Washington’s Selective Procurement Approach
When Washington first launched its public option program, the state accepted all five bidders to ensure public option plans were widely available. But participating carriers limited their geographic range to a few counties each and some hospitals refused to join their networks. (Washington caps how much public option plans can pay providers in the aggregate.) This left wide gaps in plan availability and led the state to require hospitals participating in other state programs to contract with at least one public option plan if public option plans were not available statewide by 2022.
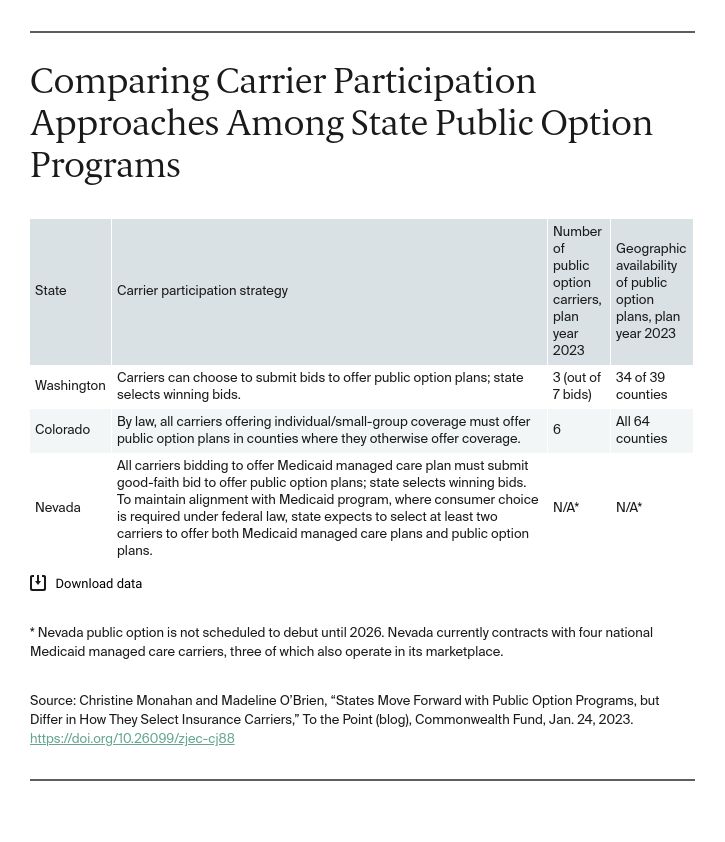
For the 2023 plan year, with this new requirement in effect, seven carriers submitted bids to offer public option plans. Most proposed to be in 10 or more counties. Ultimately, Washington contracted with three carriers offering plans in 34 of 39 counties, enabling access to 98 percent of current marketplace customers.
According to Washington Health Benefit Exchange Board meeting materials, Washington’s selective procurement of carriers was motivated by concerns that state residents face “choice overload” and that contracting with all bidders would risk further “crowding” the individual market “without affordability or market competition gains.” Washington chose carriers that offered the best combination of geographic coverage and lower premiums relative to the competition. Looking ahead, Washington plans to continue use selective contracting with carriers to further lower premiums and improve quality.
Colorado’s Mandatory Participation Approach
Colorado launched its “Colorado Option,” this winter. Insurance carriers are required to offer gold, silver, and bronze tier public option plans in all counties where they offer individual or small-employer plans. This requirement helped ensure that public option plans are available in all 64 Colorado counties. In the individual market, six carriers offered 36 public option plans, representing 11 percent of plans in the market overall. In the small-employer market, 11 carriers offered 48 public option plans — about 10 percent of all plans. Despite the influx of public option plans, the total number of plans is down in both markets compared to 2022, after two carriers facing financial struggles exited Colorado as part of wider rollbacks.
Colorado Option plans are required to meet certain premium rate reduction targets and health equity–focused network requirements. While not all plans are on target to meet the premium reductions for 2023, the state estimates that 87 percent of current individual market enrollees will be able to enroll in a plan reaching this target. Beginning in 2024, noncompliant plans will face a public hearing to determine whether one or more health care providers prevented them from complying by refusing to agree to lower reimbursement rates. If the state insurance commissioner finds this to be so, the commissioner can order the providers to join the Colorado Option plan network at state-set reimbursement rates.
Nevada’s Approach Is Still to Be Determined
Nevada is preparing to launch a public option program in 2026. Like Washington, Nevada will contract with private carriers to offer public option plans, but Nevada law also requires carriers bidding to offer Medicaid managed care plans to submit good faith bids to offer public option plans. Private carriers that do not offer Medicaid plans can choose to bid on the public option procurement. To make it easier for public option carriers to build networks, Nevada also will require providers to join a public option network if they participate in Medicaid or other state plans.
The state maintains discretion over how many carriers it will select. Because state law requires the state to maximize alignment between the new public option and Medicaid, and federal law requires state Medicaid managed care programs to offer beneficiaries plan choice, the state likely will contract with at least two carriers.
Nevada plans to solicit stakeholder input on procurement and contracting in the spring of 2023. Its procurement process is expected to begin in late 2024, in conjunction with its next Medicaid managed care procurement.
Looking Forward
Deciding how to involve private carriers in public option plan administration raises many issues that state-based marketplaces have been facing for years, including whether to require carriers to participate and engage in active purchasing or selective contracting. States that partner with private carriers to offer public options are likely to reach different answers based on their market conditions. As more states consider public option legislation, leaders can look to the differing experiences across early adopters to inform their decision-making.