Synopsis
Hospitals serving larger proportions of Medicaid and uninsured patients than other hospitals were found to have significantly higher “failure-to-rescue” rates for surgical patients experiencing postoperative complications. This disparity in mortality could not be explained by hospitals’ differing access to sophisticated clinical technology or other resources.
The Issue
The “failure-to-rescue” indicator is increasingly being used to assess the quality of hospital care. For their Commonwealth Fund–supported study, researchers explored the relationship between failure-to-rescue rates and hospitals’ safety-net burden, which they define as the proportion of patients who are insured by Medicaid or uninsured. The study also examined whether the availability of certain clinical resources, like registered nurses and advanced technology, affected the relationship between hospitals’ safety-net burden and their failure-to-rescue rates.
Key Findings
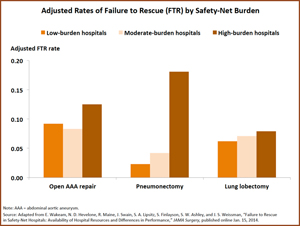
- Hospitals with a high safety-net burden had significantly higher odds of failing to rescue patients with postoperative complications, compared with low-burden hospitals. This held true even after adjusting for the availability of clinical resources and patient demographics.
- Patients in hospitals with high safety-net burdens were younger, more likely to be black, and less likely to undergo an elective procedure, compared with those in low-burden hospitals.
- High-burden hospitals were more likely to be large teaching facilities and to have high levels of “high hospital technology” (defined here as solid-organ transplantation and cardiac surgery), sophisticated internal medicine resources, and high ratios of respiratory therapists to beds. Yet compared with low-burden hospitals, these facilities had lower proportions of registered nurses and were less likely to have a PET scanner and a fully implemented electronic medical record.
Addressing the Problem
This study found significant variation in surgical safety at hospitals with high, moderate, and low proportions of safety-net patients. Though this variation does not appear to relate to hospitals’ access to clinical resources, it may be affected by differences in work culture, operational approach, or other factors. With the expansion of Medicaid under the Affordable Care Act, safety-net hospitals will play an even greater role in providing access to care to low-income and other vulnerable patients. It may be important, the authors say, for safety-net facilities to focus on failure-to-rescue rates in their benchmarking and quality improvement activities.
About the Study
The study classified hospitals’ safety-net burden by the proportion of Medicaid or uninsured patients they serve, dividing them into three categories: those with low burdens (bottom quartile), moderate burdens (middle two quartiles), and high burdens (top quartile). Using data from the Nationwide Inpatient Sample, the researchers calculated complication rates for 163,963 patients who had undergone one of eight high-risk surgeries. They used American Hospital Association survey data to assess whether hospitals had 14 different types of clinical resources, such as advanced cardiology and endoscopy tools, which may affect their ability to rescue patients in distress.
The Bottom Line
For reasons that are unclear, hospitals with large proportions of Medicaid and uninsured patients appear to have higher mortality rates among surgical patients experiencing postoperative complications, compared with facilities with low proportions of such patients.


