Abstract
- Issue: Disruptions in health coverage may delay care for beneficiaries and create higher administrative costs. To address these disruptions, Congress recently mandated 12-month continuous eligibility for children with Medicaid coverage starting in 2024. One state currently has continuous eligibility for adults, and two more will by 2024.
- Goal: To estimate the impact of extending universal 12-month and 24-month continuous eligibility to all adult Medicaid enrollees on health care coverage and costs.
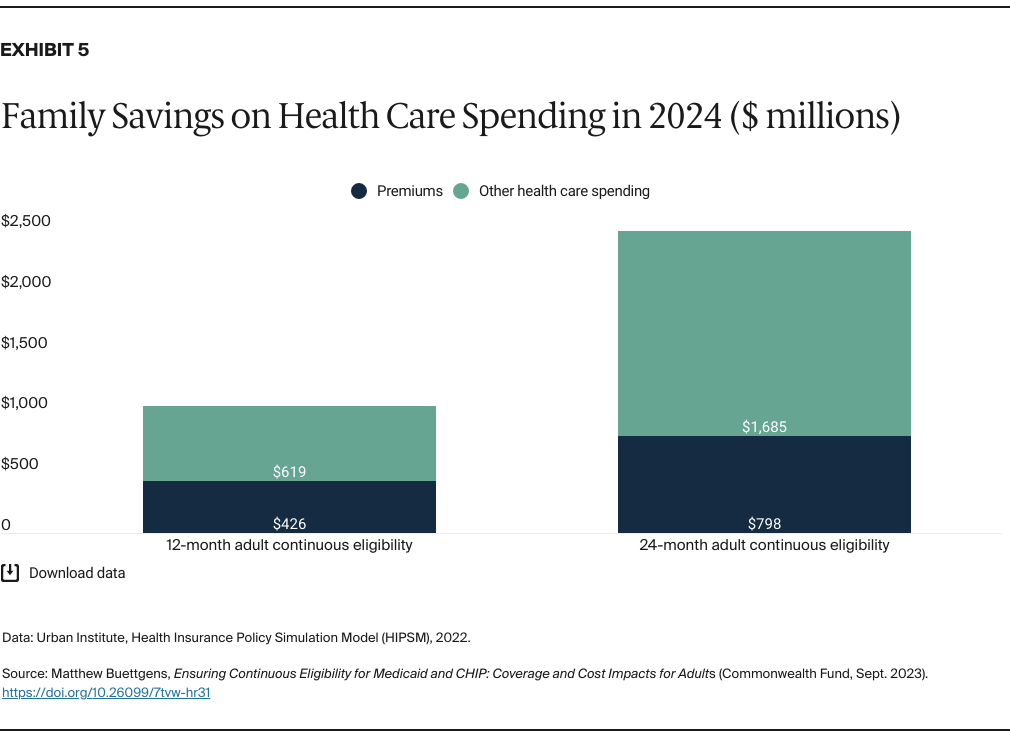
- Methods: Simulation of changes in health coverage and government spending impact, using the Urban Institute’s Health Insurance Policy Simulation Model.
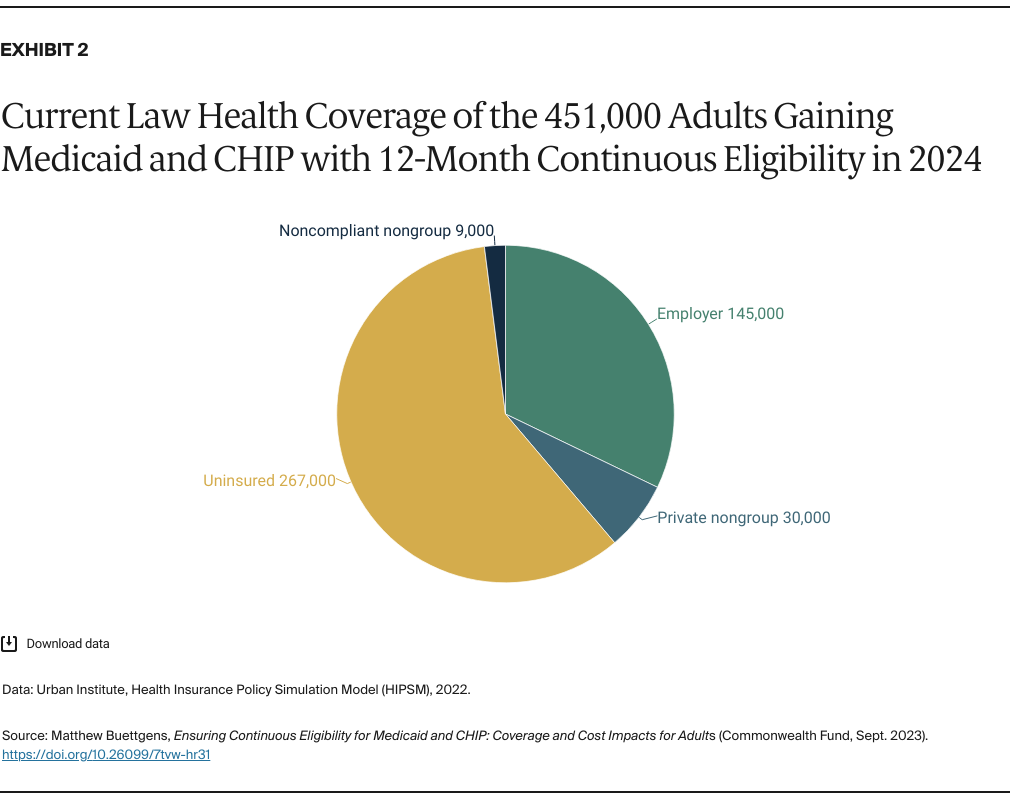
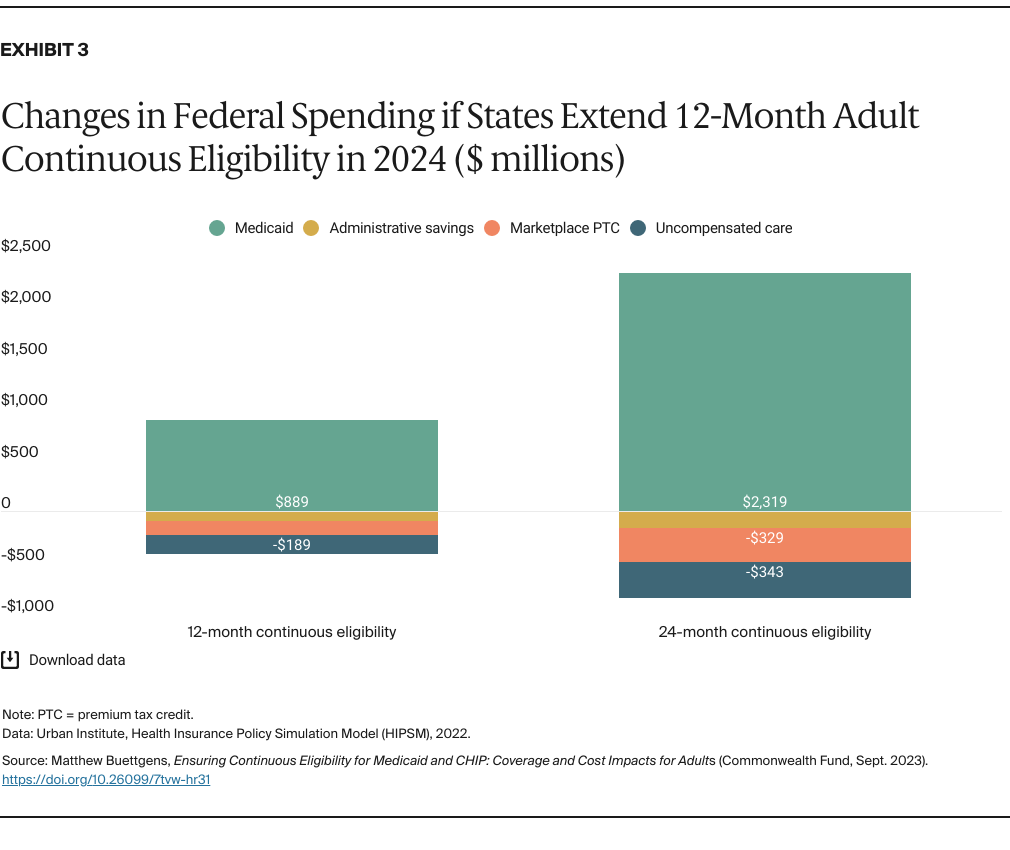
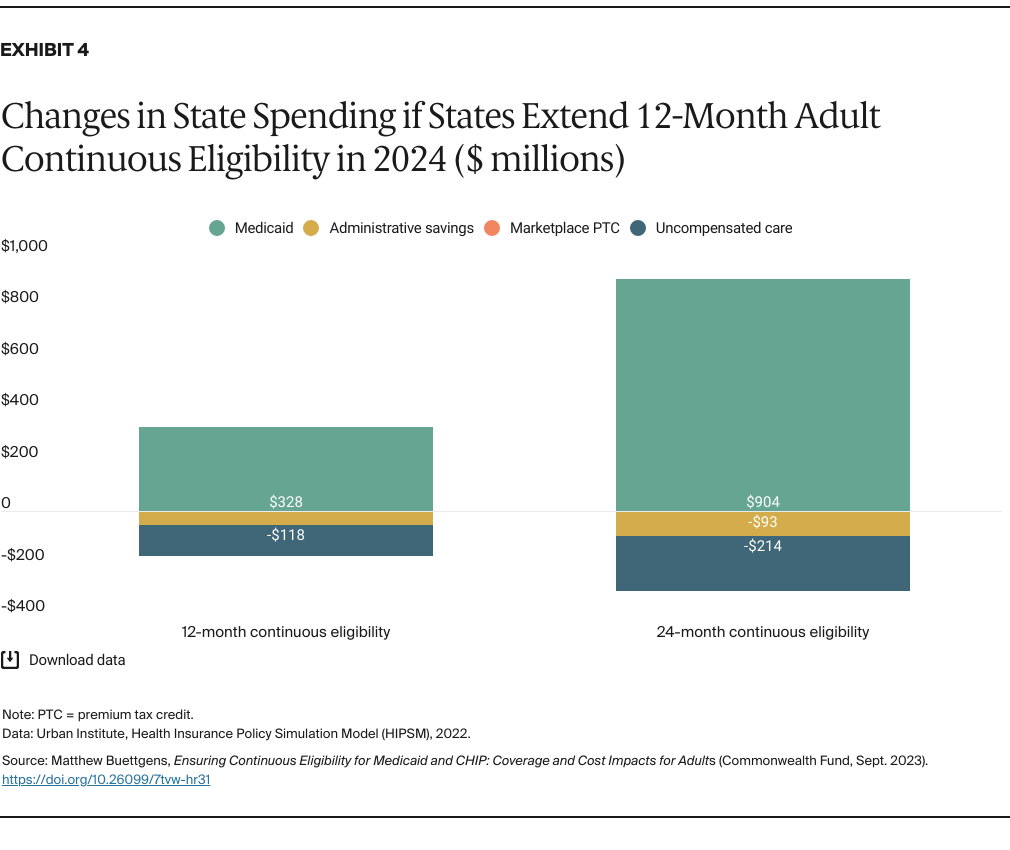
- Key Findings and Conclusions: If all states adopted 12-month continuous eligibility for adults, 451,000 more adults would be enrolled in Medicaid in an average month in 2024, a 1.3 percent increase. There would be 267,000 fewer uninsured people in an average month, and the reduction in the number of people uninsured at any time would be greater. Federal and state spending in 2024 would increase by $479 million and $158 million, respectively. Both are increases of only 0.1 percent in spending on acute care for the nonelderly. Households and employers would each save about $1 billion a year in health care spending, and total health care spending would decline by $1.8 billion in 2024. Continuous eligibility for 24 months would further expand coverage and reduce costs.
Introduction
Every year, millions of adults are enrolled in Medicaid for less than 12 months, and many reenroll within a year.1 Although some who leave the program after less than a year do so because they have obtained other health insurance (such as coverage through a new employer), others simply become uninsured. Disruptions in health coverage can lead to people delaying needed care and to higher costs for Medicaid.2
To improve continuity of coverage, many policymakers have proposed giving Medicaid enrollees a fixed term of continuous eligibility. Under the Affordable Care Act (ACA), states cannot make most Medicaid enrollees go through the renewal process more than once every 12 months.3 However, beneficiaries are required to report changes in circumstances that could affect eligibility, and states can require individuals to provide income verification in as little as 10 days or face disenrollment. But under a policy that guaranteed a fixed term of continuous eligibility (12 months in most proposals), coverage would remain. Yet some beneficiaries could still lose coverage during the year if they move out of state, age out of a program for children, or fail to pay premiums.
States have long had the option of extending 12-month continuous eligibility to children through Medicaid or the Children’s Health Insurance Program (CHIP). Congress made this mandatory in the Consolidated Appropriations Act of 2022. However, states need to apply for a Section 1115 waiver to extend continuous eligibility to adults. New York is the only state that currently has 12-month continuous Medicaid eligibility for adults. The Centers for Medicare and Medicaid Services (CMS) recently approved continuous eligibility waivers that will cover adults in Oregon and Illinois, and other states are seeking similar waivers.
In this brief, we use the Urban Institute’s Health Insurance Policy Simulation Model to estimate the impact of all states adopting 12-month and 24-month continuous eligibility for adults in Medicaid in 2024. By this time, all states will have implemented 12-month continuous eligibility for children. We consider the impact of similar policies on children in a companion issue brief.4
Our estimates do not include the temporary impact of the unwinding of the COVID-19 public health emergency (PHE), which will affect health coverage for the first half of 2024.5
Key Findings
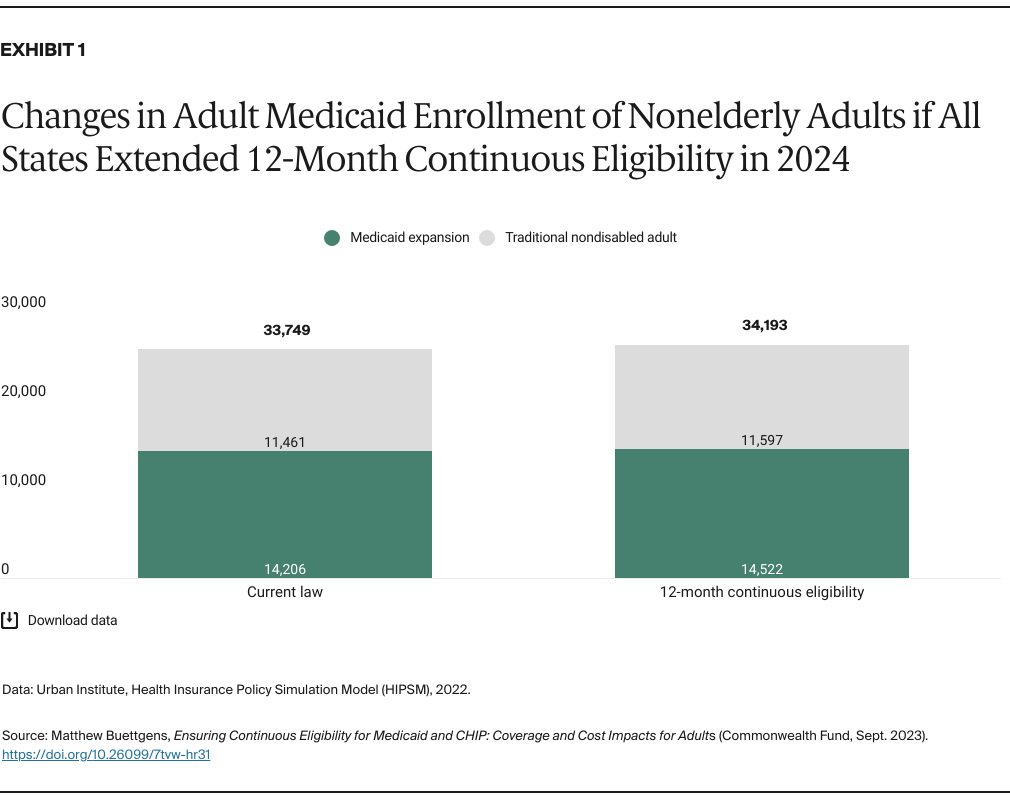
Impact on coverage with 12-month continuous eligibility. If all states adopted 12-month continuous Medicaid eligibility for adults, we estimate that 451,000 more adults would be enrolled in an average month of 2024, an increase of 1.3 percent (Exhibit 1 and Appendix 1). There would be 315,000 more Medicaid expansion beneficiaries (a 2.2% increase) and 136,000 more nondisabled adults enrolled (a 1.2% increase).