As the new Congress convenes and the Supreme Court prepares to hear arguments in the King v. Burwell case challenging tax subsidies for insurance purchased through the federally facilitated marketplaces, proposals to repeal and replace the Affordable Care Act (ACA) are resurfacing. Many of these rely on high-risk health insurance pools to cover people with preexisting health conditions.
In fact, the risk pools are suggested as a viable alternative to the ACA's ban on preexisting condition exclusions in the individual market and the marketplaces. My recent analysis of high-risk pools, however, explains why these entities simply are not a realistic alternative to coverage requirements under the ACA. In a nutshell, high-risk pools:
- are prohibitively expensive to administer,
- are prohibitively expensive for consumers to purchase, and
- offer much less than optimal coverage, often with annual and lifetime limits, coverage gaps, and very high premiums and deductibles.
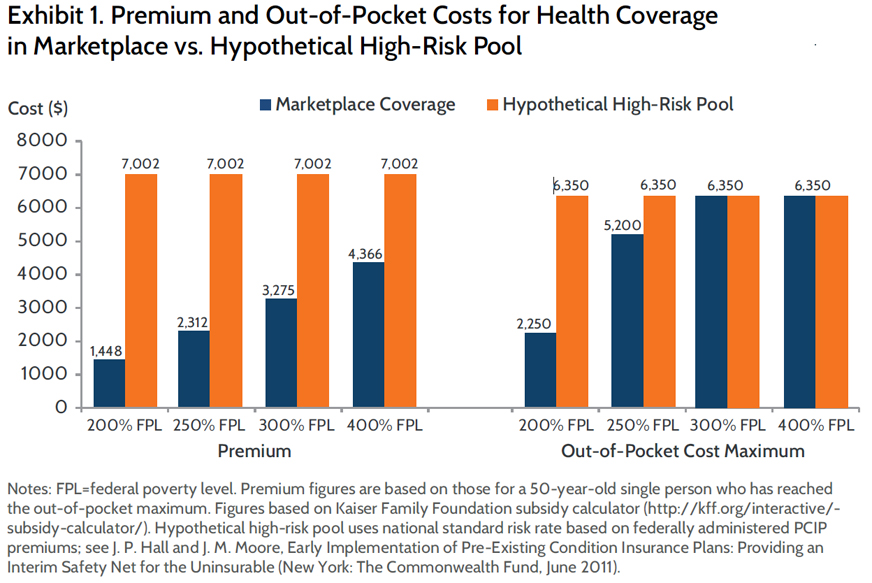
Recent proposals to replace ACA reforms with high-risk pools focus on using state-based programs, but historical experience with 35 state-based high-risk pools and more recent experience with the national Pre-Existing Condition Insurance Plan (PCIP) illustrate the problems with this approach. Even though state-based high-risk pools charged premiums of up to 250 percent of those charged to healthy beneficiaries in the individual insurance market, premium revenues paid just 53 percent, on average, of program costs. In addition to these high premiums, enrollees in state-based high-risk pools faced annual deductibles as high as $25,000 and annual coverage limits as low as $75,000.1 Past research indicated that high costs and limited benefits associated with high-risk pool coverage resulted in delayed or forgone care and adverse outcomes for enrollees. Many also accrued medical debt despite having insurance.2
For these reasons, use of high-risk pools in lieu of marketplace and Medicaid expansion coverage would result in greater state and federal costs, fewer people with preexisting conditions able to obtain coverage, and coverage that fails to meet the often greater needs of people with chronic conditions. Affording coverage would be particularly difficult for people with incomes below 400 percent of the federal poverty level, who accounted for 80 percent of the uninsured population with preexisting conditions prior to implementation of the ACA.3
By concentrating risk, high-risk pools also concentrate costs, resulting in greater expenses to administrators and consumers and driving plans to impose severe coverage limits that often serve to negate the benefit of having insurance. Indeed, pronounced adverse selection is common in high-risk pools, because only the very sickest and most expensive individuals are willing to pay the high premiums for coverage, increasing administrative costs even more. This phenomenon was evident in several state-based high-risk pools, such as in California and Kansas, where enrollment declined from 2009 to 2011, but premiums totals and medical reimbursement costs increased, even with coverage limits in place.4 In stark contrast, coverage expansions under the Affordable Care Act spreading risk across a broad population to decrease per capita costs and allow for more affordable and comprehensive coverage for all. By their very nature, high-risk pools cannot and will not do so.
- Comprehensive Health Insurance for High-Risk Individuals: A State-by-State Analysis, 2012/2013 (Denver, Colo.: National Association of State Comprehensive Health Insurance Plans).
- J. P. Hall and J. M. Moore, “Does High-Risk Pool Coverage Meet the Needs of a Population at Risk for Disability?” Inquiry, Fall 2008 45(3):340–52; J. P. Hall, S. L. Carroll, and J. M. Moore, “Health Care Behaviors and Decision-Making Processes Among Enrollees in a State High-Risk Insurance Pool: Focus Group Findings,” American Journal of Health Promotion, May–June 2010 24(5):304–10; and J. P. Hall, J. M. Moore, and G. W. Welch, “Preventing Disability Among Working Participants in Kansas’ High-Risk Insurance Pool: Implications for Health Reform,” Journal of Vocational Rehabilitation, 2011 34(2):119–28.
- M. Merlis, Health Coverage for the High-Risk Uninsured: Policy Options for Design of the Temporary High-Risk Pool, No. 2 (Washington, D.C.: National Institute for Health Care Reform, May 2010).
- Comprehensive Health Insurance, 2012/2013.



