Introduction
Since almost the inception of the Medicare program, beneficiaries have had the choice of receiving coverage through traditional Medicare or private insurance plans, known today as Medicare Advantage plans. Each year, during Medicare open enrollment, beneficiaries can reassess their coverage options to decide which coverage best meets their health needs and budget. Little research has been conducted to understand how and why beneficiaries make these choices.
Beneficiaries weigh several trade-offs.1 On the one hand, Medicare Advantage plans typically provide some coverage for benefits not included in traditional Medicare, such as eyeglasses. Plans also have a cap on out-of-pocket expenses for services covered by traditional Medicare, while traditional Medicare does not have a similar limit. On the other hand, traditional Medicare allows beneficiaries to go to any doctor, hospital, or other health care provider that accepts Medicare, without the need for prior approval; Medicare Advantage enrollees typically need a referral from their primary care physician as well as plan approval if they want services from specialists, such as oncologists, covered by the plan.
Historically, most Medicare beneficiaries have chosen to receive their benefits through traditional Medicare,2 but enrollment in Medicare Advantage plans has grown rapidly over the past decade. Forty-five percent of Medicare beneficiaries are enrolled in Medicare Advantage plans in 2022, a share that is projected to rise to more than 50 percent by 2025.3
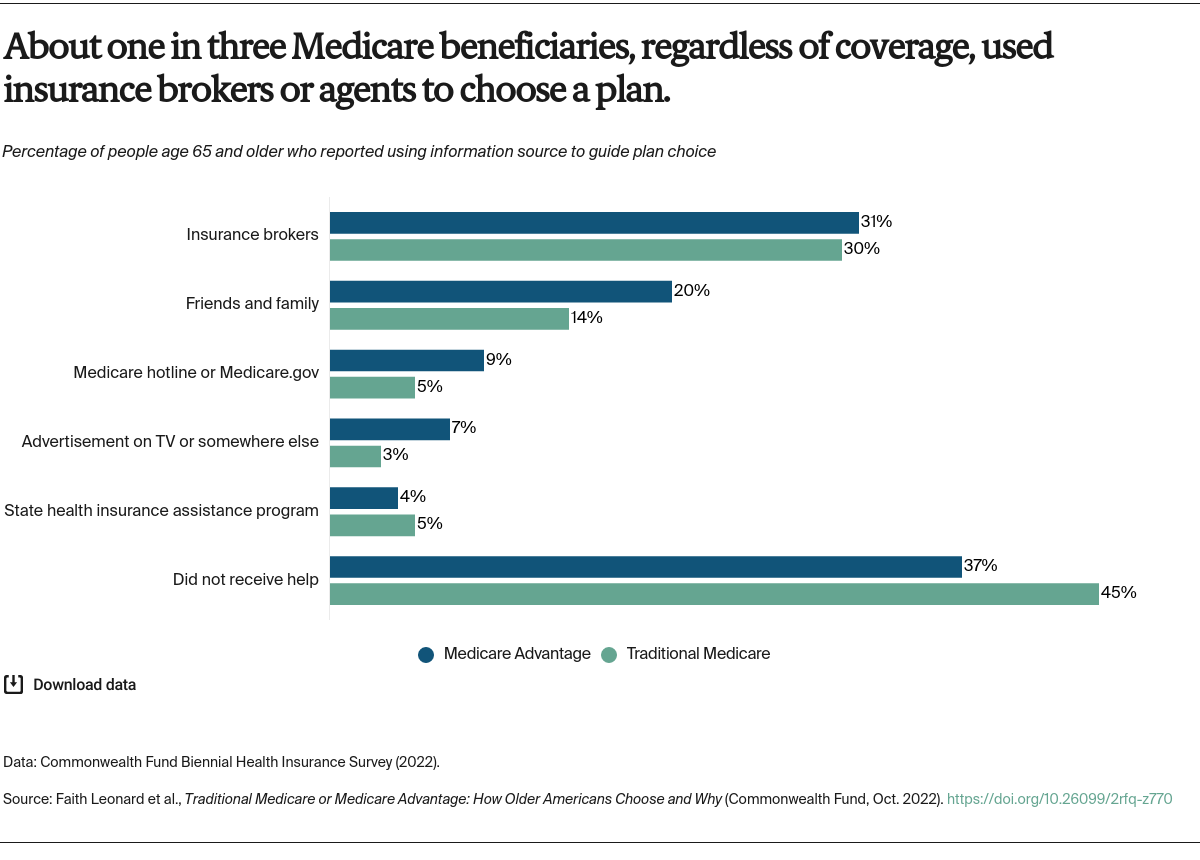
In the Commonwealth Fund’s 2022 Biennial Health Insurance Survey, we asked people age 65 and older who were enrolled in Medicare as their primary source of coverage why they chose Medicare Advantage or traditional Medicare, and what resources they used to choose their coverage. The survey firm SSRS interviewed a nationally representative sample of 8,022 adults age 19 and older between March 28 and July 4, 2022. This analysis focuses on 1,605 respondents age 65 and older who were enrolled in Medicare. To learn more about our survey, including the revised sampling method, see “How We Conducted This Survey.”