A recent report from the Centers for Medicare and Medicaid Services (CMS) shows that national health spending grew at a historically low rate of 3.9 percent in 2010, almost paralleling the 3.8 percent increase in our gross domestic product (GDP) last year. This is somewhat reassuring news for the millions of American families and businesses who have struggled with the explosive growth in health insurance premiums and out-of-pocket costs over the past decade. It’s also good news for the federal government as the slowdown indicates that the cost of health reform has been overestimated.
There are several likely explanations for the relatively modest growth in health spending. First, as federal officials have noted, continuing declines in employment and private health insurance coverage have contributed to fewer people receiving both essential and nonessential treatment. The number of people covered by private insurance declined by 5 million in the last two years, and the number of uninsured reached a record-high 50.7 million in 2009. Without coverage, fewer people have received needed preventive and acute care. And people have increasingly gone without prescriptions, tests, and elective procedures.
Some of the slowdown in 2009 and 2010 may be related to the uncertainty surrounding the enactment and implementation of the Affordable Care Act. During earlier reform efforts, including President Clinton’s proposed health reform and President Carter’s proposed hospital cost containment legislation, health care cost growth abated as cautious hospital and other health care leaders held back on hiring decisions until the implications of proposed changes were clearer. In 2009 the health care industry—including hospitals and pharmaceutical companies—also pledged to achieve voluntary savings.
Health spending trends may also reflect almost a decade of voluntary efforts to improve patient safety and quality, and eliminate waste—cutting costs while improving health outcomes. The Institute for Healthcare Improvement has completed several successful campaigns to improve patient safety and continues to support widespread initiatives that encourage efficiency. The Commonwealth Fund’s own Commission on a High Performance Health System has been publicizing approaches to reduce hospital readmissions, implement medical homes, and improve the quality of nursing home care. Some hospitals are now using “Lean” techniques used by other industries to improve care and cut out waste. The American Recovery and Reinvestment Act included significant funding for physicians and hospitals to adopt health information technology, which should improve efficiency. 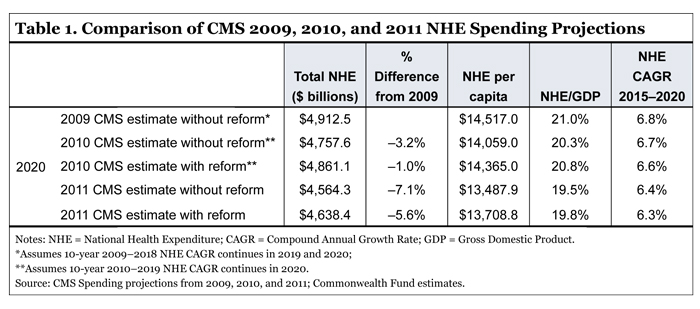
Whatever the reason, one significant implication of the new figures is that the original federal budget costs of the health reform law were overestimated. As Table 1 illustrates, in 2009, as health reform was being debated, total national health expenditures were projected to reach $4.9 trillion in 2020. This baseline was used by federal scorekeepers evaluating the law and estimating the cost of providing coverage for the uninsured and premium subsidies for working families. Today’s figures show that expenditures are now projected to reach $4.6 trillion in 2020, 5.6 percent below original estimates.
By using the higher 2009 health system spending baseline, analysts assumed that providing coverage for the uninsured and premium subsidies would be more expensive for the federal government than now appears to be the case. The offsetting revenue estimates, by contrast, are less sensitive to the slowdown in health expenditures—legislative provisions such as taxes on wealthy individuals, lower Medicare Advantage payments, and productivity adjustments for hospitals can still be expected to produce significant federal budget savings. If scorekeepers were to redo original estimates based on these new projections, the deficit reduction generated by health reform would be greater.
More broadly, any reduction in health spending growth is reason for cautious optimism as premium growth moderates and the public cost of providing affordable coverage to all is reduced. Indeed, the slowdown in health care costs in the last two years has already saved the nation substantially more in national health expenditures ($274 billion less by 2020 than originally estimated) than CMS estimated health reform will have increased expenditures in 2020 ($74 billion).
The slowdown also benefits employers, households, and state governments. In 2009 CMS estimated that total health expenditures would consume 21 percent of the GDP in 2020. Now, with health reform, it estimates that health spending will be 19.8 percent of GDP. And instead of increasing at an annual rate of 6.8 percent between 2015 and 2020 as projected prior to reform, health spending with health reform is now projected to grow at 6.3 percent annually.
All of this is good news for federal policy officials as they grapple with the federal budget deficit. Health care costs are abating, and the revenues used to finance health reform are reducing the deficit while health reform budget expenditures have been overestimated. But it is not the time for complacency.
Despite the slowdown, U.S. health care spending per person is still more than twice that in other major industrialized countries, and costs are projected to rise though 2020. The retirement of “boomers” born after World War II will continue to cause health care expenditures and federal budget outlays to increase as a percentage of the economy. It is important to implement key cost-saving provisions of the Affordable Care Act, including value-based purchasing, shared-savings incentives for accountable care organizations, innovative payment pilots such as patient-centered medical homes, and creation of the Independent Payment Advisory Board.
Fundamental changes to the health care system are needed to alter the long-term outlook for health care cost growth and protect the country from future increases. Key provisions of the Affordable Care Act offer the potential to usher in a new era in health care with greater emphasis on cost control, efficiency, and avoidance of overutilization and waste. Fully implementing and building on important tools such as the Independent Payment Advisory Board and Center for Medicare and Medicaid Innovation can ensure we continue to do just that.



