On June 28, 2021, the Biden administration proposed a rule that would make a hard U-turn from several of the Trump administration’s most controversial measures affecting the Affordable Care Act (ACA) marketplaces and health insurance markets more broadly.
Each year, the Centers for Medicare and Medicaid Services publishes a “notice of benefit and payment parameters” rule, which sets the ground rules for insurance plans and marketplaces for the following year. Typically, much of the rule is routine, addressing inflation updates, risk adjustment, and similar details. But it’s also been used to make significant policy changes in the administration of ACA programs and regulation of ACA health plans.
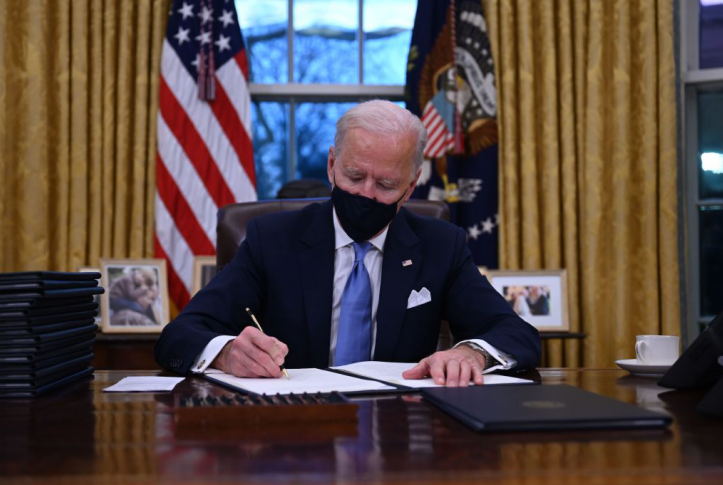
The Biden administration’s new proposed rule would reverse several controversial Trump-era changes in a partial payment rule published one day before Biden’s inauguration. The proposed rule also modifies other earlier Trump administration rules.
Several of the June 28 proposed rule’s provisions follow directly from Biden’s “Executive Order on Strengthening Medicaid and the Affordable Care Act.” The proposal also frequently relies on Biden’s “Executive Order on Advancing Racial Equity and Support for Underserved Communities Through the Federal Government,” explaining how the changes it is proposing would aid minorities and underserved communities.
State Innovation Waivers
Perhaps the most controversial changes affect the ACA’s section 1332 waiver program. Section 1332 allows states to request waivers from key provisions of the ACA to implement their own approaches to expanding individual and small-group coverage, if they satisfy certain guardrails.
In 2018 the Trump administration issued guidelines that significantly weakened these protections. These guidelines, which were finalized as regulation in January 2021, would have allowed states to count coverage that was not as comprehensive or protective as ACA coverage as meeting the guardrails, as long as ACA-compliant coverage were available to all. The Trump administration encouraged states to promote affordable private coverage over public insurance.
The Biden administration’s new proposal reinstates the Obama administration’s guidance. States would have to demonstrate that their proposed waivers would result in coverage as comprehensive and protective against excessive premiums and cost sharing as ACA coverage, and for at least as many people. States would also have to show that their proposal would not adversely affect vulnerable populations.
Other Reversals of Trump Policies
The Biden administration’s proposed rule would also prohibit states from using private entities like web brokers, insurers, or agents instead of public marketplaces to enroll individuals in ACA coverage. The Trump administration would have permitted this and, in fact, granted Georgia a waiver to pursue such a course. The new proposed rule voices concern that getting rid of public marketplace enrollment would adversely affect consumers, particularly vulnerable populations. Eliminating public marketplaces could cause consumer confusion, increase the likelihood that consumers would enroll in noncomprehensive plans, complicate coordination with Medicaid and the Children’s Health Insurance Program, and otherwise disrupt coverage.
In another dramatic change from Trump administration policy, the proposed rule would abolish the Trump “two bill” policy requiring insurers to collect a separate payment for abortion services. The Hyde Amendment prohibits federal funding for most abortions. Section 1303 of the ACA, therefore, requires insurers to keep separate accounts for the value of abortion coverage, which the enrollee must pay for, and of all other minimum essential coverage, which is partially funded by federal tax credits.
A Trump administration rule required insurers to bill separately and request a separate payment for abortion services. This policy was enjoined by the courts and never implemented. The proposed rule would reinstate the former rule, which allowed insurers alternative ways of complying with the 1303 requirement, as long as the enrollee was notified that the premium for abortion services was separate from the premium for other services.
Expanding Access to Coverage
The remaining provisions of the proposed rule focus on expanding access to ACA coverage, especially for vulnerable populations. Millions of people with household incomes up to 150 percent of the federal poverty level ($19,140 for an individual and $39,300 for a family of four) — many of whom are now temporarily eligible to enroll in free coverage under the American Rescue Plan Act — would be able to enroll in or change silver-plan coverage once a month. To keep people from waiting until they get sick and then enrolling, enrollment has traditionally been limited to an annual event; with free coverage, however, this is less of a concern.
The duties of navigators, who are receiving increased funding under the Biden administration, would expand to include counseling enrollees with issues they encounter after enrolling in plans. The open-enrollment period for 2022 and subsequent years would be expanded by a month to run until January 15, allowing people who are enrolled automatically to change plans after they receive their first bill. The user fees charged to insurers that use the federal marketplace, or state-based marketplaces that rely on the federal platform, would be increased to pay for the extra services the federal marketplace would provide, including expanded outreach.
In sum, after four years of Trump administration efforts to reduce the role of the ACA in providing health coverage, the new administration is proposing a clear reversal of course to once again rely on ACA plans and marketplaces to expand coverage.