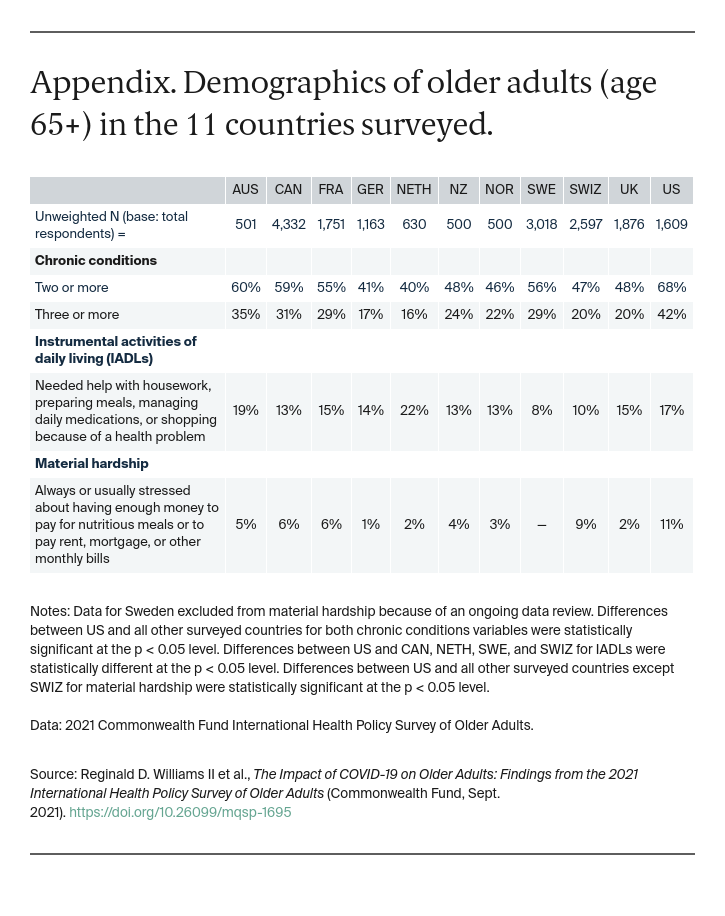
The 2021 Commonwealth Fund International Health Policy Survey of Older Adults was conducted from March 1 to June 14, 2021, by SSRS, a U.S. survey research firm, and contractors in the other countries. The survey was administered to a nationally representative sample of adults age 65 and older in Australia, Canada, France, Germany, the Netherlands, New Zealand, Norway, Sweden, Switzerland, and the United Kingdom and of adults age 60 and older in the United States.
A total of 18,477 interviews of adults age 65 and older were completed for the 2021 survey. The full U.S. sample included 360 adults ages 60–64 or who reported being older than age 60 but did not give an exact age. These responses were not included in this analysis. Final country samples (age 65 and older) ranged from 500 to 4,332. Interviews were completed either online or using computer-assisted telephone interviews.
In Australia, France, Germany, the Netherlands, New Zealand, Norway, the United Kingdom, and the United States, samples were generated using probability-based overlapping landline and mobile phone sampling designs. Both mobile and landline telephone numbers were included to improve representativeness. The sample in Canada was generated using a probability-based landline-only sampling design. Standard within-household selection procedures were used to increase the likelihood of reaching an eligible respondent for landline samples.
In Germany, respondents were randomly selected from a public list of phone numbers, landline as well as mobile phones, flagged as belonging to households with at least one adult age 65 or older. In Norway, respondents were randomly selected from a listed registry, and interviews were completed via landline and mobile phones. In Sweden and Switzerland, respondents were selected via nationwide population registries, recruited via postal mail, and invited to participate in an online or phone version of the survey.
A common questionnaire was developed, translated, adapted, and adjusted for country-specific wording as needed. Not all questions were asked in each country (noted in the exhibits). Interviewers were trained to conduct interviews using a standardized protocol. Response rates varied from 7.2 percent in the United Kingdom to 47.7 percent in Switzerland.
International partners joined with the Commonwealth Fund to sponsor surveys, and some countries supported the use of expanded samples to enable within-country analyses. Data were weighted to ensure that the final outcome was representative of the adult population in each country. Weighting procedures considered the sample design, probability of selection, and systematic nonresponse across known population parameters including region, sex, age, education, and other demographic characteristics deemed consistent with standards for each country. In the U.S., the weighted variables also included race and ethnicity.
The margin of sample error for the 2021 International Health Policy Survey of Older Adults was approximately +/– 2 percent for Canada and Sweden; +/– 3 percent for France, Germany, Switzerland, and the United States; +/– 4 percent for the Netherlands and the United Kingdom; +/– 5 percent for Australia and New Zealand; and +/– 6 percent for Norway, all at the 95 percent confidence interval.
Acknowledgments
The authors thank Robyn Rapoport, Sarah Glancey, Rob Manley, and Christian Kline of SSRS, as well as Chris Hollander, Jen Wilson, and Paul Frame of the Commonwealth Fund.