Born as an afterthought to Medicare five decades ago, Medicaid has evolved from an adjunct to state welfare programs to the nation’s largest health insurer. The occasion of Medicaid’s 50th birthday is a fitting time to consider that evolution, not to reminisce, but to help chart the path forward. Medicaid is a complex program with a complex history, and understanding its role in the U.S. health system is essential to ensuring that it is performing at optimal levels for its beneficiaries, as well as for states, taxpayers, and the myriad health care providers, health plans, and others touched by the program. In a four-part series supported by The Commonwealth Fund, Cindy Mann and Deborah Bachrach of Manatt Health Solutions examine Medicaid’s evolution and consider its role in the new coverage paradigm established by the Affordable Care Act (ACA).
On January 1, 2014, a new health care coverage paradigm took hold in the nation. A transformed Medicaid program became, along with the insurance marketplaces and the Children’s Health Insurance Program, one of three programs offering a continuum of subsidized coverage for people who lack affordable insurance through the workplace.
The Affordable Care Act (ACA) solidified Medicaid’s health insurance credentials, moving it farther along a path it had been traveling for three decades—from its origins in the welfare system to the nation’s largest health insurer. And yet, efforts to bring Medicaid back to its welfare roots continues to haunt the program—as evidenced by recent proposals by some states to impose work requirements and eligibility time limits and to resist expanding eligibility to cover so-called “able-bodied” adults. Medicaid is a complex program that has looked different at different times in its history; appreciation of its role today has implications for Medicaid and the entire health care system.
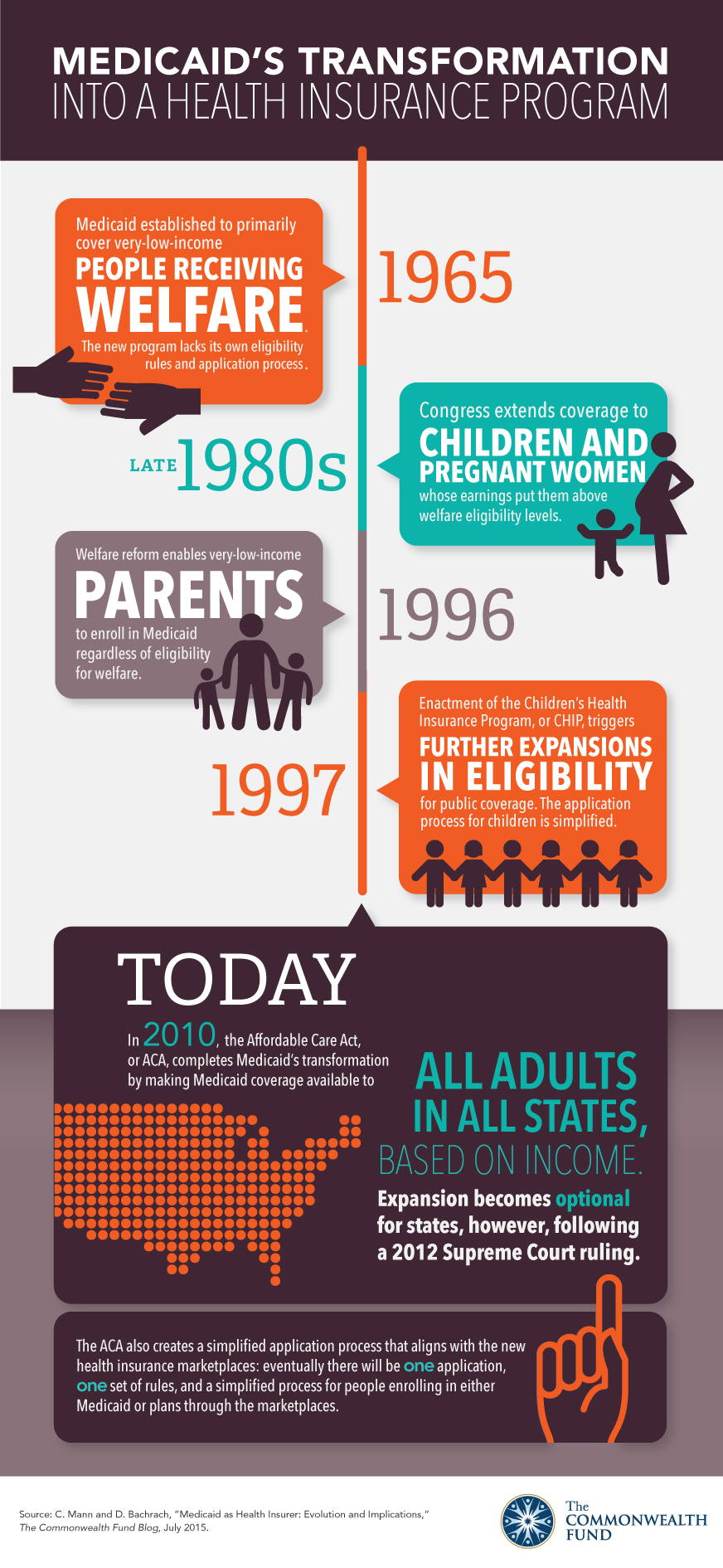
Medicaid started out in 1965 primarily covering people receiving welfare. It didn’t have its own eligibility rules or application process. If you qualified for cash assistance, you received a Medicaid card. Its reach was limited; the nation’s welfare system—and therefore Medicaid—confined its support to the so-called deserving poor: children and their parents and the elderly, blind, and disabled. And, in keeping with operative welfare principles and budget considerations, enrollment was not encouraged. Most low-income families remained uninsured.
In the late 1980s, concerns about infant mortality and children’s health prompted Congress to extend Medicaid coverage to children and pregnant women whose earnings put them above welfare eligibility levels. This striking expansion of coverage reflected an equally striking though less noted break in the relationship between Medicaid and welfare. Medicaid had begun its steady march to becoming a health insurance program for low-income individuals.
The year 1996 was the year of welfare reform. The Aid to Families with Dependent Children program was replaced by the Temporary Assistance for Needy Families block grant to states, with the goal of reducing reliance on welfare by ending the entitlement to cash aid and imposing work requirements and time limits. But health coverage was seen as different—something that ought to be available to people even if they were no longer (or never were) cash assistance recipients. And so, the same law that revamped welfare further severed the ties between it and Medicaid by ensuring that very-low-income parents could enroll in Medicaid regardless of their eligibility for cash assistance.
The enactment of the Children’s Health Insurance Program, or CHIP, in 1997 prompted the next round of changes. CHIP triggered further expansions in eligibility for children in Medicaid and CHIP, and brought about a wholesale overhaul of the way children enrolled in coverage. The Medicaid application process for children was simplified: families didn’t have to come into the welfare office to apply, asset tests were dropped, and unnecessary verification burdens were lifted. The explicit goal of promoting coverage was a marked departure from the objectives that had characterized the administration of welfare, and, derivatively, Medicaid. These efforts have had a lasting impact for kids and provided a blueprint for the ACA. Driven largely by public program coverage, uninsured rates for children dropped from a high of 15 percent in 1994 to 7 percent in 2013.
The ACA completed Medicaid’s evolution from an adjunct to welfare programs to an insurance program for low-income Americans, at least on paper. It eliminated the carryover from welfare of covering only certain groups of low-income adults. For the first time, Medicaid coverage was to be available to all adults in all states based on their income, whether or not they had children. Expansion, however, became optional after the 2012 Supreme Court ruling and 20 states have yet to expand the program.
But perhaps just as significant, the ACA established new Medicaid eligibility rules and processes aligned not with welfare but with the marketplace. It called for one application, one set of eligibility rules, and one simplified process for enrolling in the appropriate health coverage program. Though these changes are not yet fully mature, one year after implementation, the national uninsured rate has dropped to a record low, with rates falling most sharply in states taking up the Medicaid expansion.
So far, 30 states and D.C. have chosen to expand Medicaid eligibility. A handful of these states have done so by adopting alternative expansion policies requiring federal waivers. Some of the states now considering expansion and some that have already expanded are proposing welfare-style work or eligibility time limits.
Medicaid’s transformation is an important lens through which to consider current as well as the next generation of policies. For example, will the state expansion proposals requiring work or time limits strengthen Medicaid’s ability to function as a cost-effective, high-quality insurer aligned with other parts of the health care system, or do they harken back to a different era and a different program? Important work remains to be done to track these and other policies, and a clear-eyed vision of Medicaid’s role is essential to accomplish the work ahead.