 This is the third of four briefs in The Commonwealth Fund’s Medicare at 50 Years series that explore the key issues confronting the Medicare program and policy options for addressing them. The first brief discussed the potential of value-based payment to improve beneficiary care and achieve savings; the second outlined policy options for modernizing Medicare’s benefits and limiting costs for low-income beneficiaries. The last brief in the series will focus on care for complex patients.
This is the third of four briefs in The Commonwealth Fund’s Medicare at 50 Years series that explore the key issues confronting the Medicare program and policy options for addressing them. The first brief discussed the potential of value-based payment to improve beneficiary care and achieve savings; the second outlined policy options for modernizing Medicare’s benefits and limiting costs for low-income beneficiaries. The last brief in the series will focus on care for complex patients.
The Commonwealth Fund’s Medicare at 50 Years series is now available in its entirety for viewing and download as an e-book.
Abstract
The authors assess how Medicare financing and projections of future costs have changed since 2000. They also assess the impact of legislative reforms on the sources and levels of financing and compare cost forecasts made at different times. Although the aging U.S. population and rising health care costs are expected to increase the share of gross domestic product devoted to Medicare, changes made in the program over the past decade have helped stabilize Medicare’s financial outlook—even as benefits have been expanded. Long-term forecasting uncertainty should make policymakers and beneficiaries wary of dramatic changes to the program in the near term that are intended to alter its long-term forecast: the range of error associated with cost forecasts rises as the forecast window lengthens. Instead, policymakers should focus on the immediate policy window, taking steps to reduce the current burden of Medicare costs by containing spending today.
Introduction
Predictions about Medicare’s financial future are often pessimistic, sometimes to the extreme. As some would have it, the program’s future is a looming disaster toward which we are inexorably drawn by rising health care costs and the mass retirement of the baby boom generation.
Several observations suggest this dismal outlook is wrong. Changes in both policy and financial forecasts over the past 15 years provide reason for optimism about our nation’s ability to afford the Medicare program into the future. Legislative changes enacted since 2000, primarily through the Medicare Modernization Act (MMA) in 2003 and the Affordable Care Act (ACA) in 2010, have substantially altered both the level and composition of current and forecasted program financing. Moreover, new information concerning the nature and pace of technological change in health care has altered actuaries’ assessments of likely program costs for the near and long-term future. In fact, since 2003, the overall financial outlook for the program has improved considerably, even as the level of covered benefits has increased. More recently, there has been a marked slowdown in Medicare spending.
The ability to make significant programmatic changes in the short term—as demonstrated by the MMA and ACA—and the difficulty of forecasting costs over the long term suggest that policymaking can be most effective by addressing immediate needs.
This brief explores how the ACA and MMA have altered forecasts of future Medicare viability, details the limits of long-term forecasting, and reflects on the difficulty that tomorrow’s beneficiaries would have in determining their future needs and spending today.
Medicare Financing at a GlanceMedicare is financed through a payroll tax that accumulates in a trust fund whose balances pay for expenses under Part A (which covers inpatient hospital care), through premiums paid by Medicare beneficiaries who choose to participate in Parts B (physician services) and D (prescription drugs), and through general revenues. The Medicare trustees annually project future revenues and disbursements to ensure that Medicare trust fund balances are adequate to pay future costs; they also forecast total Medicare spending as a share of gross domestic product (GDP). |
New Policies and Paradigms: Why Medicare Forecasts Change Over Time
Forecasts evolve because of both policy changes and modifications to forecasting methods and assumptions. In 2003, the Medicare program’s trustees projected that the program (then consisting only of Parts A and B) would account for 4.7 percent of the nation’s GDP in 2030, and 8.5 percent of GDP by 2070.1 Since then, with the enactment of the MMA and the ACA, the Medicare program has changed substantially. These changes have had a significant impact on spending and are altering projections of future program costs as well as financing. The 2014 projections put Medicare costs, now including Part D, at 4.9 percent of GDP in 2030, and 6.6 percent in 2070.
By introducing income-related premiums for Medicare Part B, the MMA changed how the existing Medicare program is financed. It also created a new prescription drug insurance benefit (Part D), financed in part through premiums and in part through general revenues. At the outset, the income-related premiums for Part B affected only the top 5 percent of Medicare beneficiaries; the current thresholds start at about 735 percent of the federal poverty level (FPL). Medicare beneficiaries above the highest income threshold pay 80 percent of the average cost of Part B.2
The ACA expanded Medicare benefits by enhancing Part D drug benefits and by including Part B preventive care services with no cost-sharing.3 The ACA also adjusted reimbursement formulas for Medicare Part A, reducing payment growth to account for economy-wide productivity gains. Prior to the ACA, Medicare Advantage plans had received reimbursement at rates in excess of the cost of covering beneficiaries under the traditional fee-for-service program. The ACA reduced reimbursement rates for Medicare Advantage plans to eliminate these overpayments. The ACA also made a variety of other changes to Medicare spending.4
On the financing side, the ACA added an income-related Part D premium and froze the thresholds for the Part B and Part D income-related premiums from 2010 through 2019. By 2019, an estimated 9.6 percent of Medicare beneficiaries are expected to be subject to the high-income premiums.5 The ACA also raised payroll taxes for higher income beneficiaries. The 0.9 percent tax on high-income earners is expected to raise $123 billion between 2010 and 2019 for the Hospital Insurance Trust Fund.6
The reported short- and long-term outlook for the program also changed because of changes in forecast methods and assumptions. These changes occurred as actuaries projected the impact of the legislative changes described above; as they learned more about the performance of different aspects of the program; and as they altered their forecast methodology. Most significantly, in 2003 the Medicare trustees substantially altered their assumptions about long-term cost growth. Before 2003, the trustees projected health care cost growth would be equal to wage growth (GDP+0); the predicted rise in spending reflected only the change in the number of elderly per worker.7 A technical review panel convened in 2000, however, recommended that the long-term projection should assume that health care costs would grow 1 percent faster than GDP (GDP+1), and the trustees incorporated this recommendation beginning in the 2003 report.
Changes in Forecasts of the Level of Medicare Spending, 2000 to 2014
The effects of these changes in policy and forecasting assumptions are apparent in the shifting projections made in the trustees’ reports between 2000 and 2014 (Exhibit 1). (See Appendix A for an alternative 2014 projection and explanation.) 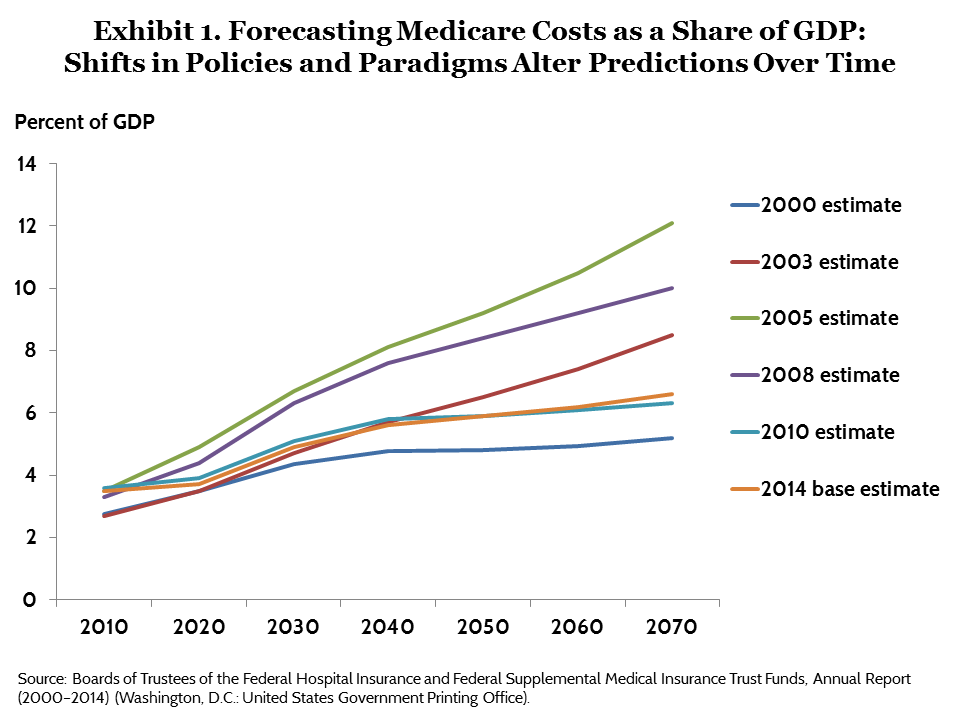
The first notable change in Exhibit 1—the shift between the 2000 trustees report estimate and the 2003 estimate for the period after 2025—occurred simply because of the change in the long-term growth assumption described above. This change alone suggested that by 2070 health care costs would consume 3.2 percent more of the GDP than was projected in 2000.
The second shift, between the 2003 and 2005 estimates, occurred because of the MMA. Part D added substantial costs to Medicare immediately, and the trustees projected that these high costs would grow rapidly in the near future. The new program was expected to add 2 percent to the GDP share of Medicare by 2030 and 3.6 percent to that share by 2070. However, the rate of new drug development slowed appreciably in the early 2000s and blockbuster drugs such as Zocor and Zoloft went off patent. These developments led the trustees to revise their projections. The 2008 estimate, incorporating more of the realized Part D experience, was more than 2 percentage points of GDP below the 2005 estimate at the end of the forecast period.
The effects of the ACA can be seen in a comparison of the 2008 and 2010 forecast estimates. The ACA had a significant short-term effect on the Medicare forecast, extending the projected trust fund depletion date by 12 years. It also had a large effect on the long-term forecast by permanently changing the formula for increasing hospital payment rates from year to year. These changes reduced by 3.7 percent the anticipated share of Medicare in GDP by 2070.
Very short-run changes in health spending also contributed to changes in the forecast. No significant Medicare legislation passed between 2010 and 2014, and the Medicare technical review panel did not alter the trustees’ long-term forecast projection. Instead, the 2014 estimate is about 0.2 percentage points of GDP below the 2010 estimates for 2030 and 2040 because of the unanticipated slowdown in health care spending that continues through today.
The current 25-year forecast for the total cost of Medicare as a share of GDP in 2040, after all the baby boomers have retired, is now just slightly below the level it was in 2003—before passage of the MMA and before the Great Recession. Put differently, faced with a deficit comparable to the one we see today, policymakers in 2003 assessed Medicare as a program ripe for expansion.
Changes in the Composition of Medicare Financing
The new policies and changes in assumptions described above also changed the expected composition of Medicare financing. Concerns currently focus on the program’s expected draw on general revenue, financed primarily through income taxes.
Exhibit 2 breaks out the trajectory of financing from each of three revenue sources: payroll taxes, premium income, and general revenue. According to all projections, the share of total Medicare expenditures financed through the payroll tax is expected to decline over time, and the absolute share of GDP collected through the payroll tax is expected to be nearly flat. 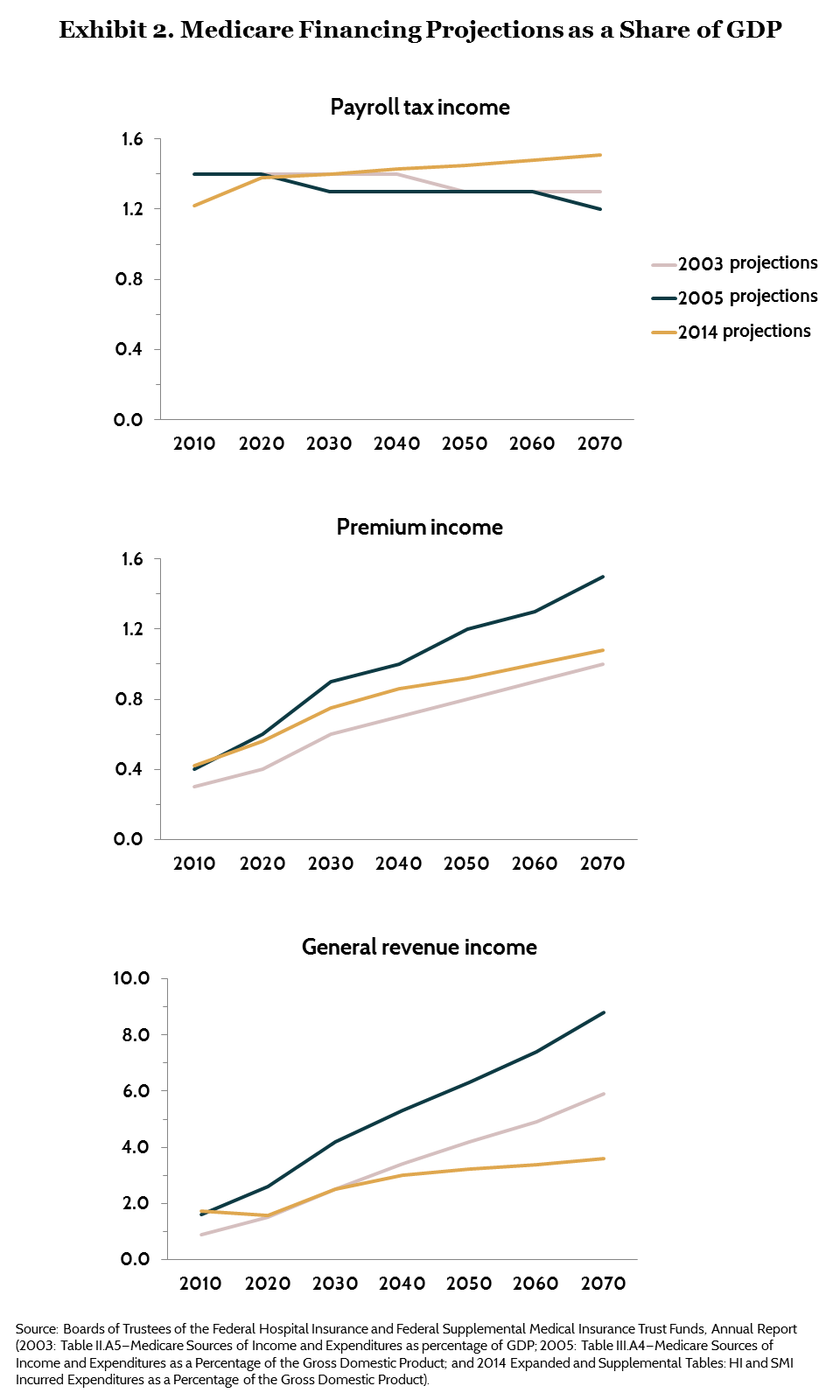
Premium income grows as a share of GDP as a direct consequence of the expected increase in the cost of the overall program. The share of Medicare spending financed through premium income increased after passage of the MMA and the ACA because of the introduction of income-related premiums. Current estimates suggest that premium income financing for Medicare will rise from about 0.4 percent of GDP in 2010 to about 1.0 percent of GDP by 2070.8 For all but high-income beneficiaries, premiums for Part B and Part D are intended to finance a fixed share (25%) of program expenditures. The thresholds for high-income premium payments are indexed after 2019, so the overall share of total expenditures financed through premiums is largely fixed over time.
The decline in estimates of the future cost of Medicare, however, has substantially reduced the expected call on general revenues in the future. Under the trustees’ baseline projections, the Medicare general revenue share of GDP is expected to double, from about 1.7 percent to about 3.6 percent of GDP between 2030 and 2070—less than half the level expected immediately after passage of the MMA. (The 2014 alternative projections are higher; see Appendix A for more information.)
Conclusion: Uncertainty Is Inherent in Medicare Policymaking
Predicting health care costs 20 or 30—let alone 50 or 75—years into the future is an inexact science, at best.9 The costs of providing care depend on future innovations in technology, the value of such innovations to beneficiaries and to taxpayers, and the supply of and demand for health care services. As the Part D experience and the recent cost slowdown suggest, projections of the rate of future technological change are hard to make even in the short run.
The aging of the baby boomers and rising health care costs will plausibly increase the share of GDP devoted to Medicare, but nothing is certain. As we have shown, changes made in the program over the past decade meant that despite substantial expansions of benefits, the financial outlook for the program remained quite stable. The experience of the past 15 years suggests that there is room for considerable optimism about the ability of our nation to afford the Medicare program into the future.
Long-term forecasting uncertainty should make policymakers and beneficiaries cautious about dramatic changes to the program in the near term. The range of error around forecasts of Medicare costs rises as the forecast window lengthens. This suggests that policymakers should focus on the immediate policy window, taking steps to reduce the current burden of Medicare costs by containing spending today. Medicare expenditure policy changes, such as changes in payment rates or methods, can and have taken effect very quickly. Similarly, revenue changes to pay these expenditures occur in real time. Future policymakers are likely to have as much opportunity and much more information than current policymakers to make optimal decisions about Medicare’s future costs.
The challenges of forecasting Medicare costs provide an additional rationale for paying retiree costs through social insurance rather than a defined-contribution system.10 Individuals simply cannot anticipate what health care is likely to cost after they retire, and they cannot know how much to save against the prospect of these costs. If talented professional actuaries have difficulty making forecasts, then individuals will surely struggle to project what services they will need in the future. As a society, we can decide through the political process to alter policy or payment practices—and we have done so in the past—but such alterations are well beyond the power of any beneficiary.
How This Study Was ConductedThis analysis uses the 2000, 2003, 2005, 2008, 2010, and 2014 annual reports of the Boards of Trustees for Medicare to assess how the financing of Medicare and projections of the program’s future costs have changed over time.11 It assesses the impact of legislative changes on the sources and levels of financing of the program and compares projections of the future costs and financing of the program made at different times to evaluate how both funding and forecasts have changed. In keeping with the treatment of this issue in the trustees’ reports, we assume that when the trust fund expiration date occurs, Medicare Part A spending that cannot be paid from trust fund revenues will be funded through general revenue. Thus, projected trust fund deficits, in years beyond 2012 in the 2003 report and in years beyond 2030 in 2014, were added to the general revenue financing bill. Our projections use the trustees’ official baseline, which assumed that the sustainable growth rate payment system for physicians would be overridden and that physician payments would increase at a rate of 0.6 percent from 2016 through 2023. It also assumes that the Medicare hospital payment system’s productivity adjustments, enacted through the ACA, will continue to be upheld into the future. The trustees also provide an alternative scenario, which we discuss in Appendix A. |
Appendix A. An Alternative 2014 Cost Projection
In recent years, the Medicare trustees’ reports have included several alternative projections. The 2014 report included three sets of projections: current law projections, baseline projections that assumed that the sustainable growth rate (SGR) would be overridden, and a set of alternative projections that assumed the revised hospital payment updates phase out beginning in 2019. This brief reports results for the baseline projections.
Some evidence suggests that even the baseline projections may be too pessimistic. The Committee for a Responsible Federal Budget, for example, has shown that 98 percent of the overrides of the SGR between 2004 and 2014 were offset by other reductions in Medicare spending (Committee for a Responsible Federal Budget, blog post, March 13, 2014). The final “doc fix” bill passed this year will offset only a third of the cost of the fix through other Medicare changes (Committee for a Responsible Federal Budget, blog post, March 25, 2015), but this offset is not incorporated in the baseline scenario.
The alternative scenario assumption that the productivity adjustments will not be sustainable is based primarily on the argument that these adjustments will lead to a substantial deviation between Medicare payment rates and private insurer payment rates. Recent research, however, suggests that private payment rates are more likely to imitate Medicare rates than to deviate from them.12
Exhibit A-1 below includes the alternative scenario estimates in our assessment of Medicare forecasts over time. Even under the alternative scenario, 2014 Medicare long-term projections are below those made in 2003, 2005, or 2008. At the height of baby boomer retirement, in 2040, total Medicare expenditures under the alternative scenario would reach 6.09 percent of GDP, about 60 percent above their 2020 level. 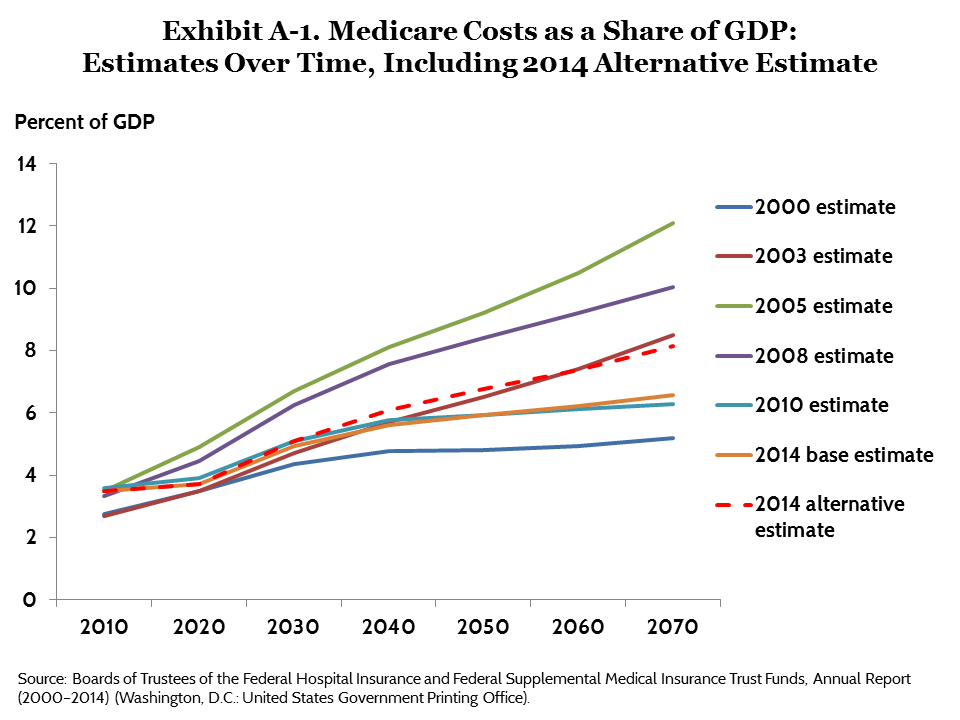
Notes
1 M. Moon, M. Segal, and R. Weiss, “A Moving Target: Financing Medicare for the Future,” Inquiry, Winter 2000–01 37(4):338–47.2 J. Cubanski, T. Neuman, G. Jacobson et al., Raising Medicare Premiums for Higher-Income Beneficiaries: Assessing the Implications (Washington, D.C.: Urban Institute, 2014).
3 K. Davis, S. Guterman, and F. Bandeali, The Affordable Care Act and Medicare: How the Law Is Changing the Program and the Challenges That Remain (New York: The Commonwealth Fund, June 2015).
4 Congressional Budget Office, Congressional Budget Office cost estimate: H.R. 4872: The Reconciliation Act of 2010 (Final Health Care Legislation) (Washington D.C.: CBO, 2010).
5 Cubanski, Neuman, Jacobson et al., Raising Medicare Premiums, 2014.
6 P. A. Davis, J. Hahn, P. C. Morgan et al., Medicare Provisions in PPACA (P.L. 111-148): R41196, Congressional Research Service Report for Congress (April 21, 2010):1–89.
7 G. S. Wunderlich, Improving Health Care Cost Projections for the Medicare Population:: Summary of a Workshop (Washington, D.C.: National Academies Press, 2010).
8 State transfers and taxes on benefits will add a further 0.4 percent of GDP by 2070 (0.6% of GDP under the alternative scenario; see Appendix A).
9 K. Davis, “Shaping the Future of Medicare,” Health Services Research, April 1999 34(1 Pt 2):295–306.
10 D. Shaviro, Who Should Pay for Medicare? (Chicago, Ill.: University of Chicago Press, 2004); and D. Shaviro, “Should Social Security and Medicare Be More Market-Based?” Elder Law Journal, 2013 21:87–148.
11 Boards of Trustees of the Federal Hospital Insurance and Federal Supplemental Medical Insurance Trust Funds, Annual Report (2000–2014) (Washington, D.C.: United States Government Printing Office).
12 J. Clemens and J. D. Gottlieb, Bargaining in the Shadow of a Giant: Medicare’s Influence on Private Payment Systems, working paper (National Bureau of Economic Research, 2013).



