Where else can beneficiaries get information about coverage options?
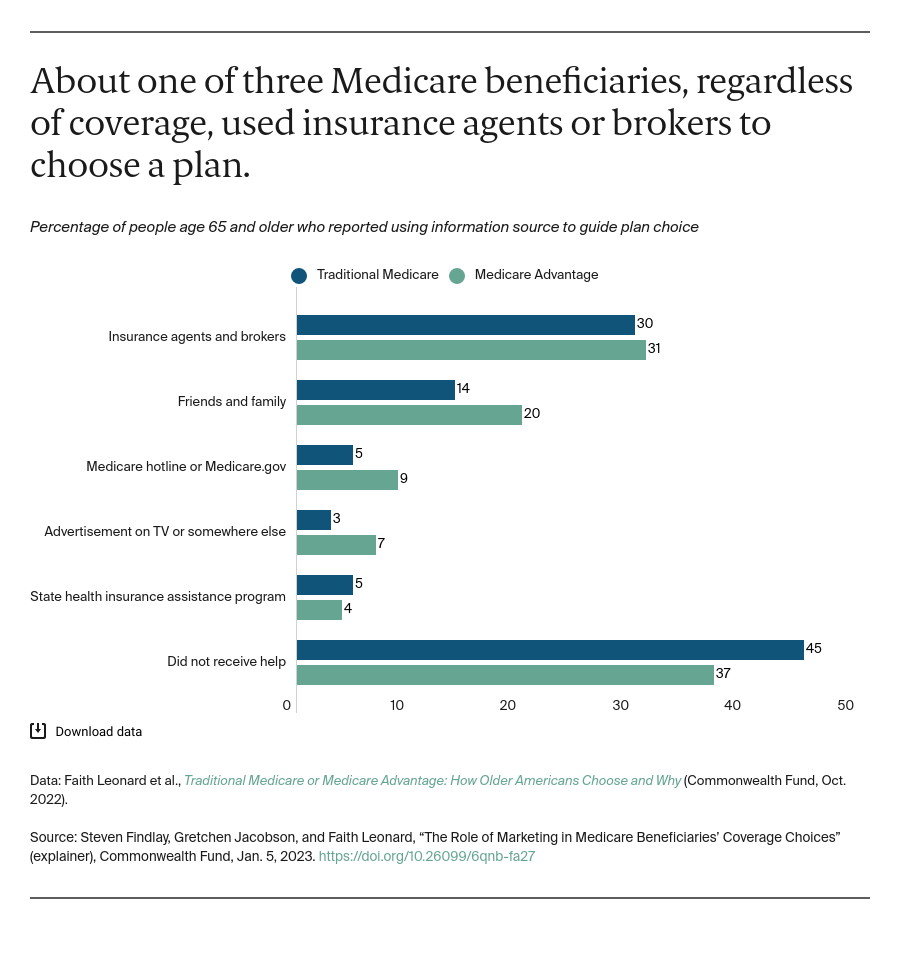
The Centers for Medicare and Medicaid Services (CMS), the federal agency that administers Medicare, provides detailed information on both traditional Medicare and Medicare Advantage plans in a 100-page booklet mailed annually to every beneficiary. The CMS-maintained website Medicare.gov provides information about coverage choices as well.
In addition, the federal government funds State Health Insurance Assistance Programs, or SHIPs, in each state to provide consumers with information, online and in person, about Medicare benefits and to offer personalized help with coverage options. The SHIPs received about $49 million in federal funding in 2021. Most SHIPs rely on volunteers, and many contract with local community-based partners to provide services.
Is plan marketing useful to beneficiaries in making coverage decisions?
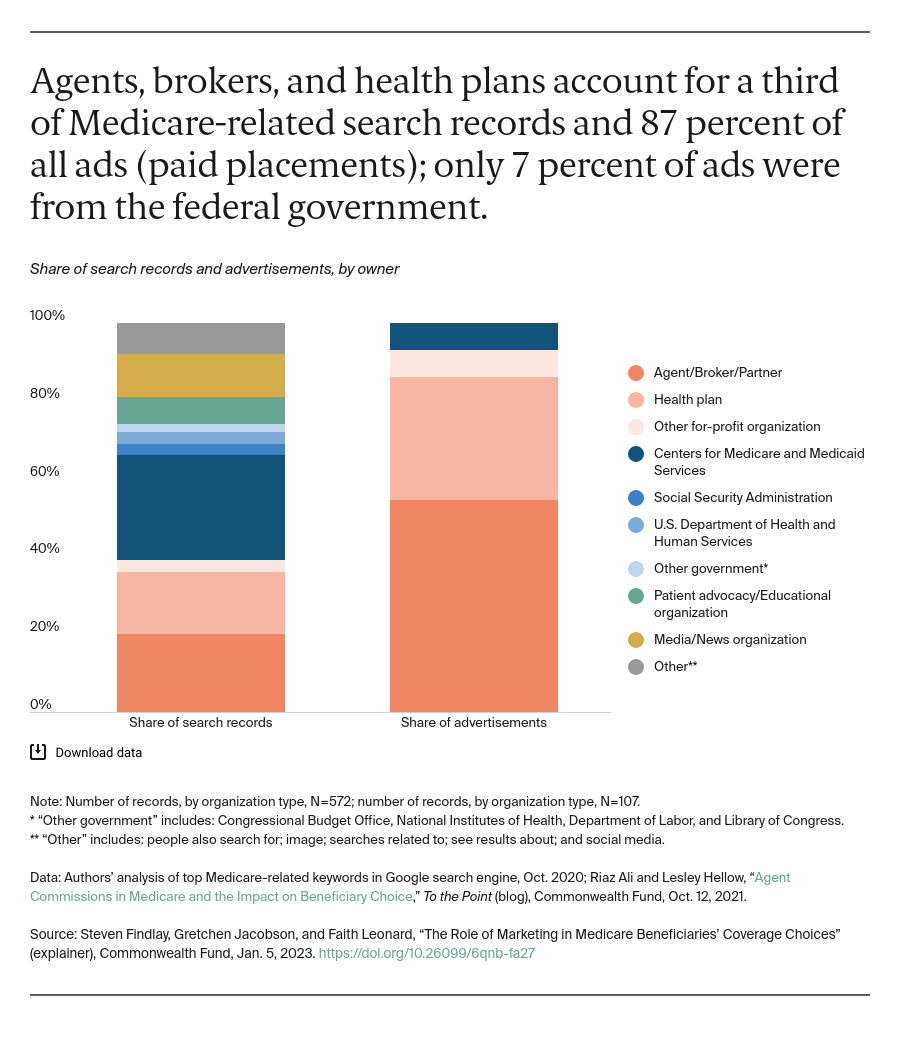
A relatively small proportion of beneficiaries use advertising to make their coverage decisions. Nonetheless, CMS reported more than 41,000 complaints in 2021 about Medicare private plan marketing, more than double the number in 2020 and up from about 6,000 in 2017. Complaints involved inaccurate or confusing information about reimbursements, benefits, premiums, and provider networks, as well as misleading print and TV ads. A recent report by the U.S. Senate Committee on Finance also identified examples of beneficiary complaints, including insurance agents soliciting enrollment at grocery stores; mailers from Medicare Advantage plans that looked like official business from the federal government; high-pressure solicitations, including robocalls multiple times a day; and agents suggesting in phone calls that they were speaking on behalf of Medicare and the government.
The rise in complaints could be the result of a number of factors. These include the surge in advertising by plans and by the agents, brokers, and other third-party marketing organizations, or TPMOs, with whom plans contract; the inability of plans to address beneficiaries’ complaints; or changes in how complaints are classified. Marketing violations, from spoofed robocalls to sham health plans, have been a recent problem in the commercial insurance market as well.
What has the federal government done to address the confusion and complaints?
Impelled by the rising number of complaints, CMS released new marketing rules that took effect in October 2022. The rules build on existing regulations that have evolved over years. CMS has proposed additional rules to further address complaints and beneficiary confusion including drawing greater distinction between education and marketing done by plans; restricting the use of the name “Medicare” in product labeling and marketing; restricting the use of superlatives like “best” or “most”; and prohibiting ads that don’t use a specific plan name.
Rules for insurers. The CMS rules are designed to prevent Medicare private plans from presenting misleading information about a plan’s costs or benefits. Only plans with the highest ratings (five stars) can be marketed all year. All other plans may contact beneficiaries about plan offerings only from October 1 through the end of Medicare’s open enrollment period on December 7, and during Medicare Advantage’s open enrollment period for current enrollees (January 1 to March 31).
CMS makes a distinction between communications and marketing materials. Marketing is considered information intended to influence beneficiaries’ decisions: details about benefits, premiums, and cost sharing; star ratings, rankings, and measurements; and how one plan compares to another. Communications materials do not provide this type of information. Plans are required to submit their marketing materials to CMS for review, though they are not required to do so for communications materials.
Insurers are not permitted to compare their plans with other plans by name or to suggest that Medicare prefers their plan. There are also restrictions on use of the term “free.”
In addition, educational activities must be separate from marketing activities, and insurers are responsible for TPMOs complying with CMS marketing rules. In this way, insurers are accountable for misleading marketing, even if an agent, broker, or online subcontractor was directly responsible.
Medicare Advantage and Part D plan sponsors must create inserts in their promotional materials written in each of the top 15 languages, aside from English, that are spoken in the U.S. Those materials must then reach people in geographic areas where the languages are spoken by 5 percent or more of the population. Additionally, plans must follow Section 508 of the Rehabilitation Act, which requires websites and other materials to be accessible for people with disabilities.
Rules for agents and brokers. The insurance agents and brokers that sell Medicare private plans are required to tell consumers when they do not sell all plans available in the area. At the same time, they are required to direct people to consult Medicare.gov or call 1-800-Medicare for information on all the options available in a given area. This message must be displayed in online, print, and TV ads, conveyed during phone conversations, and featured in digital “get-information here” tools that agencies and brokerage firms often use. TPMOs are also required to record all phone calls with beneficiaries.