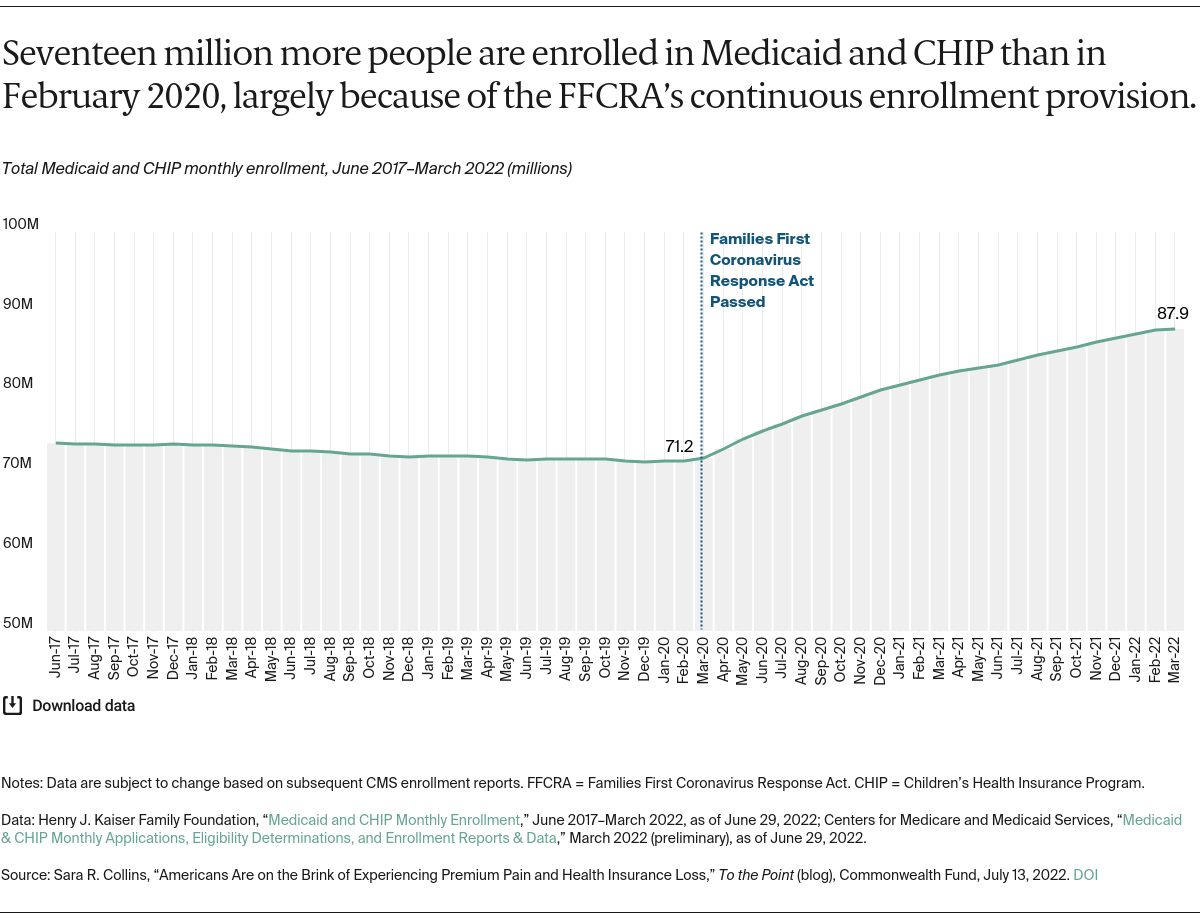
Why did this requirement drive enrollment so much higher than in prior years?
Put simply, prior to FFCRA, existing state and federal policy make it hard for eligible people to stay enrolled in Medicaid. People become eligible for Medicaid because of their income or need for health care services, like being pregnant or having a disability. Under federal law, states must verify that Medicaid enrollees remain eligible for coverage at least once a year, but many states check eligibility more frequently. Some states allow as little as 10 days for enrollees to submit documents to prove eligibility. Even small income bumps, such as from seasonal work, can lead to disenrollment, though income might drop again in a few months. Consequently, the average length of enrollment in Medicaid is less than 10 months. One study found that over a two-year period, one-third of nondisabled, nonelderly adult Medicaid enrollees became disenrolled; of those, three-quarters became uninsured for part or all of the remaining time period. Other studies have found that more than half (55%) of pregnant women1 enrolled in Medicaid at the time of their delivery reported a gap in health insurance within six months.
Gaps in coverage have consequences for people’s health care and financial security. The 2020 Commonwealth Fund Biennial Health Insurance Survey found that more than half of adults who were insured at the time of the survey but had a gap in coverage in the past year, reported skipping care or not filling prescriptions, or had problems paying medical bills.
Why Has Marketplace Enrollment Grown?
The American Rescue Plan Act (ARPA) lowered premiums for marketplace plans. In Commonwealth Fund surveys, the primary reason people give for either not enrolling in marketplace plans or dropping coverage is because the premiums are too expensive. The ARPA addressed this barrier by substantially lowering premiums through larger subsidies, leading to average per person per month savings of $67. CBO estimates the ARPA enhanced subsidies increased 2022 marketplace enrollment by 2.3 million people.
What Happens Next?
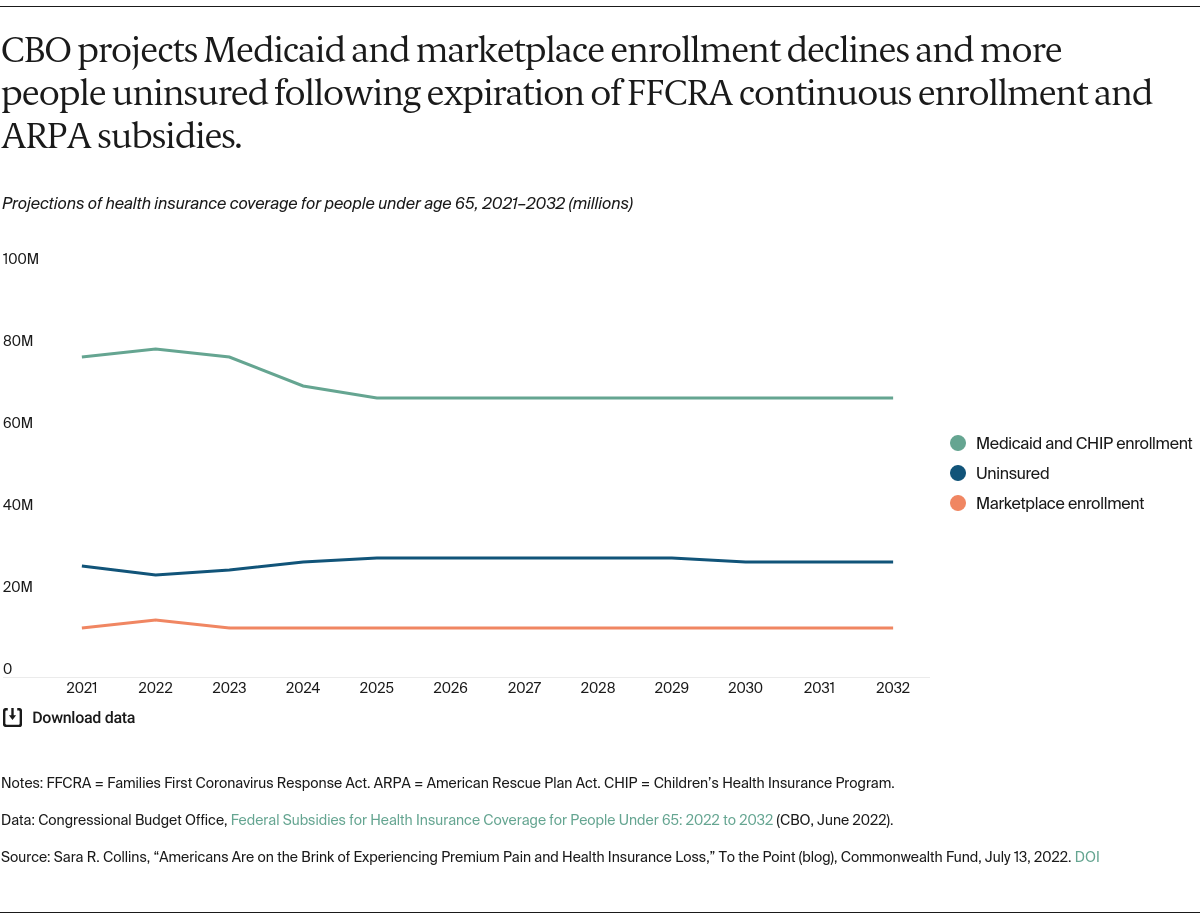
The bad news is that these coverage and premium protections will expire within months. Without congressional intervention, the ARPA subsidies will expire at the end of 2022. The continuous enrollment requirement will end when the PHE designation ends, anticipated in 2023, triggering a massive eligibility redetermination effort by states for all people enrolled in Medicaid. Evaporation of these pandemic policies led CBO to forecast that over the next 10 years:
- marketplace enrollment will fall by 1.4 million in 2023, with further declines thereafter
- Medicaid enrollment will decline by 12 million by 2025
- the number of uninsured people under age 65 will jump from a low of 25 million in 2022 to 29 million by 2025.