By Brian Schilling
In just the past three years, the more than 26,000 employees of Kraft Foods Group have become, behaviorally speaking, an almost entirely different group of people.
"In 2010, we set out to make our employees healthier and improve productivity by giving them incentives to get more engaged in their own health care," explains Kathy McAlpine, Kraft's senior director of benefits. "It's too early to declare victory, but so far so good."
That may be an understatement.
Kraft's medical spending trend dropped from an annual 8 percent increase in 2009 to a 1.2 percent increase in 2012, compared with a 3.9 percent increase nationwide. The percentage of employees completing health risk assessments (HRAs) jumped from 39 percent to 99.5 percent over the same period. Participation in chronic disease management programs has skyrocketed. The number of workers who report working at less than full capacity because of illness—a phenomenon known as presenteeism—is down.
Behind the Numbers
Kraft's success in encouraging beneficiaries to get involved in their care is the result of several factors, including smart benefit design and appropriate use of incentives and penalties. But one factor has played a particularly important role: the company's decision to emphasize customer service in its choice of health plans, Aetna One.
"The idea that we wanted a health vendor that could offer targeted, timely outreach to our employees and their families was really central to our benefits redesign effort," said McAlpine. "We started with the idea that it was our job to help our employees use and take advantage of their benefits. That's what made Aetna One and their health concierges so attractive to us."
Aetna One is an Aetna product that pairs designated "health concierges" with particular employers and employees. Health concierges are like high-powered customer service agents, but with a lot more training, access to more data, and no obligations to field a certain number of calls per hour. Typically, they have a small, dedicated group of companies from which they are expected to field calls. This allows health concierges to know each caller's copays, deductibles, referral requirements, support services, and other benefits details exhaustively.
To understand how they add value, consider the experience of one (non-Kraft) caller: Late last year, Angela Lupton, an employee at Aetna's customer service center in New Albany, Ohio, took an atypical call from an Aetna member.
"She was an older woman in her 90s and she was distressed about a bill," explained Lupton. What made the call unusual was that the bill didn't come from Aetna and it was for services rendered almost a decade earlier. "She didn't know if she needed to pay it and wasn't really in a position to find out."
What happened next is even more unusual; Lupton asked the woman for details, researched the services in question, followed up with the appropriate parties at the nursing home that generated the bill, coordinated with the collection agency that had become involved, and resolved the issue. Happily, too—the bill was a mix-up and the woman didn't have to pay.
"I'll typically understand callers' benefits as well as or better than they do and that allows me to help them make the most of their coverage," says Lupton. Lupton also works closely with a dedicated team of specialists to help match callers with needed services, so if, for instance, she receives a call from someone asking about a new diabetes test, she can talk to the caller about available diabetes support and also refer her to the appropriate professional, often by name.
Why Putting Service First Matters
Kraft's redesign effort may sound familiar to other large employers that have similarly been hit hard over the past 10 years by rising health care costs. The overhaul included:
- a mandatory high-deductible health plan;
- a health savings account;
- a four-tier prescription drug benefit program;
- steep surcharges for nonparticipation in key health management programs; and
- incentives of up to $500 per employee per year for taking steps to manage and improve their health.
These strategies—while somewhat controversial—are popular: 69 percent of U.S. employers offer a high-deductible health plan, 87 percent include a tiered formulary, and savings accounts, incentives, and penalties are all fast becoming de rigueur. But at Kraft, the emphasis on services makes all the difference.
"It's one thing to revamp your health benefits so that employees have a strong financial incentive to get involved in managing their own health," said McAlpine, who helped develop the organization's benefits overhaul. "But financial incentives only go so far. They certainly don't turn an employee who is confused about her health benefits into one who understands them overnight. Our employees aren't experts at navigating the health care system and we don't expect them to be. We viewed it as our job to help them."
And help they do. Of the steady stream of calls that come from Kraft employees on a weekly basis, 97 percent are resolved during that first call. Of the remaining 3 percent, the majority are resolved within a day or two. And overall, members are very happy with their service—nearly 96 percent say they're happy with Aetna's customer service.
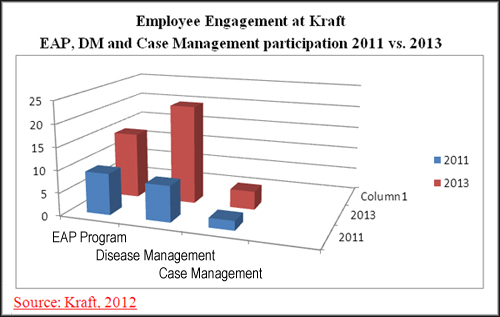
McAlpine says that great customer service has helped Kraft's benefits redesign achieve its three main goals: improve health, raise productivity, and control costs. The projected increase in Kraft's medical spending dropped by about 85 percent to 1.2 percent per year. Health risk assessment (HRA) participation is nearly universal at 99.5 percent. And participation in chronic disease management programs among the sickest employees has gone up nearly 450 percent. As a result, says McAlpine, Kraft's employees are healthier. Health risk scores in all categories have shifted from high risk to low risk, meaning it's less likely in the coming year they'll have significant medical problems.
|
Improved Productivity Percent of Kraft Employees Reporting Various Levels of Impairment, 2009-2011 |
||
| Level of Impairment | 2009 | 2011 |
| None | 71 | 77 |
| Slight | 23 | 18 |
| Mild | 4 | 4 |
| Moderate | 1 | .5 |
| Severe | 1 | .5 |
| Source: Kraft, 2012. |
| Increased Engagement in Disease Management Number of Kraft Employees with One of Five Specific Conditions* Engaged with a Nurse Via a Related Case Management Program |
||
| 2010 | 2011 | |
| Number of employees |
339 |
1,518 |
| *Asthma, chronic obstructive pulmonary disease, congestive heart failure, coronary artery disease, and diabetes. Source: Kraft, 2012. |
| Lower Health Risk Levels Percent of Kraft Employees at Various Health Risk Levels, 2009 vs. 2011 |
||
| Overall risk level | 2009 | 2011 |
| Very high | 3% | 2% |
| High | 69% | 64% |
| Moderate | 26% | 31% |
| Low | 2% | 3% |
| Source: Kraft, 2012. |
Kraft's redesign effort was recognized recently by NBCH and the Integrated Benefits Institute, which together awarded it the 2013 Healthy Workforce Productivity Award. This annual award goes to an employer that has successfully worked with its employees to develop, implement, and measure a notable health and productivity initiative.
"What really stands out with respect to Kraft's effort is the drop in health-risk factors among their employees," said NBCH President Andrew Webber. "To me that's much more notable than the drop in health spending. When you reduce health risks, you've done your employees and your organization some good in a way that will pay dividends for a long time."
The drop in health risks is no simple byproduct of a more enlightened benefit design. It's the direct result of a concerted effort to engage Kraft employees in their own health care. On the front lines of that effort are the health concierges, who are trained to steer people toward an array of typically underused health plan resources.
Health concierges are trained to talk, at length and intelligently, about available disease management resources, maternity programs, lifestyle coaches, smoking cessation opportunities, and other resources available to the employees of the companies.
"If I get a call from someone asking about a particular type of blood sugar test, my goal isn't just to answer that one question," says Aetna's Lupton. "That's the entry point for a conversation about diabetes, lifestyle coaching, and disease management resources. I ultimately want to be able to refer that caller to someone who can help them make sure they're staying on top of whatever health issue they're dealing with."
To date, Aetna's health concierges have given more than 13,000 such referrals to Kraft employees. Under a more typical customer service arrangement, none of those referrals would have been made unless the caller specifically requested it.
"For us, the concierges make the difference between having a great benefits program and having a great benefits program that actually gets used the way we want it to be used," said McAlpine. "Our benefits programs do not suffer from lack of use."
Sidebar: Benefits Redesign Rationale
High-deductible plans. By the end of this year, nearly 80 percent of employers with more than 1,000 employees are expected to offer a high-deductible plan. But perhaps more tellingly, almost 15 percent of those employers offer only a high-deductible plan. Note that a RAND study found that when families shift into high-deductible plans, their health spending dropped—but so did their consumption of preventive health care. Employers should seek to ensure that workers don't scrimp on valuable and cost-effective preventive care such as immunizations, screening for hypertension and colorectal and breast cancer, counseling adults about using baby aspirin to prevent cardiovascular disease, and screening pregnant women for HIV.
Tiered forumulary. Eighty-seven percent of employer health plans include some sort of drug benefit formulary. These formularies typically increase employee cost-sharing for more expensive or less effective drugs. Four-tier formularies are gaining market share. Today, about 14 percent of workers have such a formulary. To help guide beneficiaries to less expensive or more effective drugs, the average copayment is now $51 for so called "nonpreferred" third-tier drugs. The average coinsurance rate for the same tier: 39 percent.
Health savings accounts. As of last year, 17 percent of U.S. workers with employer-based insurance were enrolled in a health savings account (HSA), according to the Kaiser Family Foundation. A separate Kaiser study from the same year found that among individuals contributing to their own HSAs, costs substantially affected the care they chose—discouraging the use of costly emergency rooms and encouraging less expensive office visits.
Incentives and penalties. While incentives are still more popular than penalties for shaping health-related behaviors, employers are increasingly willing to use both, according to a 2012 Towers Watson survey of large employers. Forty-three percent of employers provide incentives to encourage participation in biometric screenings and 30 percent offer incentives to engage in healthy lifestyle activities in the workplace. By contrast, only 20 percent of employers use penalties to help shape behavior. But when it comes to smoking, the gloves are off: 42 percent of companies levy an average $50 per month premium penalty on tobacco users. About 10 percent of employers have adopted achievement standards related to metrics such as body mass or blood pressure.


