Primary and preventive care are important for improving and maintaining health, as well as reducing health care costs in the long term. Having health insurance—whether private or public coverage—is a "ticket" for entering the health care system, but by itself does not ensure access to timely and appropriate care. And the safety net clinics and health centers that serve people without coverage struggle to meet demand.
Hampering access to care is a shortage of primary care physicians, nurses, dentists, and other health personnel, particularly in low-income urban and rural communities. There are inadequate numbers of certain types of practitioners, as well as a maldistribution of practitioners—that is, insufficient numbers living and working in isolated geographic areas and/or willing and appropriately trained to serve culturally diverse low-income Medicaid beneficiaries and uninsured individuals.
This issue of States in Action focuses on federal and state efforts to enhance access to basic care. We describe a range of strategies available to states, largely involving efforts to expand and leverage the primary care workforce and to develop and test new models of care delivery.
Workforce Shortages and Other Barriers to Access
Tens of millions of people are living in areas of the U.S. with insufficient basic care, as the nursing and primary care physician shortages grow:1
- About 65 million people live in regions without adequate primary care, designated by the federal government as Primary Care Health Professional Shortage Areas (HPSAs). According to the Health Resources and Services Administration (HRSA), 16,643 additional primary care providers—more than a 4 percent increase over the current number—would be required to meet the need in the 6,204 primary care HPSAs, based on a population-to-practitioner ratio of 2,000:1. This need would not be met even if all medical school graduates in 2008 had become primary care providers.
- About 49 million people live in areas with shortages of basic dental care. 9,642 additional dental providers would be required to meet the need in the 4,230 dental HPSAs, based on a population-to-practitioner ratio of 3,000:1. This need is the equivalent of 4.1 percent of the 233,104 dentists practicing nationally in 2008.
- About 80 million people live in areas with shortages of mental health care. 5,338 additional mental health providers would be required to meet the need in 3,201 mental health HPSAs, based on a population-to-practitioner ratio of 10,000:1. This is the equivalent of about five times the number of graduating medical students who were matched to psychiatry programs in 2009.
A report by the National Association of Community Health Centers found that 56 million Americans have inadequate access to a primary care physician and could be considered "medically disenfranchised," out of the even larger number of people who are considered medically underserved because they live in shortage areas or face financial, linguistic, or other challenges to accessing primary care.2
Further, there is an estimated shortfall of over 400,000 nurses, projected to grow to 1 million nurses by 2020.3 Last year, about 50,000 qualified applicants to nursing programs were turned away, primarily due to lack of qualified faculty and clinical training sites. An aging nursing workforce and attrition also contribute to this shortage.
The number of medical school graduates choosing primary care disciplines such as family practice, internal medicine, and pediatrics has been declining sharply, as the income gap between primary care physicians and specialists—related to wide disparities in reimbursement rates under both public and private coverage—continues to grow. The U.S. physician workforce has a larger proportion of specialists than in many other countries, with 65 to 70 percent of physicians specializing according to some estimates (though some specialists spend part of their time providing primary care). Less than 50 percent of the physicians in Canada, the United Kingdom, and New Zealand are specialists. Cross-national patient surveys find that Americans are less likely than Canadians, Britons, and New Zealanders to have a regular doctor or place of care.4
In addition to barriers to access related to workforce shortages, many people face economic, cultural, or language barriers to care. The causes and consequences of such barriers are too complex to address here. To learn about them, see Racial and Ethnic Disparities in U.S. Health Care: A Chartbook and Improving Quality and Achieving Equity: The Role of Cultural Competence in Reducing Racial and Ethnic Disparities in Health Care.
Federal Efforts to Improve Access to Primary Care
There are many federal programs dedicated to reducing barriers to care. HRSA's Bureau of Health Professions, for example, addresses workforce shortages and insufficient diversity in the health workforce by identifying areas of need and administering a variety of grants and other funding for health professional education and training. HRSA's Bureau of Primary Health Care provides funding and technical assistance to federally qualified health centers, which provide care to uninsured, low-income, and underserved populations. Table 1 lists federal programs that benefit health care workforce shortage areas.
The American Recovery and Reinvestment Act, also known as the stimulus plan, signed into law February 17, 2009, provides significant funds to supplement prior efforts to combat barriers to health care access, generate new health care jobs, and meet the primary care needs of the growing uninsured and Medicaid populations. About $200 million was allocated to help train health care professionals through grants, scholarships, loans, and loan repayments.5 An additional $300 million was allocated to expand the National Health Service Corps, providing scholarships and loan repayments for students and practitioners who agree to practice primary care in shortage areas. The number of National Health Service Corps practitioners is expected to double to more than 8,000 by 2011.6
Table 1. Federal Programs that Benefit Shortage Areas
Health Center Program – administers grants and technical assistance to health centers serving primarily uninsured and low-income, publicly insured patients
Rural Health Clinic Program – provides cost-based reimbursement from Medicare and Medicaid to rural health clinics
Medicare HPSA Bonus Payment – offers extra payments to physicians who serve in primary care HPSAs and to psychiatrists serving in mental health HPSAs
National Health Service Corps Loan Repayment and Scholarship Programs – provide scholarships and educational loan repayment to primary care health professionals and students training to become primary care physicians, dentists, nurse practitioners, certified nurse-midwives, or physician assistants who practice in underserved areas7
Indian Health Service Scholarship Program – offers students of American Indian or Alaska Native background scholarships for training in health professions and allied health professions in exchange for service obligations
Exchange Visitor Program – waives the two-year foreign residency requirement for foreign physicians with J-1 visas in exchange for working for three years in a primary care or mental health HPSA
Conrad State 30 Program – allows states 30 J-1 visa waivers for foreign physicians each year in exchange for service in a shortage area
Source: HSRA, http://bhpr.hrsa.gov/shortage/, accessed February 2010
The American Recovery and Reinvestment Act also provided $2 billion for grants to health centers to expand their capacity to provide primary and preventive health services to medically underserved populations, and to meet an increased demand resulting from job losses and other effects of the recession. The Increased Demand for Services initiative (about $340 million), for example, is funding health center efforts to expand access through hiring new providers, extending hours of operation, and increasing the types of services offered. The Facility Investment Program ($515 million) and Capital Improvement Program ($850 million) are funding the costs of health center construction, renovation, and equipment, including information technology such as electronic health records.
The federal government also contributes to health care workforce development through payments to teaching hospitals for costs associated with training physicians in residency programs. These payments from Medicare and Medicaid total about $12 billion per year.
State Strategies to Address Workforce Shortages
Many analysts view the current HRSA and other federal programs to expand and redistribute the primary care workforce as helpful but inadequate. According to one analysis, such efforts are not enough to "counter overwhelming market incentives toward lucrative and highly specialized services—mostly in metropolitan areas."8 While there are a substantial number of new and planned medical schools, as well as increases in class sizes at some existing schools, these expansions alone are not likely to change the proportion of primary care providers in the physician workforce. Major payment reforms and changes in current federal subsidies in training and education may be necessary. But there are also efforts under way at the state level to improve access to primary and preventive medical and dental care. Indeed, there are many ways in which states can help increase the supply of primary care clinicians or leverage existing providers. States can supplement and build on federal incentive programs, or take the lead and test new approaches, potentially paving the way for expansion at the federal level.
Scope of Practice
Scope of practice laws, which detail the services that health professionals are allowed to offer and the settings in which they can practice, are largely determined by state governments. As a result, there is wide variation among scope of practice laws across states, particularly for mid-level practitioners such as nurse practitioners, physician assistants, emergency medical technicians, and dental health workers. Some states strictly limit the services and settings for these professions, while others allow broad latitude, thereby increasing the pool of practitioners9 able to provide basic medical and dental services. Training and qualifying mid-level practitioners to conduct some basic services traditionally performed by physicians and dentists—especially in rural and shortage areas and in public programs—can improve access to care and reduce costs.
While state legislatures can change scope of practice laws, state nursing and medical boards also have rule-making authority over scope of practice, such as defining training and certification requirements.
Virtually all states have used scope of practice laws to define and/or expand the role of nurse practitioners. About 147,295 nurse practitioners are serving patients in the U.S., with varying capacities in different states (Figure 1).10 In addition, as described in a Snapshot in this issue, Alaska and Minnesota promote the use of "dental therapists" to help meet basic dental needs in isolated areas, address workforce shortages, and reduce costs.
Figure 1. Nurse Practitioner Scopes of Practice
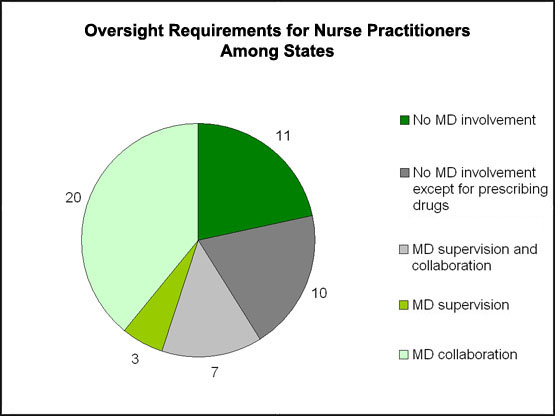
Note: Totals sum to 51 (50 states and the District of Columbia). States use varying definitions of collaboration and supervision, but supervision generally involves direct or indirect physician oversight of the services provided by nurse practitioners, while collaboration means that nurses and physicians plan and practice together in an interdependent way.11
Source: S. Christian and C. Dower, Scope of Practice Laws in Health Care: Rethinking the Role of Nurse Practitioners (Oakland, CA: California HealthCare Foundation, January 2008).
States use scope of practice laws to expand the use of allied health workers as well as more highly trained health professionals. Lay community health workers, for example, can fill roles such as counselors and educators, patient advocates, or members of clinical teams. Community health workers usually share a racial or ethnic background and/or a primary language with the community members they serve, helping to build bridges between the health care system and populations who face financial, language, or cultural barriers to care. The Bureau of Labor Statistics estimated that there were approximately 121,206 community health workers nationwide in 2005, an increase of 41 percent from 85,879 in 2000.12
Expanding the pool of health care providers through scope of practice changes has been controversial. Often, physicians and dentists are concerned about the ability of mid-level trained professionals to provide high-quality care and treat complex cases; some also fear increased competition for their services. Advocates for broadening the scope of practice point out that doing so expands access to much-needed services, helps leverage the expertise of physicians and dentists by freeing them to treat more complex or critically ill patients, and reduces costs for many basic services. States have addressed some quality control concerns through careful delineation of authorized responsibilities, stringent educational and certification requirements, and requirements for physician/dentist supervision. States also can fund analyses of the likely impact of scope of practice changes, and then monitor and evaluate expansions. While some research has suggested that nurse practitioners can provide primary care that is comparable in quality to that provided by primary care physicians, this issue continues to generate debate and research.13
Primary Care Reimbursement
Another critical lever that states control is third-party reimbursement. State insurance departments and Medicaid programs determine whether various practitioners qualify for reimbursement by private insurers and Medicaid, respectively.14 States may also use their leverage as health care purchasers to attempt to reduce provider workforce shortages by setting competitive Medicaid reimbursement rates for primary care services and for new models of care, such as medical homes and community care teams that emphasize primary and preventive care.
There are significant disparities in Medicaid rates across states for services overall and for primary care specifically. While higher payment rates do not guarantee access to care, they do increase the probability that providers will accept Medicaid patients.15 Among pediatricians in private practice, there is evidence that Medicaid fee levels, in addition to the payment models and administrative requirements, influence provider acceptance rates.16 As of 2008, five states had Medicaid primary care reimbursement rates that were comparable to or higher than the rates paid by Medicare.
Some states are offering enhanced Medicaid payments (and/or encouraging additional private insurance payments) to practitioners for becoming "medical homes," a patient-centered approach to providing comprehensive primary care. This has the potential to improve access to care by encouraging practitioners to serve Medicaid beneficiaries and take an active role in prevention. In some cases, the payments are sufficient to cover the cost of care teams, including care coordinators and health educators.
Several states, including Vermont, North Carolina, and Rhode Island, are using Community Health Teams to coordinate primary care and other services in order to prevent and manage chronic disease, creating both a new care coordination structure and new payment strategies to support it. West Virginia and Pennsylvania are also planning to implement this model. Community health teams include a variety of providers, from care coordinators and nurse practitioners to nutritionists, social workers, behavioral health providers, and other community health workers. The model is also part of the national, multi-payer "Advanced Primary Care" demonstration projects being conducted in Medicaid and Medicare. Vermont is integrating the medical home and community health team models as part of its Blueprint for Health public–private initiative to reduce the toll of chronic diseases, an effort highlighted in the June/July 2009 issue of States in Action. The state divides the responsibility for funding the salaries of community health team staff among private insurers, the state Medicaid program, and Medicare.
Colorado's Medicaid program is offering enhanced payments for certain preventive services to practitioners who meet medical home certification. Working with the state, the Colorado Children's Health Access Program provides support services to pediatric practices—including a centralized care coordination/resource hotline, assistance with Medicaid enrollment and claims, and help with quality improvement projects—that qualify the practices for the additional reimbursement. This effort has helped to increase the portion of private pediatric practices serving children in public programs from about 20 percent in 1996 to more than 90 percent today.
Telemedicine
Telemedicine involves the use of conference calls as well as videoconferencing and other Web-based technologies for consultations, medical procedures, or examinations. Telemedicine can enhance access to care for patients in isolated rural areas or other areas where they face challenges in accessing care. Telemedicine is most often thought of as a strategy for increasing access to specialists for patients in remote areas, but it also can be used to expand access to primary care.
While telemedicine may produce savings by reducing travel time and expenses, it may require investments in sophisticated, and expensive, equipment. In addition, state physician licensing requirements may present challenges to the use of telemedicine across state borders, though 10 states have some version of a portable special-purpose license that covers telemedicine interactions.
As part of their efforts to improve access to primary care, states can cover telemedicine services in their Medicaid programs and require private insurers to reimburse for them. Estimates of the number of states that cover telemedicine in Medicaid vary from 19 to 34, with states taking different approaches and covering different services.17 Maine and New Hampshire recently enacted requirements for private insurers to pay for telemedicine, joining 10 other states with similar laws.
Table 2: States Requiring Private Insurance Coverage for Telemedicine | |
|
|
Source: M. Edwards, Background on Maine and New Hampshire's Enactment of Laws Mandating Private Insurance Reimbursement for Telemedicine, Maine Telemedicine Service News, September 2009.
Training and Placement Incentives
As described above, the federal government provides financial and other incentives to promote training of primary care physicians and nurses and encourage them to practice in underserved areas. States can supplement these efforts through tuition discounts, loans, and/or scholarships to students pursuing primary care degrees; loan forgiveness and affordable housing to graduates agreeing to practice in underserved areas for a specified period of time; and creation of medical school slots and incentives for students to specialize in primary care.
Community Health Center/Clinic Capacity
In 2008, community health centers provided care for more than 17 million patients, including 3.1 million who received dental services and nearly 700,000 who received mental health care.18 Through financing, reimbursement, and technical assistance for community health centers, rural health centers, and state-run clinics, states can increase the number and capacity of health centers that provide primary and preventive care to low-income and uninsured residents. A recent study found that increasing grant funding for federally qualified health centers between 1996 and 2006 increased the services available to patients, including uncompensated care.19 There is also evidence to suggest that by providing a regular source of care, health centers can reduce disparities in access to care related to race/ethnicity, income, and insurance status.20
Recent experience in New Orleans demonstrates the potential for community clinics to provide care for high-need populations. Since the city's major safety net hospitals were devastated by Hurricane Katrina, a network of independent primary care and behavioral health clinics has emerged to meet the population's substantial needs. A Commonwealth Fund study of patient experiences in these clinics in 2009 found that most patients reported having easy access to care, as well as good management of their chronic conditions.
|
1Estimates as of September 30, 2009. Health Resources and Services Administration, U.S. Department of Health and Human Services, http://bhpr.hrsa.gov/shortage/, accessed February 2010.
2 Access Denied: A Look at America's Medically Disenfranchised (Washington, D.C.: National Association of Community Health Centers, March, 2007).
3 D. J. Derksen. and E.-M. Whelen, Closing the Health Care Workforce Gap (Center for American Progress: Washington, D.C., December 2009).
4 Schoen, R. Osborn, P. T. Huynh et al., "Primary Care and Health System Performance: Adults' Experiences in Five Countries," Health Affairs Web Exclusive, October 28 2004:W4-487–503.
5 Programs funded by the American Recovery and Reinvestment Act include: Scholarships for Disadvantaged Health Professions Students; the Centers for Excellence program; the Nursing Workforce Diversity program; the Health Careers Opportunity program; and the Equipment to Enhance Training of Health Professionals program.
6 Key Facts About the National Health Service Corps, U.S. Department of Health and Human Services, http://www.hhs.gov/recovery/programs/nhsc/nhscfactsheet.html, Accessed February 2010.
7 Loan repayment of up to $50,000 in student loans is also available to dental hygienists and mental health providers in exchange for two years of service at an approved site in a HPSA.
8 D. J. Derksen and E.-M. Whelen, Closing the Health Care Workforce Gap (Washington, D.C.: Center for American Progress, December 2009), p. 10.
9 There is a federal requirement that nurse practitioners must complete at least a three-month specialized training program.
10 Total Nurse Practitioners, 2009, Statehealthfacts.org, http://www.statehealthfacts.org/comparemaptable.jsp?ind=773&cat=8, Accessed February 2010.
11 For a more detailed discussion of these distinctions and the wide range of state definitions of these terms, see: Assessing Scope of Practice in Health Care Delivery: Critical Questions in Assuring Public Access and Safety. (Dallas, TX: Federation of State Medical Boards, 2005), http://www.fsmb.org/pdf/2005_grpol_scope_of_practice.pdf.
12 Community Health Worker National Workforce Study (Washington, D.C.: U.S. Department of Health and Human Services Health Resources and Services Administration, Bureau of Health Professions, 2007).
13 M. O. Mundinger, R. L. Kane, E. R. Lenz et al., "Primary Care Outcomes in Patients Treated by Nurse Practitioners or Physicians: A Randomized Trial," Journal of the American Medical Association, 2000 283:59–68.
14 S. Christian and C. Dower, Scope of Practice Laws in Health Care: Rethinking the Role of Nurse Practitioners (Oakland, CA: California HealthCare Foundation, January 2008). http://www.chcf.org/documents/policy/ScopeOfPracticeLawsNursePractitionersIB.pdf
15 P. J. Cunningham and L. M. Nichols, "The Effects of Medicaid Reimbursement on the Access to Care of Medicaid Enrollees: A Community Perspective," Medical Care Research and Review, 2000 62(6):676–96.
16 S. Berman, J. Dolins, S. Tang et al., "Factors that Influence the Willingness of Private Primary Care Physicians to Accept More Medicaid Patients," Pediatrics, 2002 110(2): 239–48.
17 N. A. Brown, State Medicaid and Private Payer Reimbursement for Telemedicine: An Overview, Journal of Telemedicine and Telecare, 2006 12(Suppl. 2):S32–9 and J. P. Marcin, J. Trujano, C. Sadorra et al., "Telemedicine in Rural Pediatric Care: the Fundamentals," Pediatric Annals, 2009 38(4): 224–26.
18 Providing Access to Health Care in the Nation's Most Needy Communities, http://bphc.hrsa.gov/.
19 A. T. Lo Sasso and G. R. Byck, "Funding Growth Drives Community Health Center Services," Health Affairs, 2010 29(2): 289–96.
20 R. M. Politzer, "Inequality in America: The Contribution of Health Centers in Reducing and Eliminating Disparities in Access to Care," Medical Care Research and Review, June 2001 58(2):234–48.


