the cost of all care provided by their staff and contracted providers, including hospital and nursing home care.
Results
On Lok
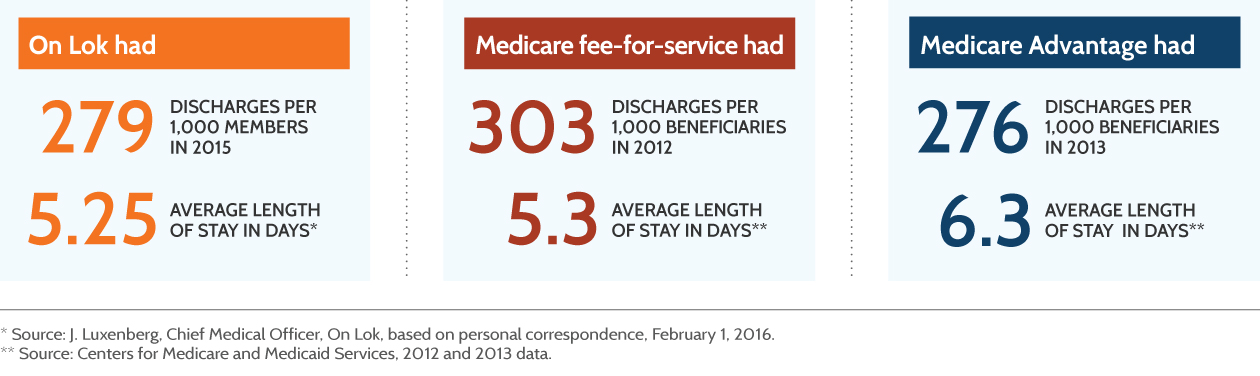
Although On Lok members are older and frailer than the Medicare population as a whole, they are hospitalized at similar rates to those in Medicare Advantage plans and less often than those in fee-for-service Medicare. The readmission rate within 30 days of hospital discharge for On Lok members is about half the average among other Medicare beneficiaries.5
Based on 2012 data, On Lok estimates that its members accrued lower costs during the last six months of life than other Medicare beneficiaries in San Francisco with one or more chronic conditions.6 California Medicaid pays On Lok and other PACE organizations in the state capitated payments for each PACE member that are set at 5 percent less than what the agency predicts it otherwise would have spent for a comparable nursing home–eligible population.
National PACE Results
A recent literature review found that PACE enrollees across the nation experienced fewer hospitalizations than their counterparts in fee-for-service Medicare.7 It found some evidence that PACE improved the quality of care, including better management of elders’ pain and lower mortality rates. PACE enrollees experienced more nursing home admissions, which may reflect the substitution of skilled nursing for hospital days (the studies reviewed did not distinguish between postacute care and long-term stays). A subsequent study (not included in the review) found that PACE may be more effective than Medicaid home and community-based waiver programs in reducing long-term nursing home use, especially for those with cognitive impairments.8
Overall, PACE appeared to be cost-neutral relative to Medicare. It may have increased costs for Medicaid, however, though more research is needed, the authors say, to account for current payment arrangements, which have evolved since the studies were conducted.
Nationally, nearly 93 percent of PACE elders say they would recommend the program to a friend or relative.9
Insights and Lessons Learned
I never thought that I would have to worry about who was going to feed my patient’s cat when I put the patient in the hospital…. You’ve got to love PACE for this. It’s truly all-inclusive but it’s incredibly complicated. There’re so many things that we really try to keep track of.
PACE is a complex undertaking that requires a relatively large, dedicated staff willing to accept responsibility for frail elders’ day-to-day needs. “You can’t do PACE without having strong medical leadership that can work in a community-based geriatric model,” says Eileen Kunz, chief of government affairs and compliance. Developing and sustaining PACE organizations also requires effective partnerships with state Medicaid leaders and support from the health care provider community.
The PACE experience may offer lessons for policymakers and health system leaders interested in promoting integrated care for high-need populations. For example, under the Centers for Medicare and Medicaid Services (CMS) Financial Alignment Initiative, some states are experimenting with ways to extend the PACE approach to care for greater numbers of those enrolled in both Medicaid and Medicare.10 In California, for example, the state Medicaid agency is partnering with CMS to contract with health plans (including On Lok) that provide medical, behavioral health, and long-term services to dual eligibles.11
The PACE experience in integrating care also may be of interest to health system leaders working under accountable care contracts that hold them financially responsible for designated patient populations. Leaders may learn from the PACE model to inform their efforts to identify high-need patients, including frail elders, and better serve them in ambulatory care settings to avoid costly complications and hospitalizations.
PACE faces competition from other programs and may face pressure from payers. There are more alternatives to nursing homes now than when On Lok began 40 years ago. Today, Medicaid waiver programs enable the provision of long-term care in home and community settings. In certain states, such as Virginia, PACE organizations are seeing competition from other home-care programs that allow family members to be hired as caregivers.
Many Medicaid agencies are increasingly turning to large managed care organizations to deliver services. Because PACE organizations are small and require more hands-on administration than typical managed care plans, they may be at a disadvantage as these agencies attempt to streamline program administration.
Medicare’s desire to share in the savings achieved by its providers could pose an additional threat to PACE, On Lok leaders say. “The origin of PACE is to put the health care dollars and the nursing home dollars in one bucket and then let the PACE team allocate those resources in the most logical way to achieve the mission of keeping people at home,” Luxenberg says. “We’ll see if that model ultimately breaks.”
The PACE model may need modification if it is to reach a larger share of the population. Federal legislation enacted in November 2015 gives program leaders the ability to pilot the PACE approach among other populations, including those with permanent disabilities or multiple chronic conditions.12 Some experiments have already begun. For example, St. Paul’s Senior Services of San Diego leveraged its PACE experience to develop a comprehensive postacute care offering for Medicaid managed care patients.13
To reduce costs and operational complexity, those adapting the PACE model will likely borrow some, but not all, of its features.14
Next Steps
The Mountain Empire PACE organization serving Dianna Boggs in rural Virginia was created as part of a federally supported effort to spread the model to rural communities, where elders tend to be sicker and may have fewer options for care than urban elders.15 It is but one example of the way in which PACE is enduring and evolving.
“Despite being 40 years old, it’s still a wonderful model,” Robert Edmondson, former CEO of On Lok, says. “What will improve it is a little more flexibility, a little broader reach, and maybe some influence of technology. But I’m sold on the model. If you visit a center, it’s what you’re going to want for your own family — there’s no question.”






