Synopsis
To reduce health care spending growth and improve quality of care, Blue Cross Blue Shield of Massachusetts in 2009 introduced an alternative to fee-for-service provider reimbursement. Under the Alternative Quality Contract, as it’s called, providers receive a global budget for patient care, plus bonuses and incentives based on cost-savings and quality performance. An evaluation of spending and quality data from the first four years of the contract showed slower spending and improved quality relative to fee-for-service reimbursement.
The Issue
Paying providers for each individual visit, test, and procedure involved in treating their patients tends to promote overuse of services and impede the fair and efficient allocation of resources. That’s why Blue Cross Blue Shield of Massachusetts (BCBSMA) launched the Alternative Quality Contract (AQC) in 2009. Under this program, BCBSMA pays provider groups risk-adjusted budgets for the entire continuum of care. Providers share in the savings generated if spending comes in below the budget; if spending exceeds these budgets, providers share in the risk. BCBSMA also offers incentive payments based on performance on quality measures. In a recent Commonwealth Fund–supported study, researchers compared spending and quality data for patients of providers who signed on to the AQC with a control group of patients whose providers did not. The period under study was 2009–2012, the first four years of the five-year contract.
Key Findings
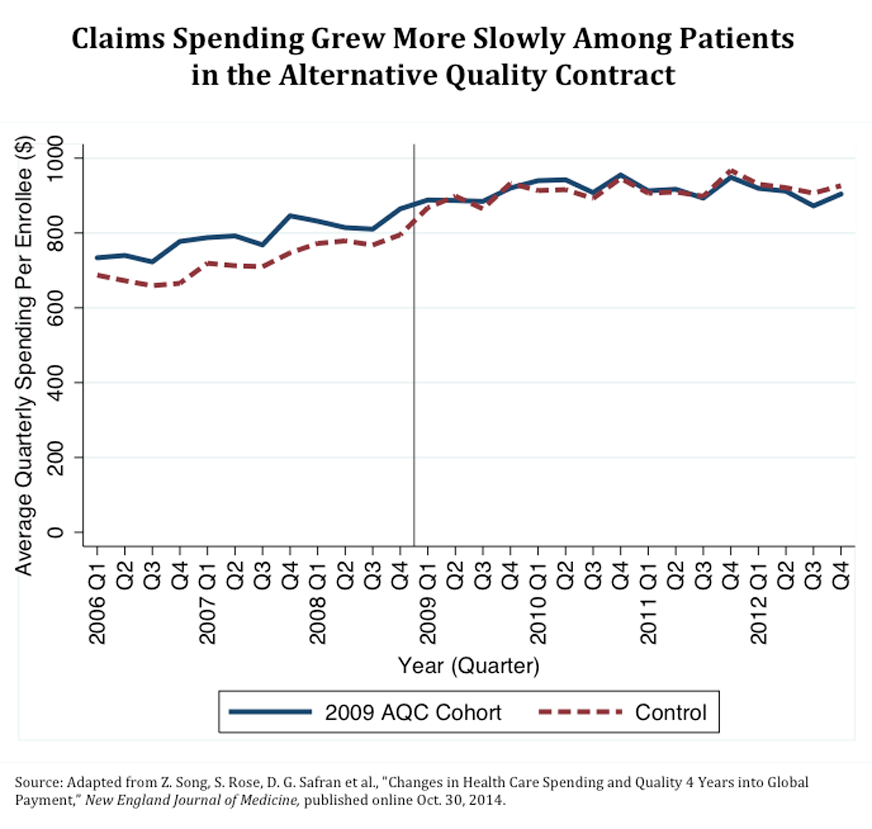
- Spending on health care claims grew more slowly—$62.21 less per enrollee per quarter—for the 2009 AQC cohort as compared with the control group. Savings averaged 6.8 percent.
- Savings were highest for procedures, imaging, and tests performed in the outpatient facility setting. Forty percent of the claims savings were attributable to lower volume of services; the other 60 percent were explained by lower prices, which included referring patients to less expensive providers.
- The AQC enrollees showed greater improvement on measures of chronic disease management, adult preventive care, pediatric care, and control of diabetes, cholesterol, and blood pressure.
- Although incentive payments from shared savings and quality bonuses exceeded claims savings during the first three years of the AQC contract, that trend reversed in 2012, leading to net savings and total payments that came in under budget.
The AQC experience may be useful to policymakers, insurers, and providers embarking on payment reform. Although it is still early, these results suggest that a two-sided global budget model may serve as a foundation for slowing spending and improving quality.
The Big Picture
The results suggest that a “two-sided” global budget model featuring shared savings and shared risk could help to slow spending and improve quality. “Changes in spending owing to lower prices or utilization suggest that new payment models may help modify underlying care patterns, a likely prerequisite for sustainable reform,” the authors conclude. Going forward, the relationship between payers and providers, they note, will be critical to the success of payment and delivery system reform.
About the Study
Researchers looked at claims payments and quality data for patients enrolled in Blue Cross Blue Shield of Massachusetts’s Alternative Quality Contract from 2009 to 2012 and compared them with data for patients with similar demographic characteristics and risk profiles in health plans that did not use global payment models or risk-sharing contracts. The researchers looked specifically at spending changes by year, category of service, and care setting. They also analyzed pricing and utilization patterns.
The Bottom Line
Although the model is still in its early stages, global budget contracts that include quality incentives and shared risk show promise to both slow spending and improve quality of care.



