Introduction
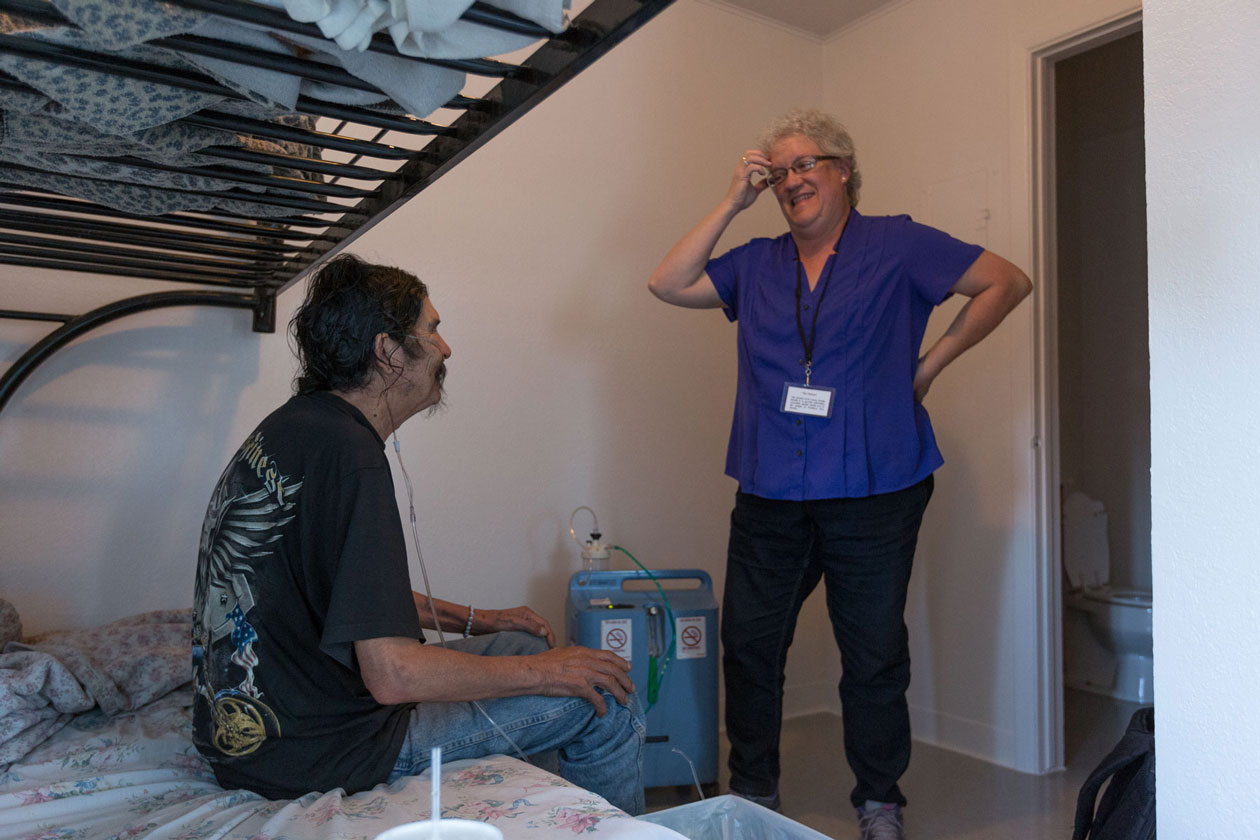
By the time Mark reached his early 40s, years of alcohol abuse had almost killed him. On the day he first met with Chris Ruge, a nurse practitioner in New Mexico, Mark was incoherent, with 20 pounds of fluid in his abdomen a clear sign that his liver had nearly stopped working. Ruge called 911, and Mark spent four weeks recovering in an ICU and skilled nursing facility. He was unable to walk and barely able to talk when he was discharged, but started drinking again within days.
Ruge and his care team are throwing lifelines to Medicaid beneficiaries like Mark — the “superutilizers” who accrue very high health care costs because of their addictions, mental illness, and physical health problems, which are often compounded by poverty and social isolation. To help Mark, Ruge spent hours with him. “We didn’t talk about medical stuff,” he says. “I just talked to him about his life and asked whether he wanted to stick around.” After several such conversations, Mark told Ruge he was ready to get sober, and asked for help.
Ruge and his colleagues are guided in this work by experts at the University of New Mexico’s Project ECHO (Extension for Community Health Outcomes) program, which for more than a decade has been using telehealth to support primary care clinicians caring for complex patients in underserved communities. In Project ECHO’s latest effort, the experts are training five primary care teams in the field via regular videoconferences to offer therapy and medication to treat patients’ mental illnesses and addictions, provide hands-on support in managing their physical health problems, and connect them with housing and other social supports to stabilize their lives.

But Ruge believes the team’s key point of leverage is building trusting relationships with patients. “We’re able to open those doors a crack and give them some hope, and show them some alternatives,” he says.
Ruge’s team is one of five working across the state, part of this complex care initiative launched in 2013. This profile describes the work, focusing on two primary care teams: one in the Southeast Heights neighborhood of Albuquerque, and the other serving the rural community of Las Vegas, New Mexico.
Project Echo’s Target Population
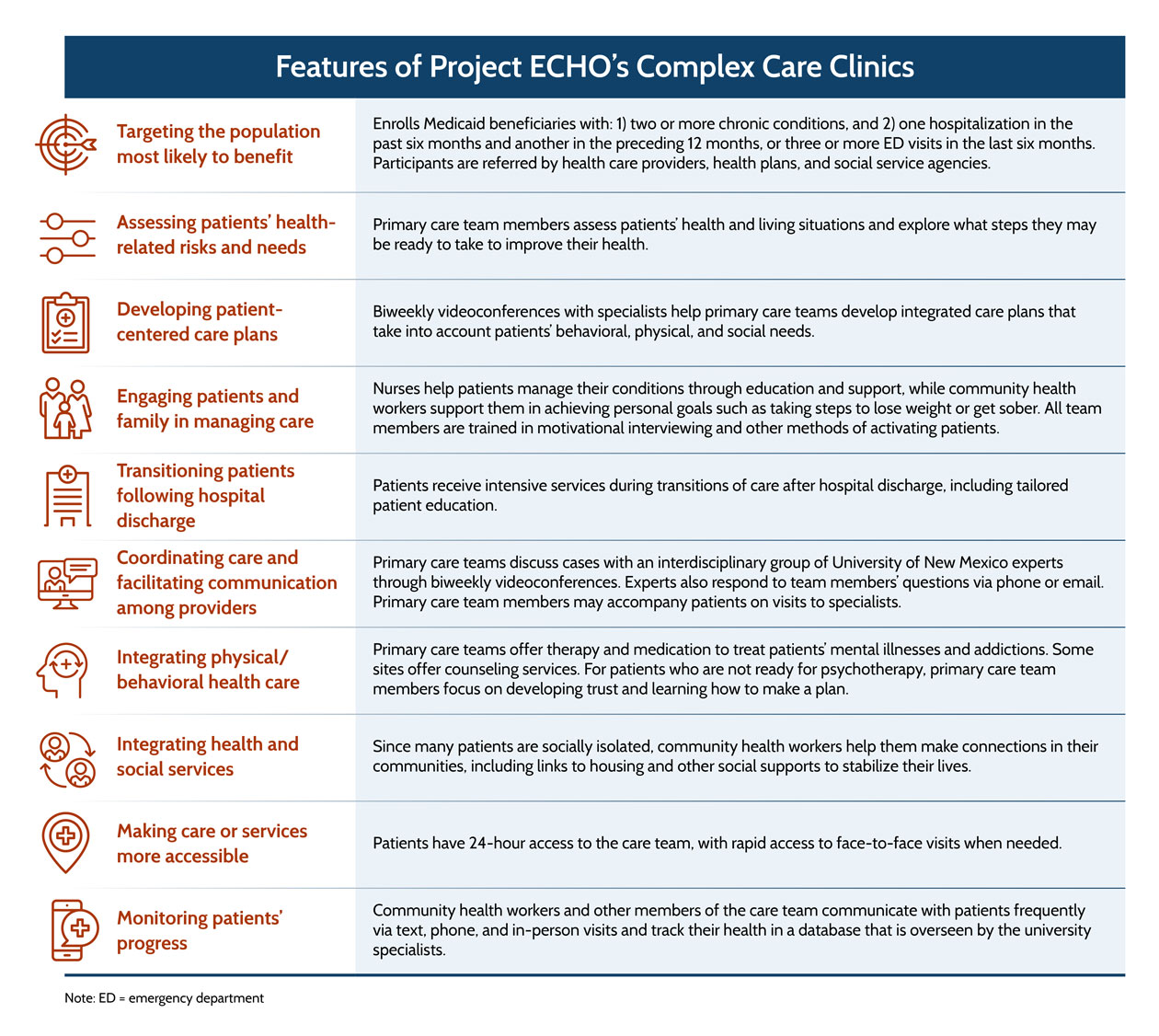
The complex care initiative targets Medicaid beneficiaries who incur very high costs due to substance abuse problems and/or mental illnesses, often accompanied by significant physical health problems. Most of the 425 current participants in the program received Medicaid coverage under New Mexico’s 2014 expansion to cover poor, childless adults. Because the ECHO team is working with all four of the state’s Medicaid managed care plans, and because nearly all of New Mexico’s beneficiaries are enrolled in managed care, participants are drawn from the vast majority of the state’s adult Medicaid beneficiaries. (New Mexico Medicaid decided to exclude those who are dually eligible for Medicaid and Medicare, since any savings from reduced hospitalizations would accrue to Medicare.) “The unifying characteristic is that they’re considered extremely difficult to care for,” says Miriam Komaromy, M.D., Project ECHO’s associate director.
Leaders initially planned to use predictive modeling to identify patients most likely to be hospitalized — the key driver of cost — and invite them to join the program, but it proved too difficult to reliably contact this transient population. Instead, patients are referred by managed care plans, community health centers, emergency departments, and social service agencies if they:
- Have two or more chronic conditions (including physical conditions, mental health problems, or chemical dependencies) and
- Have been hospitalized in the past six months and in the preceding 12 months, or have had three or more emergency department visits in the last six months.
While many thousands meet these criteria, health plan care managers tend to refer the only the subset of patients they have not been able to engage, Komaromy says.
The Southeast Heights team is treating 107 patients in this poor Albuquerque neighborhood, mainly minorities as well as some refugees. Twenty-four are homeless or unstably housed. The Las Vegas team serves 81 mostly Hispanic patients, including one homeless person. Many were released from the town’s state psychiatric hospital decades ago, as part of efforts to deinstitutionalize mentally ill patients, and remained in Las Vegas because they had nowhere else to go.
Key Program Features
Interdisciplinary Teams That Support Patients and Each Other
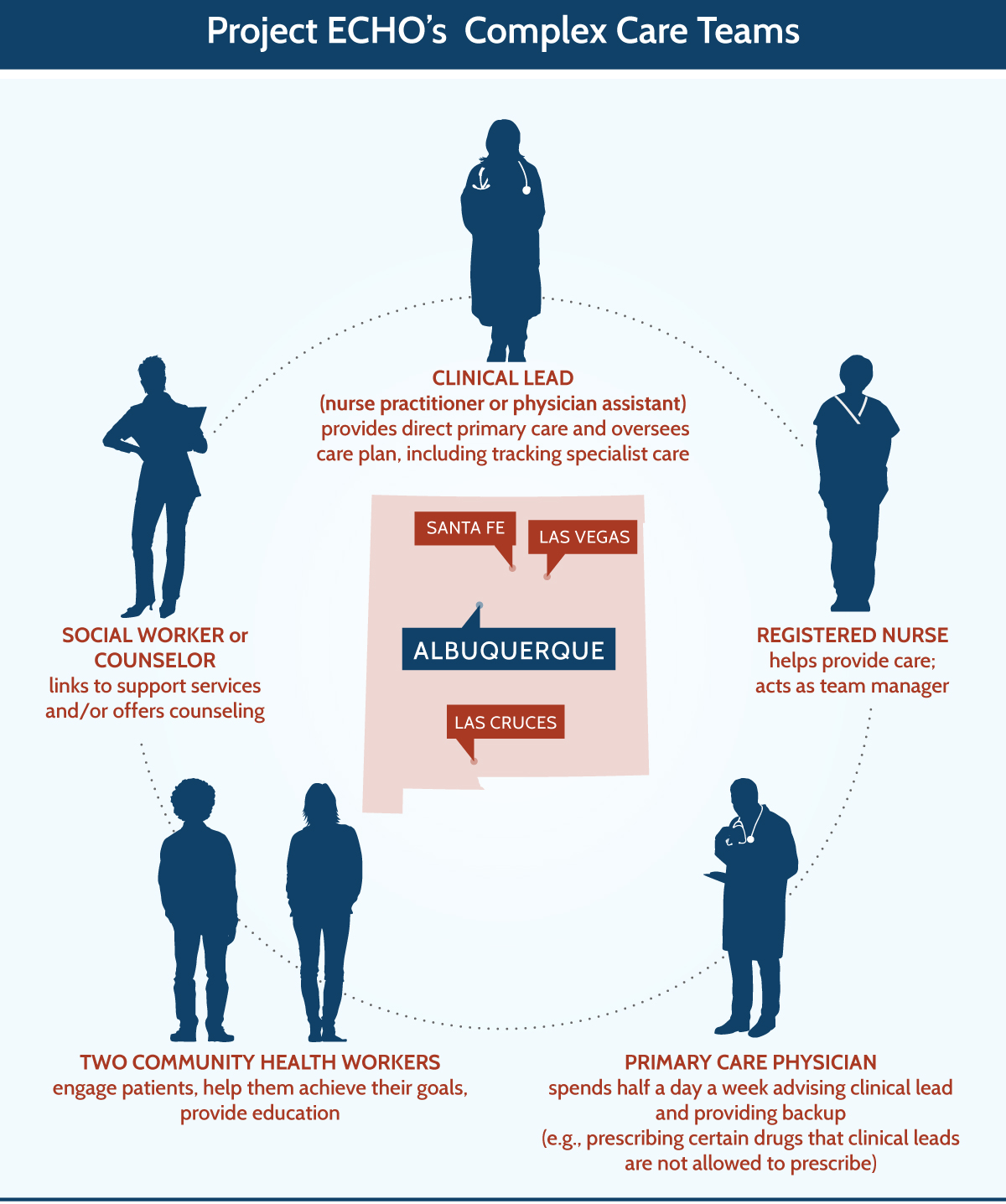
Five interdisciplinary teams work in regions of the state where there are sufficient numbers of high-cost patients: three of the teams are in Albuquerque and the others are in Las Vegas, Santa Fe, and Las Cruces. The four Medicaid managed care plans pay team members’ salaries, and the plans’ care managers liaise with the teams in the field to offer background on patients and other support. The teams are based at community primary care clinics, but they work as autonomous units, allocating their time and resources as necessary to address patients’ physical, behavioral health, and social needs.
Nurse practitioners or physician assistants, who have broad scopes of practice under New Mexico law, serve as each team’s medical lead. At each of the clinics, primary care physicians support each team by providing oversight and writing some prescriptions, including medications used for opioid withdrawal.
When enrolling patients, Ruge, the Las Vegas nurse practitioner, visits them in their homes to assess their health and living situation, and works with them to develop a care plan. Since patients have layers of social, behavioral, and medical problems, Ruge takes an incremental approach. “We explore with the patient what, if anything, they are willing to do today to decrease their risk and improve their health,” he says. This might include organizing medications in a pill box, scheduling overdue lab tests, starting counseling, or seeking ways to overcome stress. For patients on high doses of narcotics, Ruge makes clear that he won’t continue writing such prescriptions if he deems them medically unnecessary, but he will provide help in overcoming addiction. “Some people, at that point, just get up and walk out,” he says.
The nurse practitioners, physician assistants, and nurses help patients manage their conditions. Nurses offer education and hands-on support and provide guidance to the community health workers, who may be the first to notice a patient’s depressed appearance or learn of a new symptom.

Each team has two community health workers (CHWs) who make efforts to engage patients and build trust, often by finding tangible ways to improve their lives, such as getting a free cell phone. Over time, CHWs steer patients toward longer-term goals, such as taking steps to lose weight or get sober. Since many patients are socially isolated, CHWs help them make connections in their communities. For example, when Jeremy Estrada, a CHW in Las Vegas, learned one of his patients loves baseball, he began taking him along to the Little League games he coaches.
While ECHO’s leaders had planned to include social workers or counselors on the teams, this has not happened at all of the sites. (In Las Vegas, Ruge felt the team could rely on the primary care clinic’s staff counselors, while in Southeast Heights the team was unable to recruit a social worker or counselor willing to work in this untraditional way. The three other teams have included licensed mental health counselors, though not throughout the four years of the program due to staff turnover.) Instead, community health workers do some of the tasks traditionally done by social workers, such as signing people up for benefits. And even though nearly all of the patients have serious behavioral health problems, most “are not particularly ready for or open to traditional psychotherapy,” Komaromy says. Instead, they need to work on “developing trust, and learning how to make a plan — the kind of mental health care that can be delivered by a CHW or another member of the team,” she says.

Strategies for Engaging “Difficult” Patients
With a lot of people, there’s nothing to do in town. There’s no work. There’s no way to plug in, especially if they have an addiction history, then idle time means abusing one thing or another. So the CHW works with patients, finds out what their passions are, and what they’d like to do, and then walks them down that path.
These patients are often deemed “difficult to care for” by other primary care providers not just because their many needs cannot be addressed in a 15-minute visit, but because their addictions or mental illnesses can make them unpredictable, combative, rigid, or otherwise hard to deal with. Team members say their most challenging patients are those with personality disorders, who can be verbally abusive or manipulative. At the Southeast Heights clinic, team members meet with such patients in pairs to offer each other support and to prevent patients from pitting one team member against another.
Patients benefit from having personal and sustained attention. Many have lost touch with family members or friends, so they crave social connections, says Valarie Oldhorn, a Southeast Heights CHW who receives calls from some of her patients several times a week. “That phone call could eliminate an emergency room visit,” she says. “Someone may not really need to go to the ER, but they just want to talk to somebody.”
Team members have also found that offering help without judgment earns patients’ trust. “We show them that we're here for them in spite of their addiction,” says Hardgrave. Such an approach counterbalances the historic tendency of medical professionals to treat addiction as a character flaw rather than an illness. Team members also note the importance of understanding that many patients have had traumatic experiences.

Developing meaningful connections with patients means they may turn up at the clinics unexpectedly. Once, a patient came to the Albuquerque clinic in a psychotic state, threatening to shoot people. Following protocol, Oldhorn called an ambulance and the police. While she waited for their arrival, she talked calmly with the man. “We know these guys really well,” Hardgrave says. “It's not like a stranger who has to guess at what's going on. We've seen them at their worst. We know what their substance abuse preferences are, what they might have taken. I think because of that, they actually seek us out when they're in crisis because they know we're going to find them a safe place.”
Training and Support From Experts
The five primary care teams are supported by a large and varied group of experts at the University of New Mexico, including a psychiatrist; physicians specializing in addiction medicine, cardiology, chronic pain, endocrinology, gastroenterology, infectious disease, internal medicine, nephrology, and palliative care; a pharmacist; a counselor specializing in addiction treatment; and a community health worker. Project ECHO reimburses each of them for 0.1 of an FTE (one half-day per week), which covers their attendance at the two-hour biweekly videoconferences with the primary care teams, as well as the time they spend responding to team members’ questions via phone or email.

During the videoconference, the experts offer short presentations on subjects such as trauma-informed care, motivational interviewing, and addiction medicine. The primary care teams then take turns presenting their most challenging cases, and the experts offer their recommendations.
I can always come to the ECHO specialist and bounce it off of him. This is what their local cardiologist is doing. How does that jive with what his liver disease is doing?
Sometimes, the University of New Mexico experts, led by the counselor, help primary care team members by role-playing different approaches to engaging patients, such as one morbidly obese man facing respiratory failure who refused to change his diet or see a specialist. In the case of a heroin addict, the addiction medicine physician offered advice to his nurse practitioner on the use of Suboxone to wean him off of his dependency. This approach gives the primary care teams comprehensive care plans that take into account patients’ behavioral, physical, and social needs. “By getting everybody in one room, we can hash out a plan, rather than a disjointed referral system where I send them to one specialist after another,” Hardgrave says.
The teams also use the experts as a sounding board to review local specialists’ recommendations. “I often don’t get adequate feedback when I do send patients to a specialist’s office,” Ruge says. “And then I have certain questions that are unanswered.” For very ill patients — Ruge mentions those with advanced cirrhosis — the experts help review medication lists, steps to take as the disease progresses, and red flags. The University of New Mexico experts also share their cell phone numbers with the primary care teams, so they can offer advice for urgent cases.
The videoconferences also give primary care teams a chance to share their experiences with each other, helping to decrease the sense of isolation many providers feel when working in underserved or rural areas. And while the teams gain confidence in handling their complex patients, the specialists learn from the primary care teams’ on-the-ground experiences. “When we were piloting the complex care project, there was a real tendency for the specialists to give ‘lecturettes’ about ‘their’ organ system,” Komaromy says. “Over time that’s shifted. So we’ll hear specialists say things like, ‘There’s not really any point in trying to address the worsening kidney function until we can help to get this patient housed, so let’s focus on that first.’”
Financing
Project ECHO’s complex care initiative is funded through a public–private collaboration. In 2012, the University of New Mexico team received an $8.4 million grant from the Center for Medicare and Medicaid Innovation to support the administration of the project, development of training curricula, videoconferences, involvement of medical specialists, and evaluation. The grant support ended in June 2016.
New Mexico’s Medicaid agency required the state’s four managed care plans to participate in the initiative and to pay the salaries of the primary care teams. In each region, the plans contribute to team members’ salaries based on the proportion of their members who are enrolled.
Results
The primary care teams began enrolling patients in late 2013 and early 2014. ECHO’s leaders are tracking patients’ experiences through surveys and by monitoring their health care service use and outcomes in a database maintained by the primary care teams. Since finding a control group is difficult (given that enrollment is based on referrals), they are measuring the effects of this intervention through a pre/post evaluation. In the first 12 months, data show that the number of hospitalizations among participants fell by 27 percent and emergency department visits dropped by 32 percent. Preliminary findings suggest that per-member-per-month costs have also declined.
Patients report they have much better access to care and much better care experiences. After 12 months of enrollment, three-quarters (76%) said it was always easy to get the care they need, compared with 21 percent at baseline. While just a quarter (27%) of patients were very satisfied with their care at baseline, 87 percent reported being very satisfied after 12 months.
Insights and Lessons Learned
A primary care model providing hands-on support from dedicated teams, with guidance from a multidisciplinary group of experts, can improve health care outcomes and reduce costs for patients with serious behavioral and physical health problems. By helping patients make small changes to improve their lives, and by cultivating their trust over time, the primary care teams have been able to encourage behavior changes and stabilize patients’ conditions, preliminary results show. Community health workers have been key in this success. “If I were redesigning this I would probably add more community health workers and downplay some of the medical expertise,” says Komaromy. “Because the social and emotional aspects of the care are two of the most important things that we do.”
Staffing and supporting the primary care teams is difficult. In spite of their past experience working with high-need patients, team members have often experienced conflict, frustration, and turnover. Caring for this group of patients is extremely time-consuming and taxing: leaders initially planned for the teams to treat 250 patients, but soon realized that 125 was their maximum capacity. “One of the biggest challenges has been figuring out how to support the teams and avoid burn-out,” Komaromy says. “The most successful teams have been able to create a flatter structure than the usual medical hierarchy allows — one in which each team member’s strengths are maximized and members rely on one another.”
Sustaining this approach will require evidence of a business case, and spreading it may require partnerships with other payers, including Medicare. Preliminary results suggest that the reduced health care costs from this model of complex care may be more than sufficient to cover the salaries of the primary care teams. There may also be ways to achieve efficiencies that lower the costs of program administration, as described below. Given Medicaid plans’ reluctance to include dual eligibles, encouraging Medicare’s involvement — by aligning payers’ interests through a shared-savings model, for example — could encourage enrollment of a particularly high-cost group of patients who may benefit from the approach.
Next Steps
The Medicaid managed care plans had expressed interest in continuing this work after the grant funding ended and were even working with ECHO’s leaders to design a streamlined version of the program. However, recent cuts to the state Medicaid budget that were passed on to the plans led them to withdraw from contract negotiations.
In the coming months, ECHO’s leaders will have more complete data on the cost savings achieved. If these data confirm the preliminary evidence of substantial savings, they may apply for federal grant support to implement the program in other interested states. They are also hoping to develop narrower enrollment criteria and automatic referral of patients so they can establish a control group against which to measure the effects of this approach.
Project ECHO’s leaders also plan to share their clinical operations manual, training curriculum, and business plan, along with other components of the program, to encourage spread. In the meantime, Ruge’s patient, Mark, has been sober for 11 months; he continues to work with the team in Las Vegas to build his confidence and his health.

|
The authors would like to thank Jeremy Estrada, Clark Hardgrave, Miriam Komaromy, M.D., Valarie Oldhorn, and Chris Ruge who kindly provided information on Project ECHO’s complex care initiative. |