Abstract
- Issue: Disruptions in health coverage may delay care for children and create higher administrative costs. To address these disruptions, the Consolidated Appropriations Act of 2022 requires states to give children 12 months of continuous eligibility for Medicaid and the Children’s Health Insurance Program (CHIP) by 2024. Currently, 33 states offer continuous eligibility to at least some children.
- Goal: To estimate how ensuring 12-month and 24-month continuous eligibility for all children in Medicaid and CHIP would affect health care coverage and costs.
- Methods: Simulation of changes in health coverage and government spending impact, using the Urban Institute’s Health Insurance Policy Simulation Model.
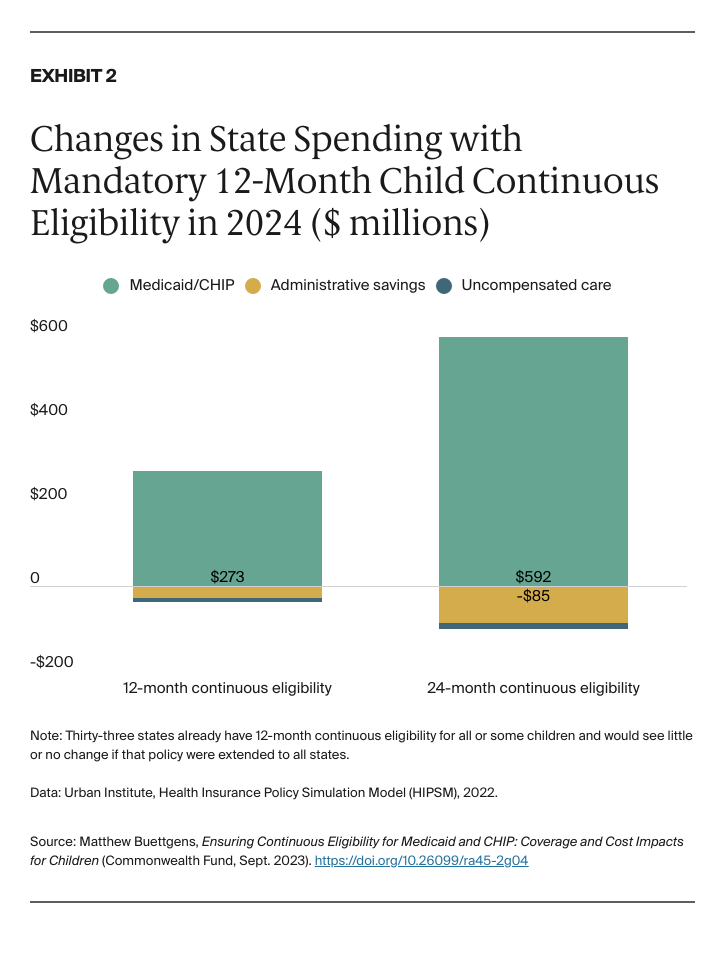
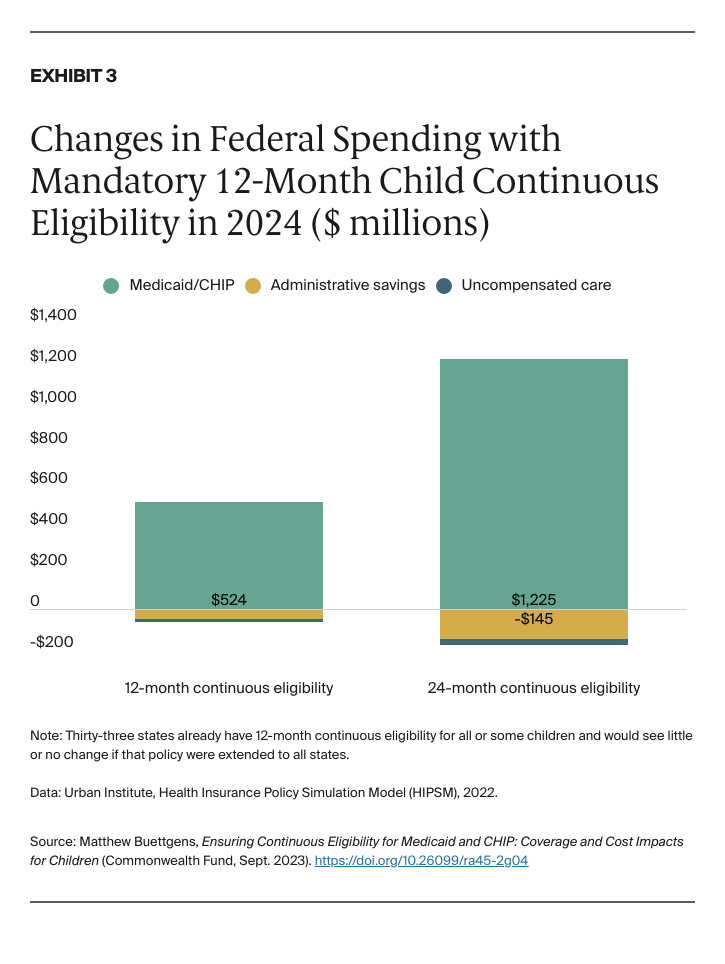
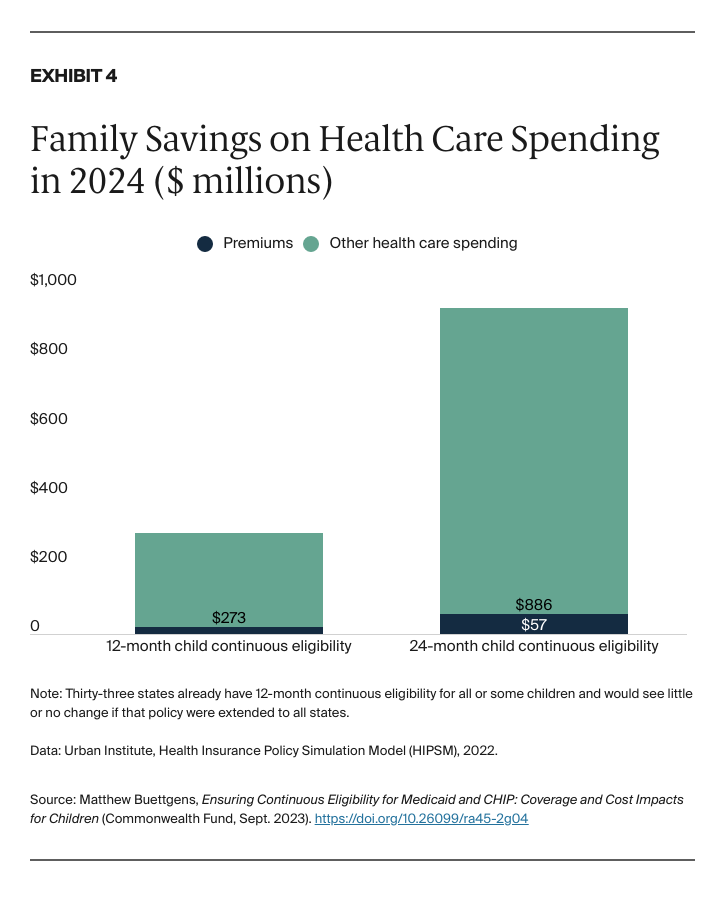
- Key Findings and Conclusions: When all states adopt 12-month continuous eligibility in 2024, Medicaid and CHIP enrollment in states that do not already have it will increase by 239,000 children in an average month, an increase of 0.6 percent. Families will spend an estimated $292 million less on health care, an average of $1,222 less per year for each child newly enrolled in Medicaid and CHIP. Federal spending will increase by $458 million annually, and state spending will increase by $238 million annually, both only 0.1 percent increases in government spending on acute care for the nonelderly. Adopting continuous eligibility for 24 months would further expand child health coverage and reduce costs for families.
Introduction
Starting in 2024, the Consolidated Appropriations Act of 2022 requires states to provide children up to age 18 with 12 months of continuous eligibility for Medicaid and Children’s Health Insurance Program (CHIP) coverage. Continuity of coverage is particularly important for children enrolled in Medicaid and CHIP who benefit from regular well-child visits. Disruptions in health coverage may lead to delayed care and higher costs for Medicaid and CHIP.1
States already had the option of extending 12-month continuous eligibility to children through Medicaid or CHIP, but not all states adopted it. At the time of writing, 24 states had 12-month continuous eligibility for all children’s coverage, and nine more had 12-month continuous eligibility for some children’s coverage, often for CHIP but not Medicaid.2 Some states are interested in extending continuous eligibility even further, for 24 months. In 2022, the Centers for Medicare and Medicaid Services approved a waiver in Oregon that would give children continuous eligibility up to age 6 and 24-month continuous eligibility for older children.
In this brief, we use the Urban Institute’s Health Insurance Policy Simulation Model to estimate the impact of all states adopting 12-month and 24-month continuous eligibility for Medicaid and CHIP for children. (For more detail, see “How We Conducted This Study.”) We consider the impact of similar policies for adults in a companion issue brief.3
Our estimates do not include the temporary impact of the unwinding of the federal COVID-19 public health emergency, which will affect health coverage for the first half of 2024.4
Key Findings
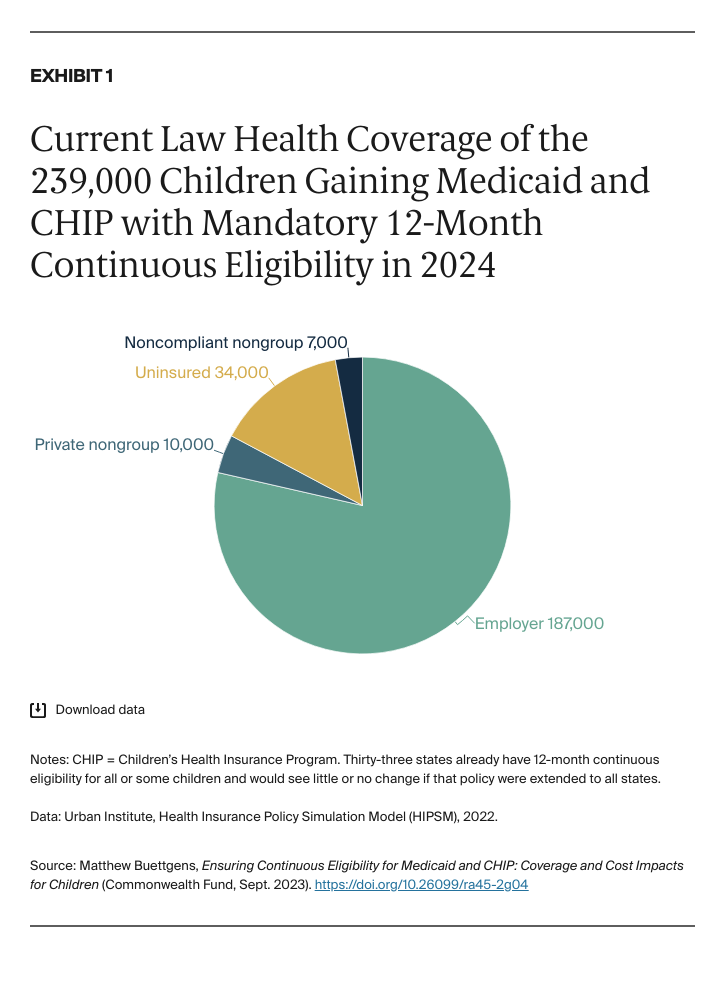
Impact on coverage with 12-month continuous eligibility for children. When the remaining states adopt 12-month continuous eligibility for children with Medicaid and CHIP, we estimate that 239,000 more children will be enrolled in an average month of 2024, an increase of 0.6 percent (Appendix 1). This expansion in coverage occurs in states that have not already adopted continuous eligibility or which do not offer it to all children. We estimate that Medicaid and CHIP will cover about 47 percent of children in 2024.
With this increase in coverage, 34,000 fewer children will be uninsured in an average month, a decrease of 1.3 percent (Exhibit 1 and Appendix 1).