Abstract
The new health insurance exchanges are the core of the Affordable Care Act’s (ACA) reforms, but how the law improves the nonsubsidized portion of the individual market is also important. This issue brief compares products sold on and off the exchanges to gain insight into how the ACA’s market reforms are functioning. Initial concerns that insurers might seek to enroll lower-risk customers outside the exchanges have not been realized. Instead, more-generous benefit plans, which appeal to people with health problems, constitute a greater portion of plans sold off-exchange than those sold on-exchange. Although insurers that sell mostly on the exchanges incur an additional fee, they still devote a greater portion of their premium dollars to medical care. Their projected administrative costs and profit margins are lower than are those of insurers selling only off the exchanges.
Background
The Affordable Care Act’s health insurance market reforms are designed to encourage insurers to compete on the value of their products rather than on their ability to identify and segment people based on their risk of incurring medical costs. The ACA does this by: requiring insurers to accept all applicants; requiring them to charge consumers within a geographic area the same age-banded premiums, regardless of health status; and prohibiting other forms of so-called medical underwriting, like excluding preexisting conditions. In addition, the ACA’s state and federal health insurance exchanges (also called marketplaces) help consumers shop for insurance by standardizing covered benefits and presenting information about costs in an accessible way.
Health insurers, however, are not required to sell policies through the new exchanges.1 In the individual market, subsidized coverage—which is offered to people earning up to 400 percent of the federal poverty level (about $47,000 for an individual or $97,000 for a family of four)—is available only on the exchanges.2 But insurers that sell subsidized coverage may also sell outside the exchanges. Moreover, some insurers in the individual market opt to stay out of the exchanges entirely, instead selling to people who do not qualify for or claim the premium subsidies.
Accordingly, two distinct segments have emerged in the individual market: coverage sold on the exchanges, mostly to people who qualify for a subsidy; and coverage sold off the exchanges, through traditional channels to people who pay full price. This division of the individual market provides an opportunity to explore how effective the ACA has been at promoting good coverage at lower prices.
Comparing these two segments allows us the opportunity to observe whether insurers use this market division to engage in the types of risk segmentation that the ACA is meant to eliminate. Before the exchanges launched, analysts speculated that insurers might attempt to segregate higher-risk from lower-risk subscribers by encouraging those at higher risk to purchase on the exchanges and those with lower risks to remain off the exchanges.3 If successful, that adverse selection strategy could increase the cost of government subsidies.
The ACA has several provisions that keep any potential for risk segregation in check. First, to keep insurers from segregating their risk pools, the ACA requires each insurer in the individual or small-group market to maintain a “single risk pool” for ACA-compliant plans.4 This means that insurers must use the same premium rating factors for all subscribers and plans within the relevant market, rather than using different rates for separate risk pools. If an insurer sells coverage both on and off the exchanges, rates must be identical for identical coverage. If coverage differs, rates may be adjusted only for actuarial value and not for differences in health status or overhead costs. Second, to counter insurers’ incentives to avoid greater risks across the market, the ACA has a risk-adjustment mechanism in the individual and small-group markets that requires insurers with lower-risk subscribers to subsidize insurers that enroll people expected to incur more medical claims.
To assess how well these rules are working, we examine insurers’ federal filings for premium rates that took effect in 2015 for ACA-compliant products sold on and off of the insurance exchanges.5 These filings, which demonstrate carriers’ compliance with the ACA’s rating rules, allow us to observe how different market segments are performing.
Findings
Market Shares and Risk Selection
Because the ACA’s premium subsidies are available only through the federal and state exchanges, it is no surprise that the majority of coverage in the individual market is sold there. For 2015, insurers projected that only 21 percent of their anticipated 14 million ACA-compliant subscribers will be in plans sold only off the exchanges. The others will be in plans sold predominantly through the exchanges.6
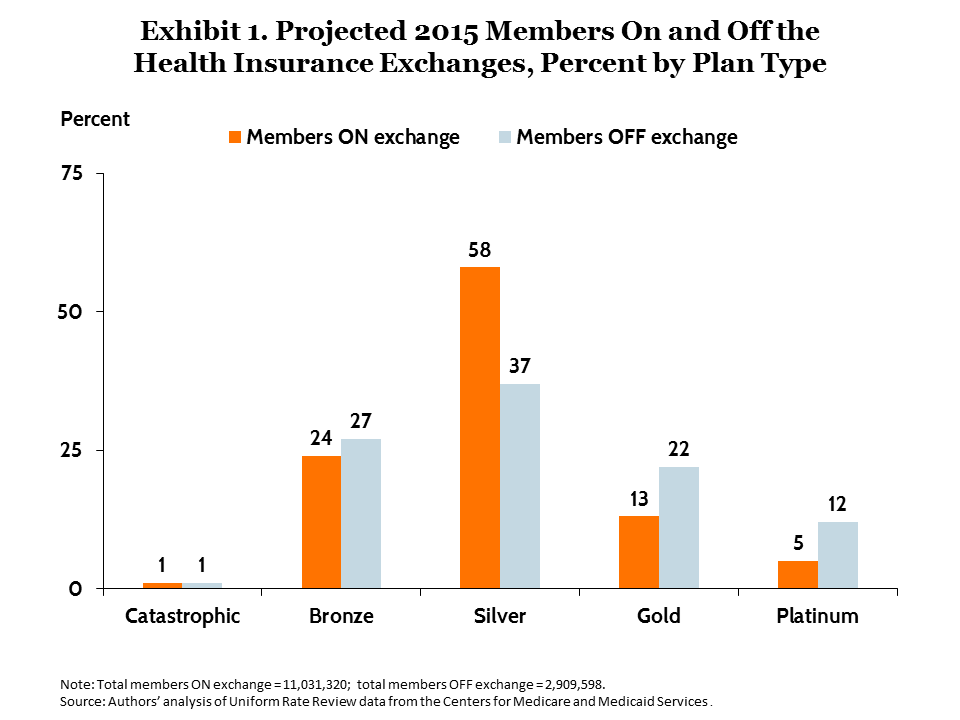
We see little evidence of insurers actively pursuing risk segmentation in their offerings on and off the exchanges. One way risk segmentation might occur is for insurers to offer leaner plans off the exchanges because these appeal more to healthier people. But this does not appear to be occurring (Exhibit 1). Bronze-level plans, which cover only an average 60 percent of medical expenses, have a similar share on and off the exchanges—about one-quarter of projected enrollment. Notably, the most generous (and most expensive) plans—i.e., the gold- and platinum-level plans—are much more prevalent off-exchange than on, constituting one-third of projected enrollment off compared with less than one-fifth on. There is a much greater proportion of people in silver-level plans on the exchanges, compared with off (58% vs. 37%). One likely reason is that lower-income people who are eligible for reduced out-of-pocket cost-sharing must choose a silver plan to receive the full benefit of that subsidy.
Another factor that dampens potential adverse selection is the different provider networks that insurers offer on and off the exchanges. The exchanges allow for shopping based on head-to-head price comparisons. Therefore, to be competitive, insurers formed narrower provider networks based on doctors and hospitals willing to give deeper discounts.7 Narrow networks are less appealing, however, to people with more complex health problems who tend to prefer a wider choice of specialists. Therefore, people with preexisting conditions could be more likely to shop for plans off the exchanges.
Two different sources suggest this is happening. A health insurance website that aggregates insurance prices reported in 2014 that the least expensive ACA-compliant plans offered by the major insurers that sold only off the exchanges cost 40 percent more than the cheapest equivalent coverage sold on the exchanges (disregarding subsidies).8 It is unlikely that this large difference was simply the result of price competition. It more likely occurred because insurers offered more expensive plans with broader networks off the exchanges. These broader networks have not attracted sicker subscribers, however. Surveys by the Kaiser Family Foundation found similar age distributions in subscribers on and off the exchanges in their first two years of operation.9 Moreover, based on self-reported health status, enrollees off the exchanges have a similar health profile. Thus, it does not appear that, at least initially, the leaner networks on the exchanges are pushing sicker people off the exchanges.
Targeted Medical Loss Ratios
The ACA’s insurance exchanges were intended to improve consumer value in two ways: by making insurers more price competitive and by reducing overhead sales costs. One way to measure this is through insurers’ medical loss ratios (MLRs). The MLR is the percentage of total premium cost that an insurer spends on medical claims, with the remainder earmarked for overhead costs and profits.
To isolate the separate market dynamics, we compared the projected MLRs in 2015 for insurers that sell only off-exchange with those that sell all products on-exchange.10 To minimize the effect of outliers, we report median rather than mean values. As shown in Exhibit 2, insurers competing off the exchanges project a median MLR that is 3.3 percentage points lower—meaning they spend this much more on overhead and profit—than those that sell all of their individual plans on the exchanges. This difference is largely accounted for by greater administrative costs. The median for administrative costs is 3.2 percentage points higher off the exchanges.
Exhibit 2. Projected Median Financial Performance Ratios, 2015
| All insurers | Insurers selling all products on the exchanges |
Insurers selling all products off the exchanges |
|
| N= | 571* | 194 | 222 |
| Medical loss ratio | 78.1% | 79.3% | 76.0% |
| Administrative ratio | 14.0% | 12.0% | 15.2% |
| Tax and fee ratio | 5.9% | 6.2% | 5.2% |
| Profit ratio | 2.5% | 2.0% | 2.7% |
Note: Median values are not additive across the four performance measures.
* The total for “All insurers” exceeds the sum of issuers “ALL ON” and “ALL OFF” because some issuers
offer plans both on and off exchanges.
Source: Authors’ analysis of Uniform Rate Review data from the Centers for Medicare and Medicaid Services.
While their administrative costs may be lower, insurers selling products on the exchanges are also projected to have higher taxes and fees because the exchanges charge fees for plans purchased there.11 These fees are built into each insurer’s marketwide rates, including rates for plans sold off-exchange that do not incur the fee, which somewhat reduces the rate impact of these fees.12
Summing together all three overhead components—administrative costs, profits, and taxes and fees—the lower total overhead by insurers on the exchanges suggests that the fees charged by exchanges cover services that help reduce insurers’ sales and administrative costs. That is only one possible interpretation, however. Because the insurers that sell exclusively off-exchange are different from those that sell on-exchange, we cannot draw firm conclusions about whether the exchanges themselves cause insurers to devote a lower proportion of their premiums to overhead and profits. It is possible that carriers with historically higher overhead or profits chose not to participate in the exchanges. However, it is also possible that the exchange structure promotes greater efficiency by reducing sales and administrative costs and by increasing price competition.
Components of Premium Increases
We next look at changes in premiums between 2014 and 2015. Exhibit 3 shows the components of insurers’ 2015 premium increases, overall and on and off the exchanges. Overall, the member-weighted average premium paid in the individual market increased $30 per person per month in 2015, with a somewhat higher increase off the exchanges ($34) compared with on ($29).13
Exhibit 3. Components of Premium Increases in the Individual Market for 2015,
On vs. Off the Health Insurance Exchanges
| All individual products (PMPM) |
Percent increase |
Products on exchange (PMPM) |
Percent increase |
Products off exchange (PMPM) |
Percent increase |
|
| N= | 1,060 | 578 | 482 | |||
| Inpatient | $3.6 | 12.1% | $3.31 | 11.3% | $4.93 | 14.7% |
| Outpatient | $5.5 | 18.3% | $5.04 | 17.3% | $7.31 | 21.8% |
| Professional | $6.1 | 20.3% | $5.68 | 19.5% | $7.77 | 23.2% |
| Drugs | $4.2 | 14.0% | $4.22 | 14.5% | $4.14 | 12.3% |
| Other | $1.5 | 4.8% | $1.15 | 3.9% | $2.62 | 7.8% |
| Medical subtotal |
69.5% | 66.5% | 79.8% | |||
| Administration | –$0.1 | –0.2% | –$0.39 | –1.3% | $1.20 | 3.6% |
| Taxes and fees | $9.0 | 29.9% | $9.93 | 34.1% | $5.45 | 16.2% |
| Profit | $0.2 | 0.7% | $0.22 | 0.8% | $0.12 | 0.4% |
| Nonmedical subtotal |
30.4% | 33.6% | 20.2% | |||
| Total premium increase, PMPM |
$30.1 | $29.16 | $33.54 |
Note: PMPM = per member per month.
Source: Authors’ analysis of Uniform Rate Review data from the Centers for Medicare and Medicaid Services.
Seventy percent of the premium increase overall resulted from growth in medical costs; 30 percent was from overhead and profits (Exhibit 3). Less than half of the medical cost increase is attributable to hospitals; the remainder is attributable to physicians, drugs, and other expenses. These percentage components are roughly the same on and off the exchanges, with any differences being difficult to interpret based on available information.
The nonmedical component of the 2015 premium increase was driven almost entirely by government fees and taxes, rather than by profits or administrative costs. About half of this increase in taxes is attributable to the fees that exchanges began to charge in 2015, and the other half appears to be taxes that affect all products. These new fees should affect premium increases for only one year, after which they will become part of insurers’ base rates.
Conclusion
The Affordable Care Act’s market reforms appear to be working well in the individual market, both on and off the exchanges. On a national level, we see little indication that risk segmentation is causing adverse effects in either market segment. All the major plan types (bronze, silver, gold) are being actively sold in both market segments, and general patterns of medical cost increase are similar in each segment. Of note, nonmedical overhead appears to differ. Insurers that sell only off the exchanges project that a higher percentage of total premium dollars will go to overhead and profits than do insurers that sell only on the exchanges—a testament to the exchanges’ ability to sell coverage efficiently.
How This Study Was ConductedData for this analysis come from the “unified rate review template” (URRT) spreadsheets for 2015; insurers must file these with the Center for Medicare and Medicaid Services’ Center for Consumer Information & Insurance Oversight to document how they develop premium rates for Affordable Care Act–compliant plans. The URRT includes two sections: the market-level analysis section, which develops the projected single risk pool rate from prior experience data, and the product/plan section, which reports the projected premiums and enrollment for the coming year in each health plan. This database provides the change in premium per member for plans offered on and off the exchanges, as well as the types of medical claims (e.g., inpatient or outpatient) and administrative costs driving premium changes. There were 570 unique insurers in different states. For measuring the components of premium increases, we analyzed 1,060 product lines that existed in both 2014 and 2015, weighted by insurers’ projected 2015 membership in each product. We also used projected membership to classify insurers and products as selling predominantly on the government exchanges versus off the exchanges. For plans sold on exchanges, insurers must also offer these plans off the exchanges. Therefore, some on-exchange plans also have off-exchange enrollment. However, because the majority of enrollees receive subsidies that are available only through the exchanges, enrollment in these plans is predominantly on-exchange; therefore, the exchange dynamics determine the pricing of these plans even when sold off-exchange. |
Notes
1 States could, if they chose to, require insurers to sell through the exchanges, but so far only Washington D.C. has done so.
2 Some small employers may also claim a tax credit for coverage purchased through the SHOP (Small Business Health Options Program) exchanges, but limitations on this tax credit have resulted in only a small fraction of employers doing so. U.S. Government Accountability Office, “Small Business Health Insurance Exchanges: Low Initial Enrollment Likely Due to Multiple, Evolving Factors” (Washington, D.C.: GAO, Nov. 2014).
3 T. S. Jost, Health Insurance Exchanges in Health Care Reform: Legal and Policy Issues (New York: The Commonwealth Fund, Dec. 2009).
4 However, insurers still may maintain separate risk pools in different states, between the individual and small-group markets, and between ACA-compliant versus grandfathered coverage.
5 These data do not include grandfathered or other noncompliant plans that people have renewed from prior to 2014. In 2014, such plans accounted for roughly a third of individual market enrollment. L. Hamel, M. Norton, L. Levitt et al., Survey of Non-Group Health Insurance Enrollees (Menlo Park, Calif.: Kaiser Family Foundation, June 2014). That proportion is expected to diminish substantially each year, however. J. Appleby, “Canceled Health Plans: Round Two,” Kaiser Health News, Oct. 2, 2014.
6 As explained in the “How This Study Was Conducted” box, however, ACA-compliant plans sold predominantly on-exchange also can have some off-exchange enrollment. Therefore, our projected percentages are not precise market shares. Nevertheless, the 21% we measure is similar to the off-exchange enrollment of 24% reported for 2014, and 26% for 2015, based on a representative survey (rather than on comprehensive enrollment data). Hamel, Norton, Levitt et al., Survey of Non-Group, 2014; L. Hamel, M. Norton, L. Levitt et al., Survey of Non-Group Health Insurance Enrollees, Wave 2 (Menlo Park, Calif.: Kaiser Family Foundation, May 2015). These estimates are smaller than estimates by others that also include “grandfathered” plans that are non-ACA-compliant sold off-exchange.
7 McKinsey Center for U.S. Health System Reform, Hospital Networks: Evolution of the Configurations on the 2015 Exchanges (Washington, D.C.: McKinsey and Company, April 2015).
8 J. Geneson and K. Coleman, “Cheapest Plans from Major Off-Exchange Companies Over 40% More Expensive Than Cheapest Exchange Plans” (June 2014), http://www.healthpocket.com/healthcare-research/infostat/off-exchange-vs-on-exchange-premium-comparison.
9 Hamel, Norton, Levitt et al., Survey of Non-Group, 2014; Hamel, Norton, Levitt et al., Survey of Non-Group, Wave 2, 2015.
10 These are simple, unadjusted loss ratios, that do not take account of several factors allowed by the ACA’s minimum loss ratio regulation.
11 S. J. Dash, J. Giovannelli, K. Lucia et al., “State Marketplace Approaches to Financing and Sustainability,” The Commonwealth Fund Blog, Nov. 6, 2014.
12 J. T. O’Connor, Comprehensive Assessment of ACA Factors That Will Affect Individual Market Premiums in 2014 (Milliman, April 2013). Moreover, states that operate their own exchange often use broader-based fee structures that reduce fees paid on the exchange by imposing fees also off-exchange. Finally, because both this fee structure and the reporting template are new, it is also possible that the exchange fees are not being fully or accurately reported. Therefore, it will be important to repeat this analysis in subsequent years, when data integrity is better established.
13 These are not actual premium “rates,” however, because they do not account for any changes projected in the age of subscribers. Actual premium rate changes have been reported previously, for exchange products. J. R. Gabel, H. Whitmore, S. Stromberg et al., “Analysis Finds No Nationwide Increase in Health Insurance Marketplace Premiums,” The Commonwealth Fund Blog, Dec. 22, 2014.



