Enabling Conditions for ACOs in Medicaid
Based on our interviews, we identified several factors that enabled states to introduce ACOs in their Medicaid programs. First, Medicaid and health system leaders alike underscored the need for flexibility, both from the Centers for Medicare and Medicaid Services (CMS), which establishes conditions under which ACOs are permitted in Medicaid, and from Medicaid agencies, which can allow multiple pathways for providers to participate. For example, states could allow providers with less capacity to bear risk to begin with “upside only” contracts rather than require all ACOs to share in losses from the start (this approach was used in Maine and Vermont, for example).
Leadership was also viewed as an essential ingredient in bringing forth an ACO program. Two respondents noted that visible support for ACOs in the governor’s office was critical for their adoption. One respondent highlighted the importance of leaders being able to articulate a vision for ACOs that could be embraced by a wide range of stakeholders, including providers, patients, and taxpayers.
ACOs are predicated on the idea that providers can effectively manage population health when incentivized to control costs and improve the quality of care. But beyond these incentives, data and analytic capabilities are a prerequisite for effectively administering ACOs and identifying opportunities for improving patient care and reducing waste.6 Medicaid leaders in states that have not yet adopted ACOs pointed to the challenge of making sense of fragmented data as a rate-limiting factor, while nearly all respondents in states with ACOs cited success in aggregating data for clinical use, such as a list of patients who are due for cancer screening, as an important first step in transforming care delivery.
We always say we’re drowning in data and starving for information, so we have now hired a team of data analysts who are making sense of it all. . . . [We hope] our health centers can then use [these data] to drive performance at the local level.
— Health system leader in state with Medicaid ACOs
Respondents also highlighted that ACOs are natural extensions of “advanced” primary care programs like patient-centered medical home (PCMH) recognition and reward programs. PCMH programs seek to foster “safe, high-quality, affordable, and accessible patient-centered care by promoting stronger relationships with patients, addressing care needs more comprehensively, and providing time to coordinate care across all sectors of the healthcare system.”7 Federal, state, and multipayer initiatives over the past decade have promoted the adoption of PCMH models of care through up-front payments, technical assistance, and collaborative learning networks. Primary care providers that have benefitted from these programs — especially federally qualified health centers (FQHCs) — are better equipped to participate in ACOs, particularly in terms of workforce readiness and information technology capacity. Similarly, state Medicaid agencies that have experience with PCMH programs or any kind of value-based payment report they are better prepared to design and negotiate ACO arrangements, identify and address challenges, and manage costs and quality.
Pay-for-performance and other commercial value-based purchasing is also sort of in the DNA, in that it’s been around for a while. So people are kind of used to the idea of standardized quality measures and performance incentives.
— State Medicaid leader where ACOs have been implemented
It came as no surprise that early Medicaid ACO adopters identified some kind of “burning platform” as a key catalyst. While we heard about longstanding dissatisfaction with fee-for-service payment among all interviewees, a more immediate crisis or opportunity prompted some states to adopt ACOs while others remained on the sidelines. Some states were mobilized by the prospect of unsustainable costs because of Medicaid expansion, and others by the possibility of receiving time-limited federal funding, such as Delivery System Reform Incentive Payments or State Innovation Models Initiative payments.8
The ACO model is a substantial departure from the fee-for-service status quo. It involves uncertainty and risk of financial loss, so a history of productive collaboration — between Medicaid agencies, providers, and any MCOs that are involved — increases the willingness of providers to participate in voluntary ACO initiatives. Contracting details such as risk adjustment, specification of performance measures, and the division of losses and savings can have dramatic consequences and it may not be easy for providers to forecast what combination of parameters will provide the best balance of opportunities and risks. In light of these uncertainties, health system leaders highlighted both trust and transparency as critical to effective collaboration with their Medicaid counterparts.
Barriers to ACO Adoption
In states that have not adopted policies to institute ACOs, Medicaid leaders cite competing priorities as a key reason. Medicaid leaders in two states indicated they had been taking steps to implement an ACO program prior to the COVID-19 public health emergency and the introduction of major policies that changed how Medicaid is administered through the introduction of MCOs. Both states expect to launch their ACO programs in the near future.
Respondents in both ACO and non-ACO states identified complex, prescriptive federal regulations as a barrier to ACO adoption and optimal design. This includes the CMS section 1115 demonstration process, which is one regulatory pathway through which state Medicaid agencies can test new payment models. For example, CMS has recently articulated a framework for approving 1115 demonstrations that loosens budget neutrality requirements but limits the total dollar amount that can be spent on these services and requires states to meet provider payment rate standards.9 Some respondents suggested that meeting the new requirements could be challenging despite the relaxation of budget neutrality.
Not all states use 1115 demonstrations to introduce ACOs; some states have opted instead to use State Plan Amendments, which are agreements between a state and the federal government that govern how a state administers its Medicaid program. However, reforms put forward through this pathway must be statewide, offer comparable services, and free choice of provider, which may preclude more limited pilots or efforts to test competing models.
Several respondents noted that federal rules related to FQHC payment caused confusion about how these entities — which are an important part of the Medicaid delivery system — could be included in ACO programs.
Both the literature and our interviews suggest that resistance from other entities involved in administering Medicaid benefits, including local governments and MCOs, can complicate ACO implementation. In particular, implementing ACOs in environments where decision-making is more decentralized or delegated can be difficult because of divergent interests. For example, in some county-administered programs — where the county is a provider through safety-net hospitals — the state and county government Medicaid authorities may have different views on ACOs. Likewise, MCOs that operate in multiple states might seek to standardize contracts across states rather than customize to each state.
It is worth noting that some states that do not currently have ACOs have adopted other population- or value-based payment models.10 One respondent made it clear that their state’s goals of improving quality and equity were tied to a different alternative value-based payment model and the state had no intention of pursuing ACOs because of a question of fit.
Factors That Amplify the Benefits of ACOs
In a health system with multiple payers, such as government and private insurers, the impact of a payment model like ACOs will depend in part on the share of providers’ revenues governed by that contract. For example, if 10 percent of a provider’s patients are covered by ACO contracts and 90 percent are reimbursed using traditional fee-for-service, there will be less incentive to invest in systems to control cost and improve quality. Thus, the presence of larger shares of Medicare and commercially insured patients cared for under ACO contracts should amplify the effects of Medicaid ACOs. The need for comprehensive community engagement in the design of ACO programs and their ongoing oversight was another theme. Addressing health-related social needs necessitates collaboration with community-based organizations, which requires Medicaid ACOs to build bridges beyond the health care sector.
Finally, Medicaid agency respondents noted that states implementing ACOs through MCOs need to ensure their providers are not faced with multiple ACO incentive structures because such fragmentation increases administrative costs and dilutes incentives. Health system interviewees likewise suggested that providers were wary of participating in Medicaid ACO programs where individual MCOs had broad discretion to design their own contracts. Some states mitigated fragmentation by requiring exclusive arrangements between MCOs and providers or creating a single ACO program that is administered identically by all MCOs in a region.
Conclusion
The literature and key informant interviews bring into relief several key insights about Medicaid ACOs. States with advanced primary care, a history of value-based purchasing, and a compelling mandate for change are fertile ground for ACOs. And upfront investments in data and delivery system transformation can help their ACOs succeed — whether this is from new federal funds, states, or MCOs. It is also clear that providers cannot effectively respond to multiple, diverging incentive models, so state policymakers need to either centralize or coordinate ACO contracts in multipayer and managed care environments. Finally, broader adoption of ACOs in Medicaid may require additional flexibility from CMS for states to build models that meet local needs and provider capabilities.
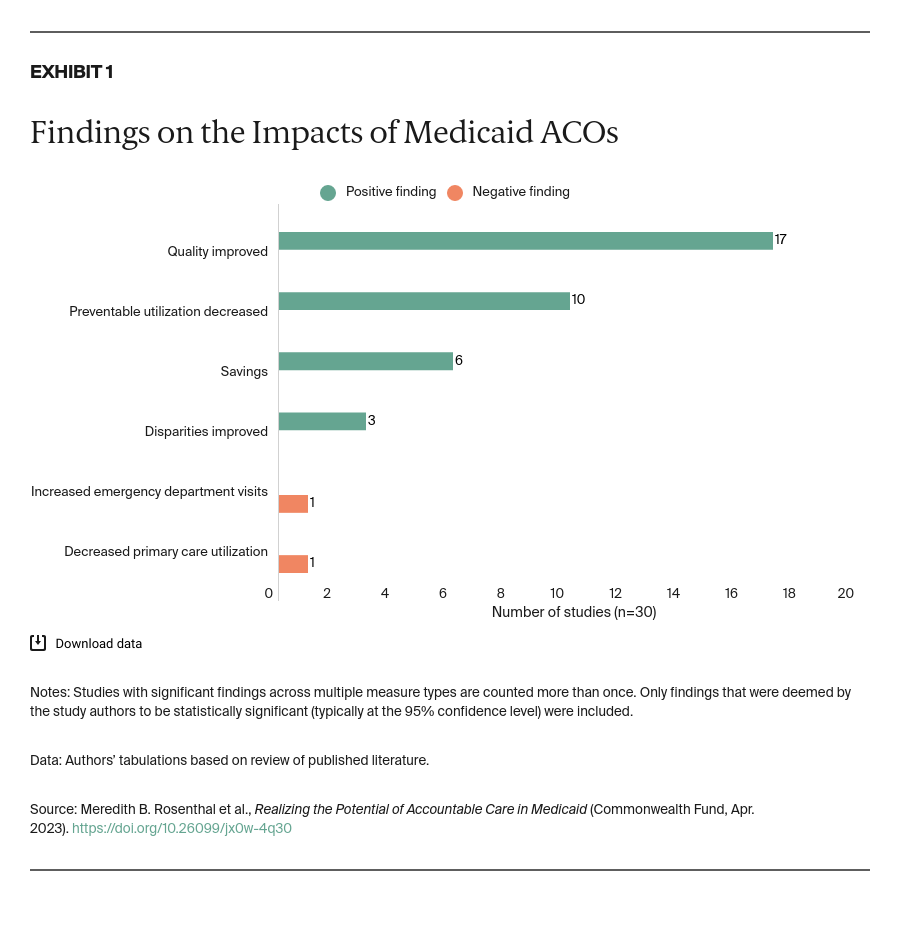
Relatively few Medicaid ACO programs have been the subject of controlled studies and this lack of a strong evidence base is a barrier to effective policymaking. The extant literature suggests that ACOs can improve health care access and quality overall, and, in some cases, simultaneously improve equity. But more research is needed, particularly on how specific aspects of ACOs lead to improvements in health and health care among marginalized groups. For example, how have Medicaid ACOs been able to increase primary care use among Black patients? These insights also may have salience for the recently launched ACO Realizing Equity, Access, and Community Health model for Medicare beneficiaries, which specifically targets equity both in the selection of participants and the model requirements.
Federal policymakers have a number of opportunities to support state innovation in the ACO space. First, CMS should consider whether the 1115 demonstration approval process and requirements for ACO initiatives can be streamlined to lower the barriers to entry and allow states to tailor ACOs to their contexts. A more expedited review process could also be beneficial. Demonstration approvals can take as long as a year, making it hard for states to maintain momentum and stakeholder engagement. Second, CMS should continue to offer information and shared learning opportunities for Medicaid decision-makers, including clear guidance on common stumbling blocks such as federal rules that limit downside risk sharing with FQHCs. Finally, in states where both Medicaid agencies and providers have comparatively limited resources, new federal funds could jumpstart ACO implementation and support rigorous evaluation.