By Karen Davis
Health care reform issues—particularly how to achieve universal health insurance—were arguably more important to Americans in 2007 than ever before. A number of the 2008 presidential candidates, as well as federal and state lawmakers, presented detailed and workable health care plans, and leading states such as Massachusetts began to see their coverage efforts pay off. Yet, much work must be done in the coming year and beyond to build a high-performing health system. Below, we feature some of the top health policy stories of the year as well as Commonwealth Fund research and analysis that are helping to shape the debate about ways to stem rising health care costs, improve quality and efficiency, and provide comprehensive coverage for all.
1. Americans say health care is the leading domestic issue in the presidential campaign.
Health care is second only to Iraq as the issue that Americans most want the 2008 presidential candidates to talk about, according to the latest Kaiser Health Tracking Poll. Several candidates have responded to the public's interest with significant health care reform proposals. A report from the Commonwealth Fund Commission on a High Performance Health System released in November, An Ambitious Agenda for the Next President, commends these proposals and outlines the approach the Commission believes will improve health system performance. The report recommends five strategies: 1) extending comprehensive, affordable, and seamless insurance coverage to all; 2) aligning incentives to reward high-quality, efficient care; 3) organizing the health system to achieve accountable, coordinated care; 4) investing in public reporting, evidence-based medicine, and the information technology and infrastructure necessary to deliver the best care; and 5) exploring creation of a national entity that sets aims for health system performance and priorities for improvement, monitors performance, and recommends practices and policies needed to achieve a high performance health system.
2. The U.S. Census Bureau announces that the number of uninsured Americans rose by 2.2 million in 2006, to 47 million.
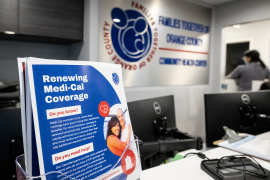
This increase of 2.2 million—a jump of 5 percent—is the largest one-year increase in the number of uninsured since 2002. The ranks of the uninsured have grown 8.6 million since 2000—an increase of 22 percent. In an effort to reverse this trend, state governments and members of Congress, as well as the presidential candidates, all advanced proposals this year to expand health insurance coverage to all Americans. The October Fund report A Roadmap to Health Insurance for All grouped the proposals into three approaches—and highlighted mixed private–public group insurance as the most pragmatic approach because it builds on the best features of our current system, with shared responsibility for financing from individuals, employers, and government. It also minimizes dislocation for the millions of Americans who currently have good coverage.
Massachusetts, which began implementing legislation that mandated insurance for all residents last year, is already demonstrating that private–public collaboration works. The governor's office recently announced that an estimated 290,000 residents have become newly insured through private insurance or though its subsidized or partially subsidized state programs.
3. Health care costs are expected to continue to rise unless policies to achieve savings are adopted.
The Centers for Medicare and Medicaid Service estimated this year that unless health reforms are enacted, total U.S. health care spending will rise to 20 percent of GDP by 2016, compared with 16 percent now. A new report from the Commission on a High Performance Health System, Bending the Curve: Options for Achieving Savings and Improving Value in U.S. Health Spending, outlines 15 federal policy options that have the potential to lower health spending relative to projected trends. These include options to produce and use better information; promote health and disease prevention; align incentives with quality and efficiency; and correct price signals in the health care market. The authors also estimated a savings of $1.5 trillion in national health expenditures over 10 years, based on a combination of selected options, along with the implementation of health insurance for all.
4. Studies continue to show that the United States spends more on health care than any other country, but its residents do not receive better care in exchange. Moreover, health care is less accessible in the U.S. because we are the only major country without universal coverage.
A Commonwealth Fund survey of primary care physicians and patients in five other nations—Australia, Canada, Germany, New Zealand, and the United Kingdom—finds that the U.S. health care system ranks last or next-to-last on five dimensions of a high performance health system: quality, access, efficiency, equity, and healthy lives. Much of this underperformance is attributable to the lack of universal health insurance in the U.S. Our failure to cover all Americans also underscores the findings of the 2007 Commonwealth Fund International Health Policy Survey, which found financial barriers are much more likely to prevent many U.S. adults from getting the care they need than adults in the six other participating countries. While no one country provided a perfect model of care, there are many lessons to be learned from the strategies at work abroad.
5. Medical homes can promote equity in care.
The latest Agency for Healthcare Research and Quality's disparities report, released in January 2007, found that that blacks received lower-quality care than whites on 73 percent of the quality measures it examined, and that Hispanics received lower-quality care than non-Hispanic whites for 77 percent of the measures. The report also revealed that low-income people received lower-quality care than high-income people for 71 percent of the measures. Similarly, The Commonwealth Fund 2006 Health Care Quality Survey found that Hispanics and African Americans have higher uninsured rates than whites, and are less likely to have access to a regular doctor or source of care. Our survey also pointed to an innovative way to reduce or even eliminate racial and ethnic disparities in access and quality. In addition to health insurance coverage, a medical home—defined as a health care setting that provides patients with timely, well-organized care as well as off-hours access—can help ensure vulnerable populations get the care they need when they need it. Medical homes are particularly good at providing chronic disease care and preventive services, and therefore can help manage or prevent costly medical problems. The authors of the survey report recommend support for community health centers and other public clinics in their efforts to build medical homes for all patients.
6. While many seniors have gained prescription drug coverage under Medicare Part D, seniors report high out-of-pocket costs that sometimes lead them to go without medication.
A survey of 16,000 seniors assessing the progress of the Medicare prescription drug benefit found that less than 10 percent of seniors lacked prescription coverage in the fall of 2006, and half of all seniors were enrolled in a Part D plan. By comparison, one-third of seniors said they had no drug coverage in 2005. However, the survey, which was supported by the Kaiser Family Foundation and The Commonwealth Fund, indicated that seniors in Part D plans were more likely to spend more than $300 per month on prescriptions than those in employer plans or with other sources of coverage, despite taking a similar or smaller number of medications. As a result, Part D enrollees were about twice as likely to skip their medications as were seniors with employer plans or Department of Veterans Affairs benefits. These findings point to the need to identify the reasons for high out-of-pocket spending, such as Medicare's coverage gap and its formularies.
Other research shows that low-income Medicare beneficiaries are still not being reached: while the subsidized drug benefit available to them could be helpful, almost half of the seniors who qualify are unaware of it.
7. A state scorecard finds wide variations in health care exist across states.
The Commonwealth Fund's first state scorecard found that health care quality, cost, and access vary widely across states, suggesting that where you live can make a big difference to your health. Other major findings were: leading states consistently outperform lagging states, indicating that federal and state policies and local and regional health systems make a difference; better access is closely associated with better quality; states have opportunities to simultaneously reduce costs and improve quality of care; and all states have substantial room to improve. The five top-ranked states, Hawaii, Iowa, New Hampshire, Vermont, and Maine, all have high rates of insurance coverage. Among the five lowest-ranking states, Nevada, Arkansas, Texas, Mississippi, and Oklahoma, uninsured rates for adults and children were well above the national average. Visit our interactive state map to see how your state ranked overall and by performance dimension.
8. Congress's bill expanding the State Children's Health Insurance Program was vetoed by the president and states now face shortfalls.
The State Children's Health Insurance Program (SCHIP), created a decade ago, expanded health insurance for low-income children through federal–state and public–private partnerships, and is widely considered a coverage success. Despite passing bills to reauthorize and expand SCHIP in September, Congress was not able to overturn President Bush's veto and 21 states now face shortages in their children's health insurance programs.
Currently, SCHIP covers about 6 million children whose families are low income but not poor enough to qualify for Medicaid. Democrats hoped to expand the program by $35 billion over five years, to $60 billion. CQ HealthBeat reported that the Bush Administration believed the bill went "'too far toward federalizing health care' and would open the program to families making as much as $83,000 a year, claims that advocates of the bill say are false." As of publication, it was reported that Congress was considering a short-term extension of the program.
9. The Centers for Medicare and Medicaid Services (CMS) proposes that Medicare pay hospitals based on performance.
CMS has proposed adding to an existing program that rewards hospitals that report quality data. The new "value-based purchasing program" would take the next step in payment reform by paying hospitals more Medicare money if they performed well on quality measures. As I've outlined in New England Journal of Medicine, and Milbank Quarterly articles, and in this column, our fee-for-service payment system is a barrier to effective, coordinated, and efficient care because it reimburses "inputs"—hospital stays, physician visits, and procedures—rather than the most appropriate care over an episode of illness or over the course of a year. As a large purchaser, Medicare can serve as a payment reform innovator by aligning financial incentives with health care quality and efficiency.
10. While the quality of care in nursing homes has improved, we can do more to improve life for older residents.
This year marked the 20-year anniversary of the Omnibus Budget Reconciliation Act (OBRA) of 1987, which included the first Nursing Home Reform Law. While the law strengthened residents' rights and set quality standards for care, nursing homes still face serious problems, including enforcement of standards, the nursing staff shortage, and limited availability of health information technology. Two recent Commonwealth Fund–supported articles addressed specific needs: empowering frontline workers to make decisions regarding patient care and creating objective measures consumers can use to evaluate nursing homes. The Commonwealth Fund continues to be a voice for culture change in nursing homes, to transform hospital-like environments to resident-centered homes and thereby enhance the satisfaction of residents, families, and staff.
As always, I'm interested in your feedback. Please e-mail me at [email protected].
Written with the assistance of Christine Haran.