Abstract
- Issue: A persistent concern about health insurance coverage expansions is that the supply of care providers is already so constrained that any increase in service use would reduce the quality of care for all Americans. Based on the experience of the Affordable Care Act (ACA) expansions, is this concern valid?
- Goals: Assess changes in the content of primary care visits, comparing the pre- and post-ACA periods.
- Methods: Analysis of the National Ambulatory Medical Care Survey, 2006–2016.
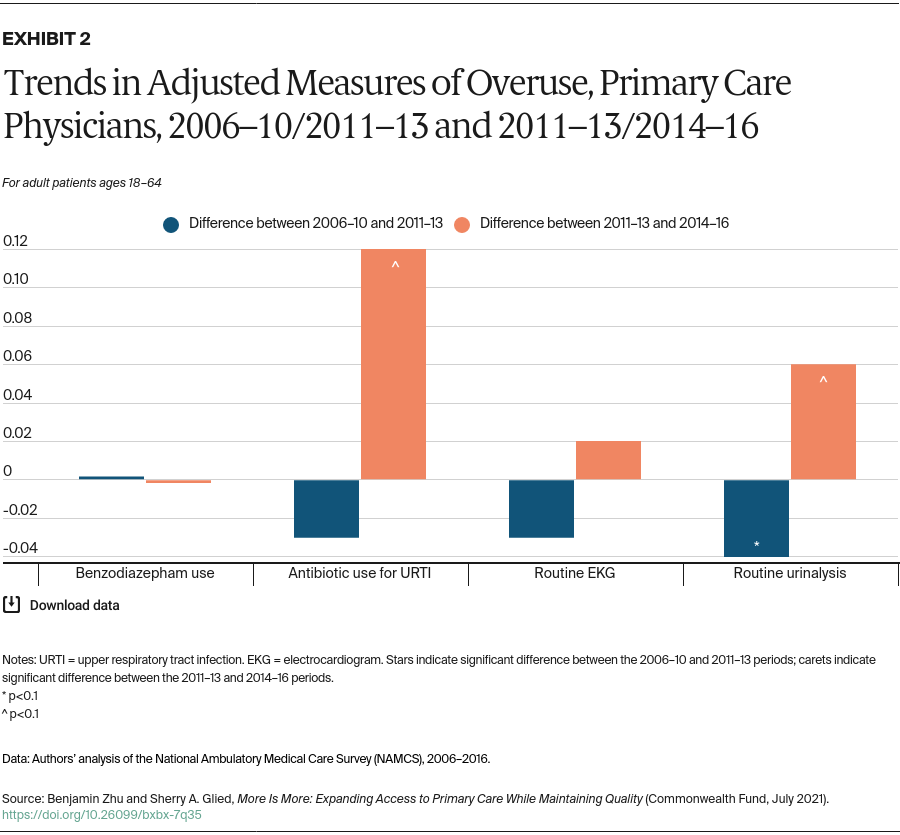
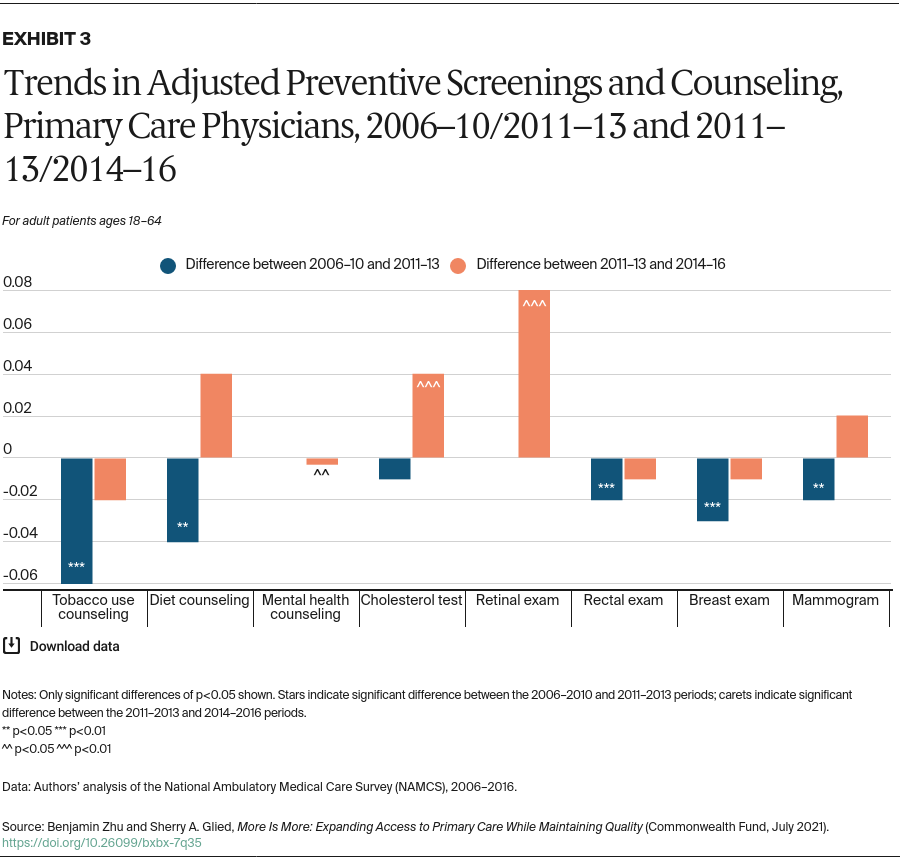
- Key Findings: The duration of physician visits, a direct measure of supply constraints, has increased substantially since 2006. While the Choosing Wisely campaign appears to have led to modest reductions in the provision of unnecessary care when it first rolled out, these effects have since been reversed. Rates of preventive screening and counseling saw a general pattern of decline between the 2006–2010 and 2011–2013 periods, followed by recovery in 2014–2016.
- Conclusion: The primary care system has been able to absorb increases in utilization generated by the ACA without jeopardizing care quality or intensity. There is also evidence that further expansions in demand can be accommodated, as providers in the post-ACA period have not reduced use of inappropriate or unnecessary care.
Introduction
Not all states have yet expanded Medicaid, although the American Rescue Plan offers inducements to do so. Opponents of coverage expansions have raised concerns about supply shortages, rehashing an argument common at the time the ACA was passed.1 At that time, against the background of an already strained primary care system, several estimates suggested that the demand for additional primary care would require substantial increases in the number of providers,2 though other studies anticipated that the existing supply would be sufficient to meet the new demand.3
Similar concerns have been raised in the debate on a single-payer health plan for the United States. The Congressional Budget Office, in its cost estimates, assumes that providers would rapidly adjust supply to meet the increased demands under such a plan.4 In contrast, some analysts believe that supply increases would accommodate only a portion of the increased demand, implying that the costs of such a plan would be lower than the CBO expects.5
Since implementation of the ACA, several studies have examined the relationship between coverage expansions (mainly Medicaid expansions) and provider availability. Some find that provider availability was not affected by coverage expansions, while others, primarily early studies, find some evidence of limits on availability.6 These studies generally focus on specific populations in particular areas. Most examine the Medicaid expansion, rather than the impact of the combined Medicaid expansion and marketplace subsidies.
Another set of studies has examined the relationship between the Medicaid expansion and the quality of care provided to patients, mainly focusing on surgical care and community health centers. Most find either improvements or no effects, suggesting that these components of the health system have been able to absorb the additional demand generated.7
To date, there has been no assessment of how the quality of primary care more generally has changed since ACA implementation. We build on the existing literature to describe how the primary care experience for all adult patients under age 65 has changed as the coverage expansions have taken place.
A robust literature has used nationally representative data on physician office practice to assess changes in the quality of primary care over time. Most find that quality metrics were stable or improving in the pre-ACA period, 1996–2010. Ma and Stafford compared 23 outpatient quality indicators in 1992 and 2002 and found generally modest changes, with significant improvements in six of the indicators.8 Edwards et al. examined trends across 25 quality indicators, comparing the 1997–2003 period to the 2004–2010 period, finding significant improvements in 10 indicators and deteriorations in seven.9 Levine et al. compared nine quality indicators between 2002 and 2013 and found improvements in four indicators and deteriorations in two.10
In this analysis, we update these estimates using the 2006–2016 National Ambulatory Medical Care Survey (NAMCS), the main data source used in prior studies. (For more detail, see “How We Conducted This Study.”) Our analysis ends in 2016 because the NAMCS substantially changed its sampling frame and methods in the 2017 survey, which is not yet publicly available and will not be fully comparable to prior versions of the survey.
We examine four dimensions of quality of care:
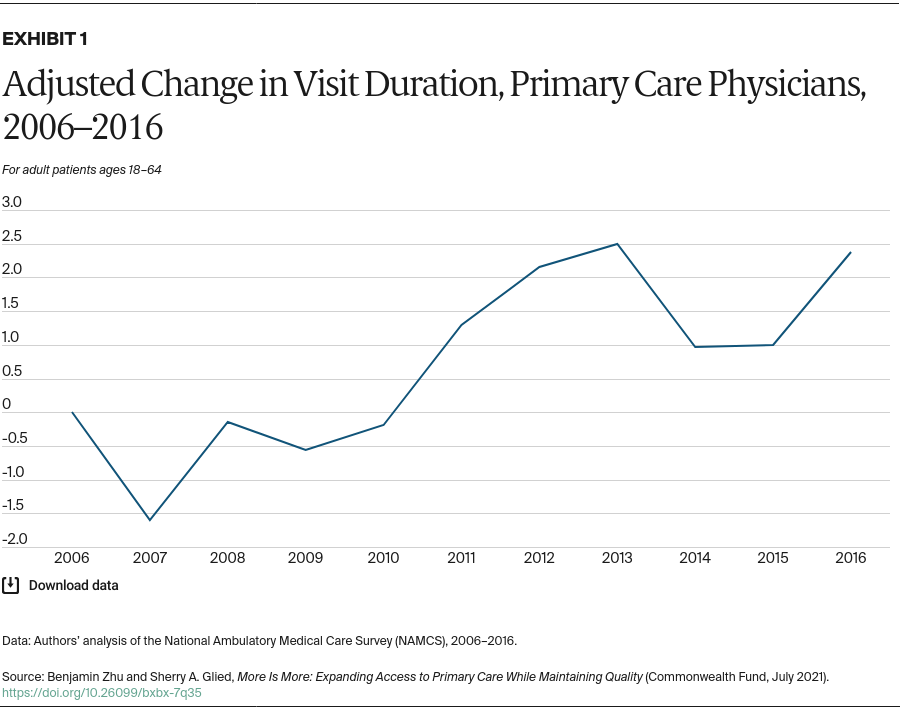
- Duration of clinician visits. If coverage expansions put pressure on clinicians to address growing demand, physicians might shorten average visit duration.
- Use of unnecessary care. Over this period, there have been deliberate efforts to reduce inappropriate care. In 2012, the American Board of Internal Medicine Foundation began the Choosing Wisely campaign to promote dialogue between clinicians and patients and empower patients to choose care that is evidence-based, necessary, and appropriate.11 If clinicians responded to the growing demand for services by cutting back on unnecessary care, there should be improvements in this dimension.
- Preventive screenings. The ACA expanded access to preventive screenings for people already insured, by eliminating cost sharing for key preventive services beginning in 2010, and through coverage expansions. To the extent that patients responded to the elimination of cost sharing, we would expect a larger share of clinician office visits to include preventive services.
- Receipt of guideline-concordant care. Guidelines for care are constantly changing as new treatments are developed and new evidence is brought to bear around existing treatments. We build on existing research, looking at guidelines for specific conditions, assessing changes in the underlying prevalence of conditions, and identifying changes in the treatments prescribed to patients with these conditions over time. The most prominent change in guidelines was the expansion of statin recommendations in 2013, which added 13 million Americans to the eligible population.12 We apply a broad definition of visits that are eligible for a statin and, to the extent that the change in guidelines led to an increase in statin prescribing, would expect increases in the rate of statin prescribing.
Key Findings
Visit Duration
The duration of physician visits is the most direct measure of supply constraints. If doctors are overbooked, they are likely to cut back on visit length. Primary care visit length increased substantially, to a recent high of 25 minutes, through 2013 (Exhibit 1). Immediately after implementation of the coverage expansions, visit duration fell by about 1.5 minutes, though it remained well above the 2006–2010 average. By 2016, visit duration had bounced back to about the level recorded in 2013. This pattern is consistent with the data on access to care, which found some evidence of access problems immediately after coverage expansion implementation, followed by an easing of these problems.