How can integrated care promote equitable access to behavioral health services?
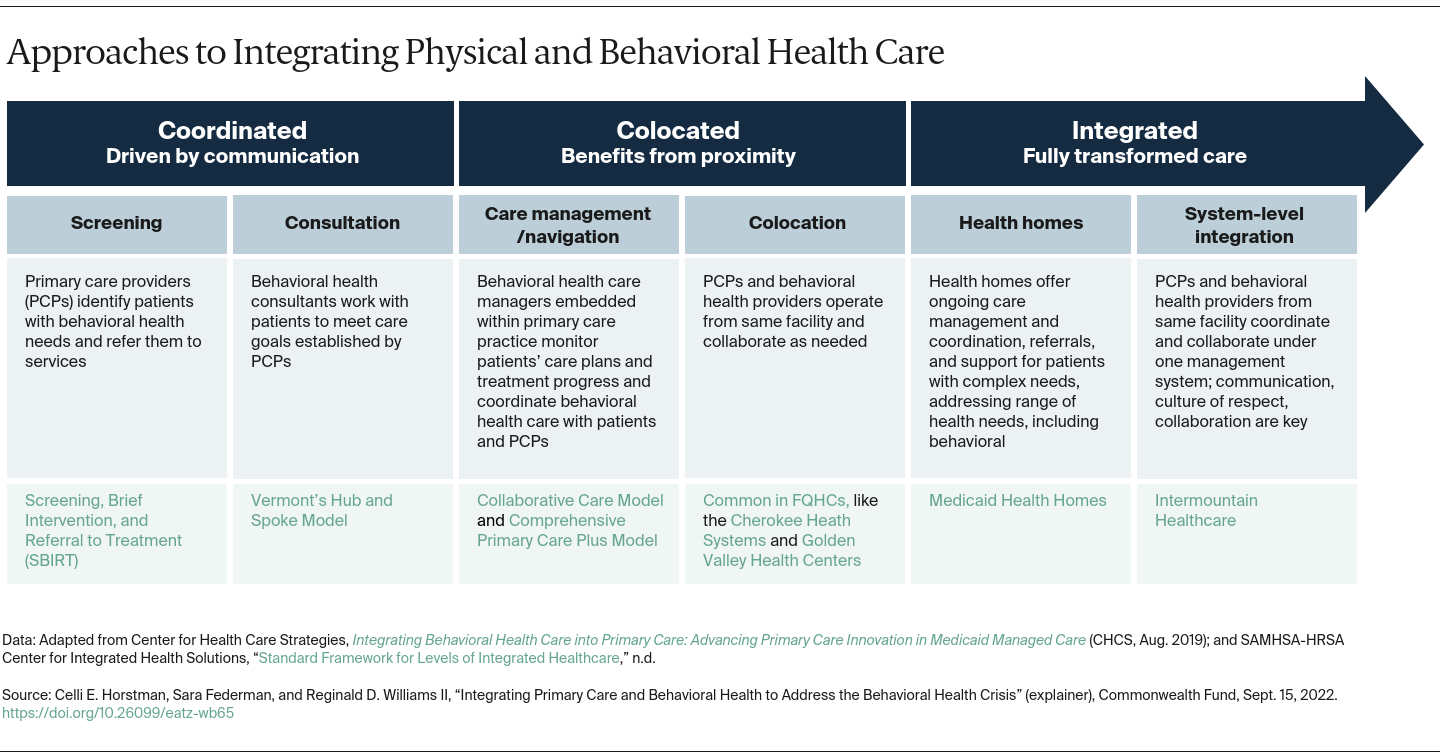
Integrated care is vital for expanding access to behavioral health services. Given the widespread barriers to accessing specialty behavioral health care — including provider shortages, high out-of-pocket costs, and gaps in insurance coverage — many people are already seeking behavioral health treatment from their PCPs. However, PCPs often feel unprepared to manage patients’ mental health or substance use concerns, especially when their conditions are more severe. Integrated care equips PCPs and associated providers with effective tools for diagnosis and treatment, while also expanding the workforce to include paraprofessionals — community health workers or peer support specialists — who offer counseling, care management, social support, and skill-building services. This approach has been shown to improve behavioral health access and outcomes across age groups and diagnoses.
Integration is also an important strategy for addressing racial, ethnic, and geographic behavioral health disparities. For people of color, integrated care can address many of the barriers that disproportionately limit their use of behavioral health services compared with their white counterparts. For example, being able to get behavioral health services in the offices of a trusted primary care provider can ease the stigma of seeking treatment that can be a barrier to care for some people of color. In rural communities, where provider shortages tend to be severe, integration can help increase access by leveraging local providers more efficiently, incorporating telemedicine to fill gaps, and promoting collaboration with community services.
Ultimately, health systems are more likely to find success with integrated care models that are tailored to the cultural and linguistic needs and preferences of their local community.
What are the challenges to widespread integration?
Workforce. Despite the potential for integration to address provider shortages, states and health systems do not engage paraprofessionals to their full potential. Currently, 39 states allow Medicaid reimbursement for peer support specialists, and Medicare covers only traditional behavioral health providers. Despite limited coverage from the Centers for Medicare and Medicaid Services, paraprofessionals can reduce staffing shortages and patient access barriers, expand the capabilities of integrated care teams, and promote patient-centered care.
Training and licensing burdens further strain the workforce. Treatment for opioid use disorder, specifically prescribing buprenorphine, requires extensive provider training to obtain the necessary waiver. In 2018, less than 4 percent of physicians had received this waiver. Among physicians who can prescribe buprenorphine, few do, often because of lack of support at the practice level and inadequate reimbursement. While the types of providers who are eligible for this waiver have been expanded, the burden of training and subsequent lack of support continues to limit access to this treatment.
Technology. Successful integration requires communication and collaboration between PCPs, behavioral health providers, and patients. Technology, including telehealth (virtual visits with a provider) and integrated communication systems (electronic health systems and other health information technology that supports interoperability), can help, enabling providers in different locations to communicate with one another and increase access for patients who can’t get to a provider.
Since the COVID-19 pandemic began and reimbursement policies changed, telehealth use by patients and providers has jumped. Still, high-speed internet access remains a problem in rural and some urban areas. Certain treatments for substance use disorders also require an initial in-person visit. Moreover, certain policies that have made it easier for providers to be reimbursed for delivering telehealth services are set to expire once the COVID public health emergency ends.
How do we pay for the integration of behavioral health with primary care?
Provider payment is a significant barrier to integration. The fee-for-service payment system that predominates in the United States disincentivizes integrated care by reimbursing providers for individual services instead of the whole-care experience. In cases where reimbursements have been designated for integrated care, like the collaborative care model reimbursement codes used in Medicare, current payment levels aren’t always enough to cover the cost of care. Providers in some states also are challenged by same-day billing restrictions, which limit reimbursements to either primary care or behavioral health services in a single visit.
Further, the immense startup costs practices face as they change workflows, hire and train staff, upgrade technologies, and launch new quality improvement processes are not reimbursable. Even after implementing integrated care models, current payment approaches may not allow providers to immediately recoup these costs.
Despite these cost burdens, integrated care can generate savings, and rethinking how we pay for this care is an important step to realizing them. Value-based payments, which incentivize and hold providers accountable for the quality of care, have been used to promote integration, generate cost savings, and improve quality. Several integrated care models have moved away from traditional fee-for-service payments to payments that are linked to quality and value, including episode-based, bundled payments in Minnesota and capitated payments that incentivize integration and quality improvement in Massachusetts. When implementing new payment models to support integration, it’s important that incentives are well aligned to promote sustainable integration.
Integration offers a way to address the country’s growing behavioral health crisis while advancing health equity. But making integrated care the norm, rather than the exception, will require the shared commitment of policymakers, payers, and providers to invest in systems change.