The 2024 Medicare Physician Fee Schedule (PFS) proposed rule — the annual regulation determining payment and coverage policy for clinician services in traditional Medicare — includes several proposals designed to advance health equity and improve access to care. This blog post examines proposals focused on enhancing support for behavioral health services, health-related social needs, complex primary care, and caregiving through new provider payment and coverage policies. Together, these policies may help bolster the Medicare workforce, especially in behavioral health and primary care. Participating providers are in short supply in these areas and whole-person care that goes beyond clinical services often goes unpaid.
Behavioral Health Services
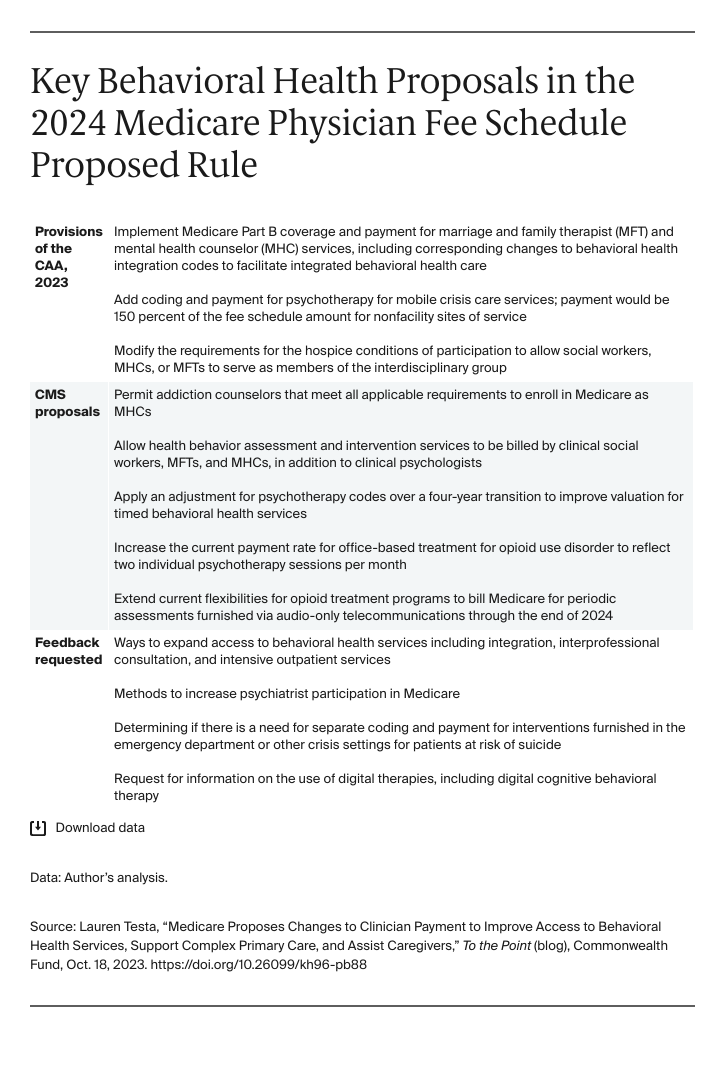
The Centers for Medicare and Medicaid Services (CMS) recognizes the need for a continuum of behavioral health providers to fully meet patient needs and has proposed an array of policies to expand the types of providers eligible to bill for behavioral health services within Medicare. Proposals also call for increases in payments for crisis care, substance use disorder treatment, and psychotherapy. The proposed rule implements several provisions of the Consolidated Appropriations Act, 2023 (CAA, 2023). The agency also seeks feedback on other actions it can take to improve beneficiaries’ access to behavioral health care.
Health-Related Social Needs
CMS proposes to establish new billing codes and payment for the administration of social determinants of health (SDOH) risk assessments, as well as community health integration (CHI) and principal illness navigation (PIN) services, provided by certified and trained community health workers, care navigators, peer support specialists, and other personnel. The proposed codes are the first specifically designed to account for the resources required when clinicians involve auxiliary personnel in furnishing these services. The change further legitimizes and encourages the inclusion of auxiliary personnel on the care team, helping to reduce the burden on clinicians and expand access to needed services.
Social Determinants of Health Risk Assessments
CMS proposes to add coding and payment for SDOH risk assessments to recognize the time and resources providers spend assessing social factors that may impact patient care. The risk assessment is a standard evidence-based tool that is tailored for a patient’s health literacy level, as well as educational, developmental, and cultural and linguistical background. If finalized as proposed, CMS would separately pay for an SDOH risk assessment provided on the same day as an in-person or telehealth evaluation and management visit, or through a supplementary payment when provided during a Medicare annual wellness visit.
Community Health Navigation and Principal Illness Navigation Services
Community health integration services address unmet SDOH needs that affect the diagnosis and treatment of a patient’s medical problems, while principal illness navigation services help people who are diagnosed with high-risk conditions (e.g., mental health conditions, substance use disorder, cancer) identify and connect with appropriate clinical and support resources. These services are especially beneficial for patients with socioeconomic disadvantages or barriers to care. CMS proposes to add coding and payment for both CHI and PIN services to reimburse auxiliary personnel for the time and resources required to connect beneficiaries with the additional support they need to produce positive health outcomes. If finalized as proposed, these services could be furnished monthly following an initiating evaluation and management visit.
Complex Primary Care
In the 2021 PFS final rule, CMS implemented a new add-on code to recognize the increased time and resources involved in providing primary care services to complex patients. Because of the need for budget neutrality, an increase in payment for some providers comes at the expense of others. Congress delayed implementing this change until now to address concerns about the potential reduction in payments for physicians who do not typically provide these services. In 2024, CMS proposes to implement the add-on code for complexity as anticipated, but refines the policy and substantially revises utilization estimates. Primary care providers (those practicing internal, general, geriatric, family, or pediatric medicine) are estimated to see annual PFS payments increase between 1 percent and 3 percent in 2024, with the add-on code driving most of this change. CMS hopes that by reimbursing practitioners for delivering complex primary care services, patients’ access to continuous, comprehensive care will increase, improving outcomes and better aligning payment with value.
Caregiving
CMS proposes to pay physicians and nonphysician practitioners or therapists when they train and involve caregivers — broadly defined as a family member, friend, neighbor, or guardian who provides unpaid assistance to a person with a chronic illness or disabling condition — in carrying out a treatment or therapy plan of care for Medicare patients with certain diseases or illnesses (e.g., stroke, dementia). Under the proposal, providers would receive payment for delivering caregiver training services, in tandem with diagnostic and treatment services furnished directly to the patient. The training services would include strategies and specific activities to assist the patient in carrying out the treatment plan. These may include ways to structure the patient’s environment to support and reinforce desired behaviors, techniques to reduce the negative impacts of the patient’s diagnosis on daily life, and skills to help manage the patient’s challenging behavior. Research suggests that involving caregivers in the care plan and providing training can improve health outcomes and alleviate the stress caregivers feel about fulfilling loved ones’ needs. This support is even more important for beneficiaries of color, who are more likely to rely on unpaid informal caregiving.
Conclusion
The 2024 PFS proposed rule marks the first time CMS has proposed a coordinated set of coding and payment changes to advance health equity goals within the fee schedule. These proposals can help increase access to behavioral health services, incentivize whole-person care and training for caregivers, and improve payment for traditionally undervalued services. Public comments were due September 11, 2023; a final rule is expected in November. If finalized, policies will take effect on January 1, 2024.



