A new report, which describes visit trends through the end of 2020, is available here.


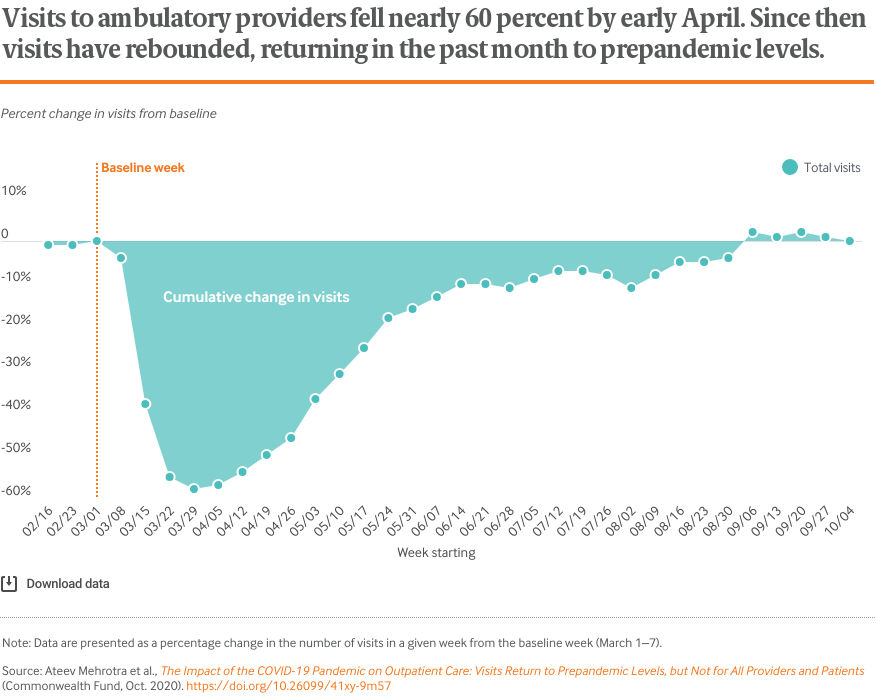
Visits for outpatient care, which had fallen nearly 60 percent in April, have returned in the past month to the levels prior to the COVID-19 pandemic.
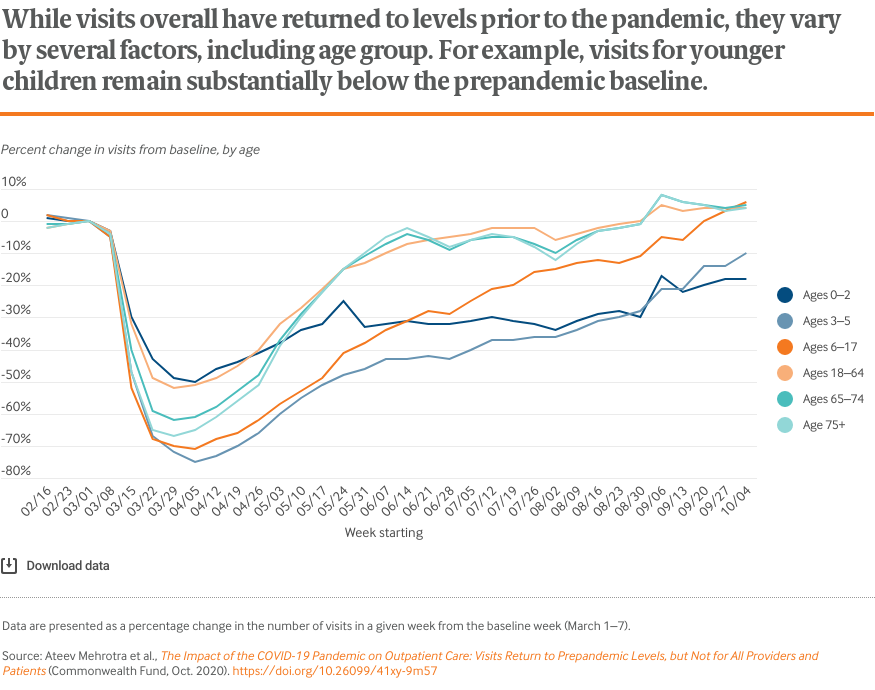
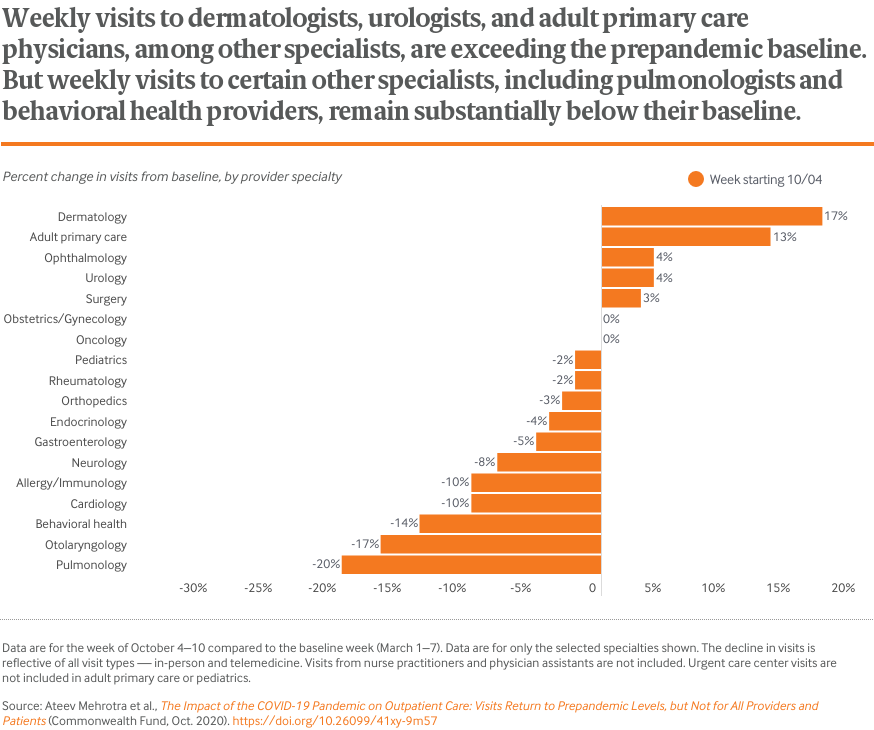
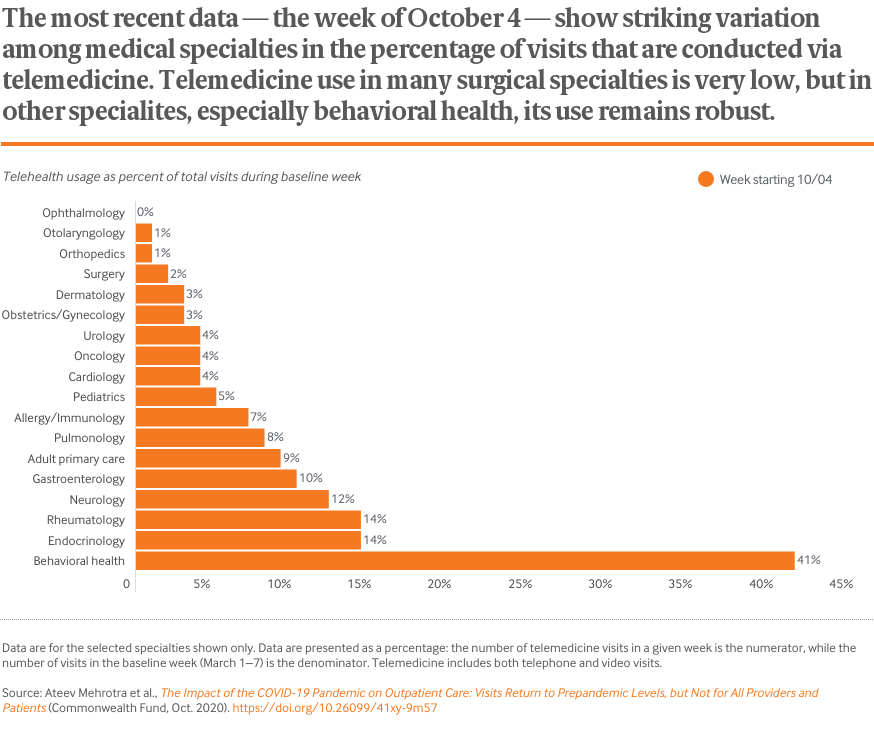
While outpatient visits overall have rebounded, there’s a lot of variation. The number of visits to dermatologists is actually higher than before the pandemic, while visits to behavioral health providers remains well below.
Visits for outpatient care, which had fallen nearly 60 percent in April, have returned in the past month to the levels prior to the COVID-19 pandemic.
While outpatient visits overall have rebounded, there’s a lot of variation. The number of visits to dermatologists is actually higher than before the pandemic, while visits to behavioral health providers remains well below.
A new report, which describes visit trends through the end of 2020, is available here.
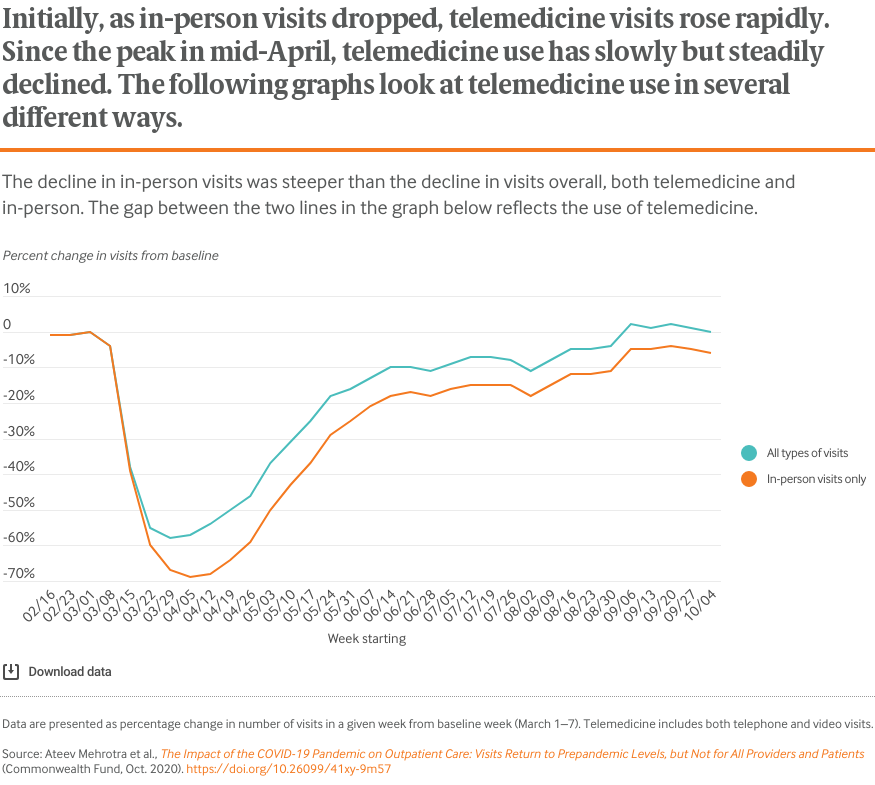
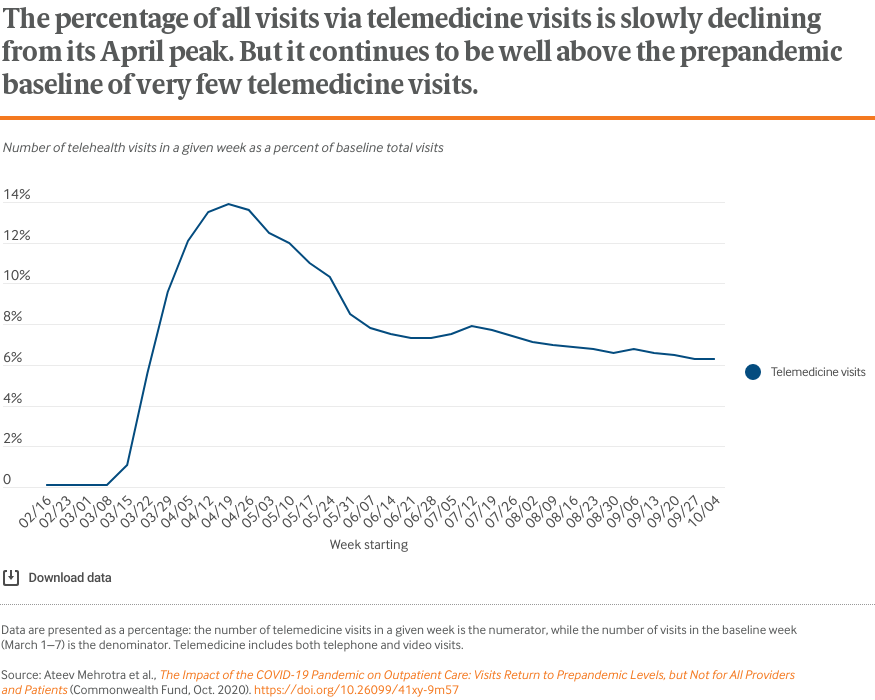
The COVID-19 pandemic has dramatically altered the delivery of outpatient care. Initially, health care practices deferred elective visits, modified their practices to safely accommodate in-person visits, and increased their use of telemedicine.
In late April, we published results showing that, early in the pandemic, the number of visits to ambulatory care providers had declined by nearly 60 percent. Our mid-May update showed a substantial rebound in office visits, but that had plateaued by late June. In August, we highlighted drops in visit counts in what were hotspots of COVID-19 incidence. In this report, our fifth, we update outpatient visit trends through October 10.
As summer ended, state and local governments lifted many restrictions on travel and nonessential services. Like many businesses, outpatient practices and their patients have adapted to this new normal. Yet providers in some areas of the country have been facing surges of COVID-19 cases in their communities and the challenges of keeping patients and clinicians safe while also maintaining revenue.
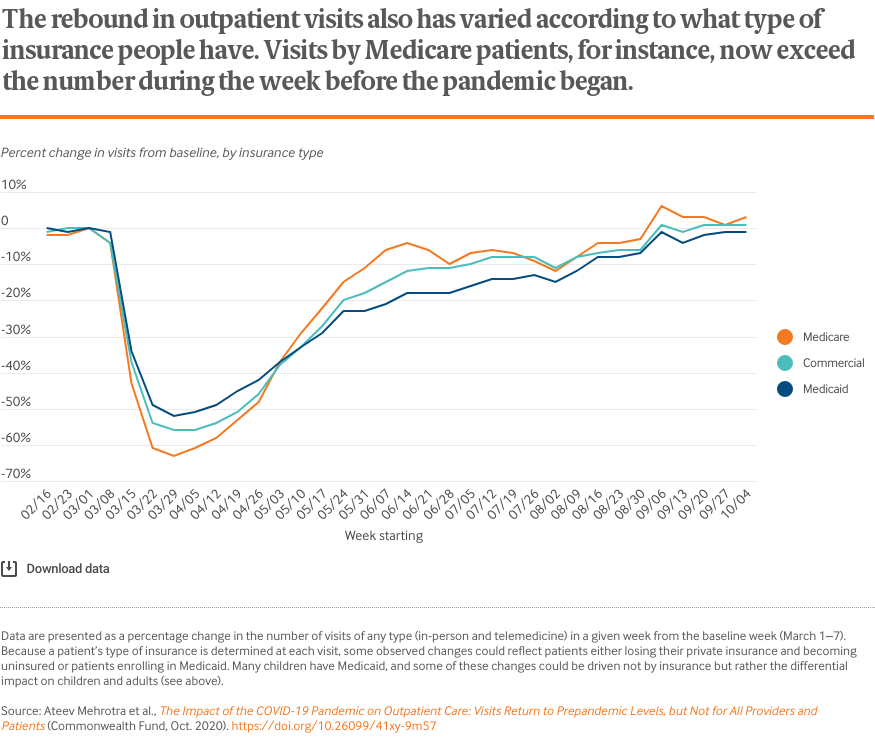
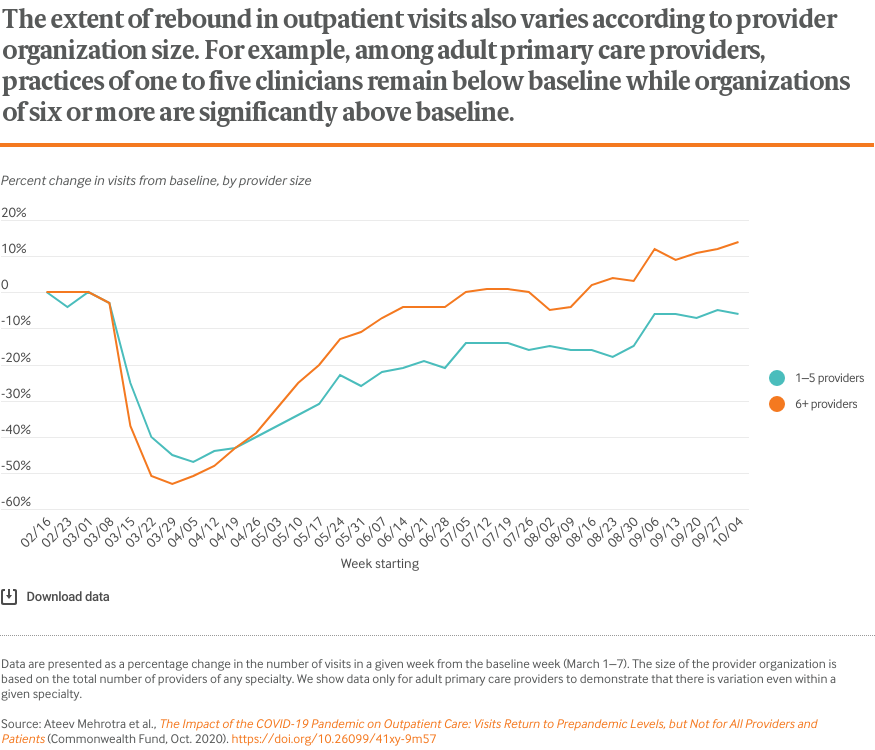
The charts that follow illustrate that overall visit counts per week have fully rebounded. In total, weekly visit counts now slightly exceed prepandemic levels. However, there is considerable variation by patient age, geographic area, clinical specialty, and insurance coverage.
By tracking trends in outpatient office visits, we hope to shed light on several persistent questions:
Researchers at Harvard University, the Commonwealth Fund, and Phreesia, a health care technology company, analyzed data on changes in visit volume for the more than 50,000 providers that are Phreesia clients. Details on data sources, analyses, and study limitations are available at the bottom of this post.
Phreesia is a health care technology company that helps ambulatory practices with the patient intake process, including registration, insurance verification, patient questionnaires, patient-reported outcomes, and payments. The data reported here come from Phreesia’s clients, which include more than 1,600 provider organizations representing more than 50,000 providers across all 50 states. In a typical year, these provider organizations have more than 50 million outpatient visits, or more than 1 million visits a week.
The provider organizations include independent single-provider practices, multispecialty groups, Federally Qualified Health Centers, and large health systems. Of all visits in a typical week before the pandemic, 47 percent are with primary care physicians (adult and pediatric) and the other 54 percent of visits are spread across more than 25 specialties. Visits with nurse practitioners and physician assistants are included under these 25 other specialties.
Data come from several sources at the organizations: 1) practice management/scheduling software; 2) check-in information submitted via patients on the Phreesia platform (e.g., reported age); and 3) selected data from the electronic health record, such as problem lists.
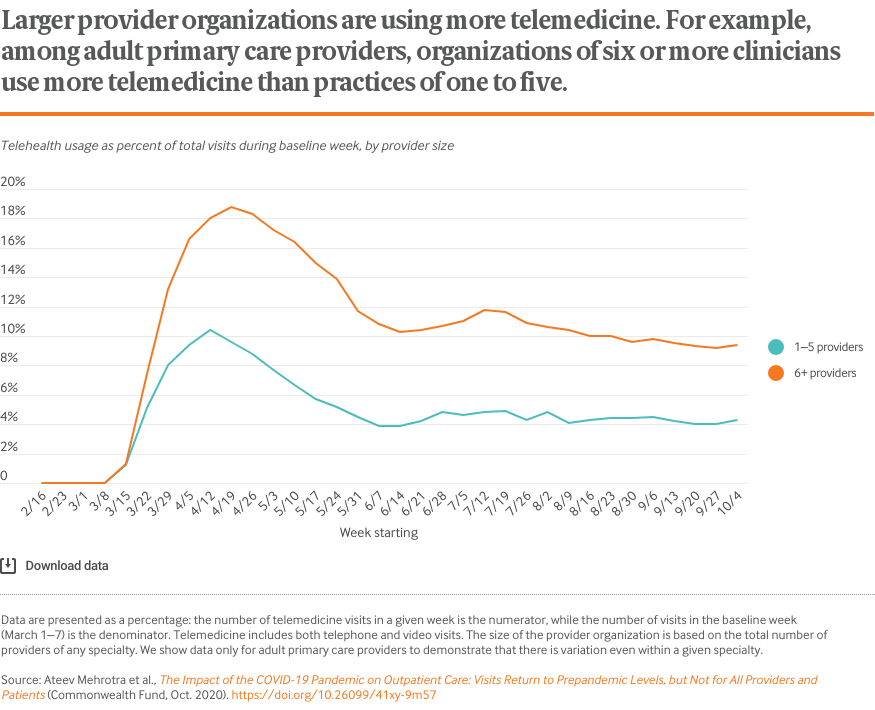
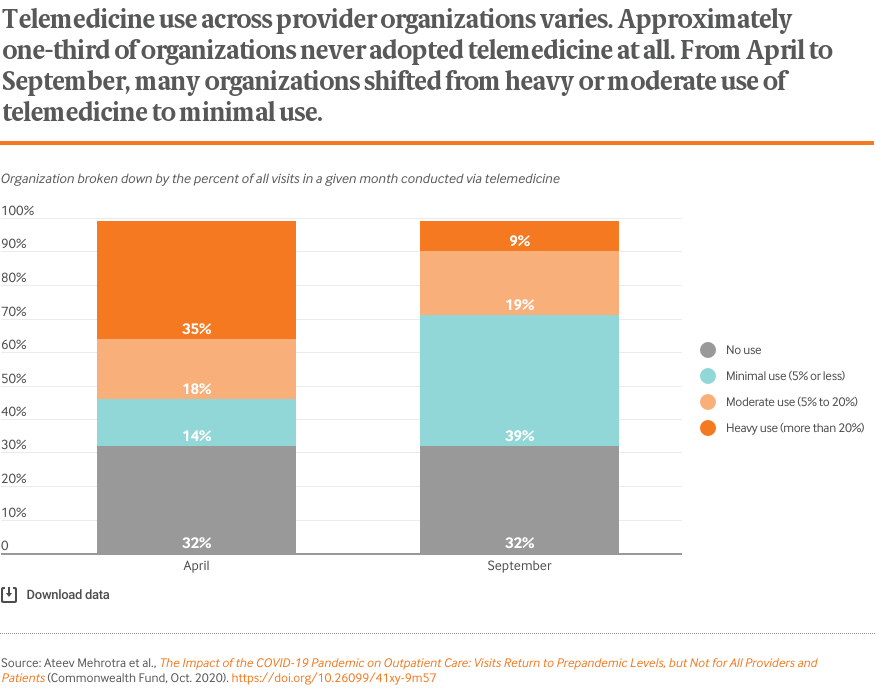
Visits were captured from February 1 through October 10, 2020. A visit was counted if it was in the practice’s scheduling software and the patient was checked in. A visit is considered checked in when either the patient or someone at the practice (such as a nursing assistant) filled in the necessary information using the Phreesia platform and the patient was ready to see the provider. Telemedicine visits were identified in the scheduling software based on the appointment type or location. Telemedicine includes both telephone and video visits. The data exclude any new Phreesia clients who joined after February 15, 2020.
Phreesia staff, in consultation with Harvard University and Commonwealth Fund researchers, analyzed all data. They calculated results and shared them with the Harvard researchers in aggregate form as percentage drops from baseline. The baseline for visits was defined as the week of March 1 to 7 — a representative week among the organizations prior to effects of the pandemic. Visits on holidays were excluded.
The data have limitations. As with any convenience sample of providers, the patterns we observe may not be representative of all organizations nationally or regionally. Unscheduled same-day and walk-in visits are typically captured in the scheduling software, but it is possible some unscheduled telephone encounters were not captured if the software did not record them. Workflow and documentation practices have likely shifted during the pandemic as well. Finally, the fraction of all visits identified as telemedicine may be underestimated, since early in the pandemic providers were still creating processes to designate telemedicine visit types in their scheduling software.
Publication Details
Date
Contact
Ateev Mehrotra, Associate Professor of Health Care Policy and Medicine, Harvard Medical School
[email protected]Citation
Source: Ateev Mehrotra et al., The Impact of the COVID-19 Pandemic on Outpatient Care: Visits Return to Prepandemic Levels, but Not for All Providers and Patients (Commonwealth Fund, Oct. 2020). https://doi.org/10.26099/41xy-9m57
Area of Focus