As part of its COVID-19 response, Congress established the $175 billion Provider Relief Fund (PRF) under the CARES Act to compensate for lost revenues providers have experienced as visits have dropped and to help providers respond to the pandemic — for instance, for purchasing personal protective equipment. The law set these two broad uses, leaving it to the U.S. Department of Health and Human Services (HHS) to determine how to distribute funds among providers.
Since April, HHS has allocated funding to different groups of providers in waves and over time and has reclassified payments into two types of distributions. These include general distribution (providers receive at least 2% of annual patient revenue), and targeted distribution (certain providers receive additional payments — for example, payments to hospitals in “hot spots” and to safety-net hospitals). On October 1, HHS announced a new Phase III of the general distribution, indicating that payments will take account of providers’ revenue losses and expenses attributable to COVID-19 and the PRF payments they have received to date. However, HHS did not provide the payment methodology.
To date, community-based providers (i.e., noninstitutional providers, such as behavioral health clinics and pediatricians) that serve Medicaid and uninsured patients have been disadvantaged by this distribution model in three ways:
- they are disadvantaged by the rules for calculating general distribution payments
- with the exception of rural health centers, they have been left out of the targeted distributions
- the PRF is administratively complex and challenging for tightly staffed, small practices to navigate.
Without more support, these providers are at risk of closing, which will lead to ongoing challenges in health care access in the very communities most impacted by COVID-19.
General Distribution Methodology to Date Disadvantages Medicaid Providers
The basic premise of the general distribution is that all providers will receive at least 2 percent of net patient revenue. Under the new Phase III distribution, some providers (though it is unclear exactly which ones) will receive additional payments.
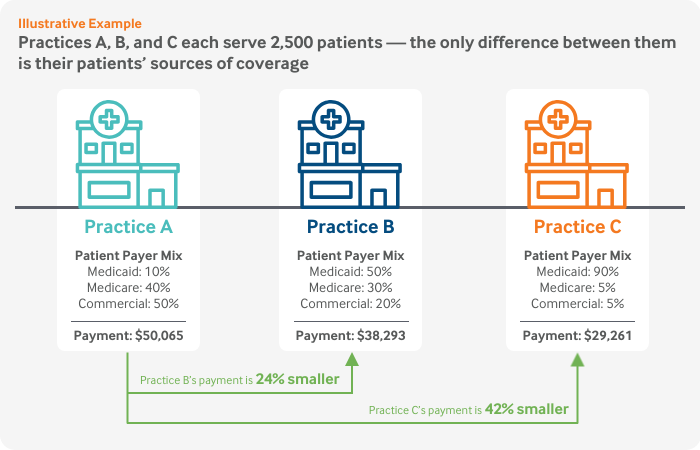
Basing payments on patient revenue means the highest per-patient payments go to providers with a large proportion of privately insured patients and the lowest go to providers with a high percentage of Medicaid patients. In other words, the least-well-resourced providers with the lowest patient revenue and thinnest margins receive the smallest general distribution payments.
This figure illustrates how the methodology plays out for three hypothetical practices that are identical in every way, except for their patients’ sources of coverage.
Through the recently announced $20 billion Phase III general distribution, HHS will make additional payments to Medicare, Medicaid, Children’s Health Insurance Program, dental, assisted living facility, and behavioral health providers based on revenue losses and expenses attributable to COVID-19. Some providers will receive an additional payment above 2 percent of net patient revenue, but the exact payment methodology was not announced. We do not yet know whether HHS will apply targeting principles to ensure the new distribution will prioritize community-based Medicaid providers or if it will perpetuate an approach that disadvantages providers with the thinnest margins.
Medicaid Community-Based Providers Are Left Out of Targeted Distributions
The general distribution’s shortcomings are exacerbated by the fact that Medicaid community-based providers have not received additional targeted relief. When announcing a distribution for safety-net hospitals, HHS acknowledged that “targeting funds to Medicaid and safety-net providers is essential because they operate on thin margins and may be struggling during this crisis” and that “it’s also important because the populations they serve, low-income and minority Americans, have suffered disproportionately from COVID-19.” Medicaid community-based providers, however, have yet to receive targeted support.
PRF is Administratively Complex and Difficult to Navigate
Since April, HHS has issued dozens of announcements and guidance changes — including altered eligibility criteria — and established terms and conditions and application portals. While perhaps unavoidable given how quickly HHS needed to act, the volume and changing rules created a difficult system for even large, well-resourced provider systems to navigate. Medicaid community-based providers that wanted to access funds had to know which distributions they were eligible for, the rules governing the use of the funds, and how to apply even as the rules were changing. Some of these providers received minimal payments (as little as $1) from the first round of general distribution payments issued in mid-April1 and were locked out of applying to receive their full 2 percent of patient revenue payment until mid-August, when HHS updated certain eligibility criteria.
The Centers for Medicare and Medicaid Services and the Health Resources and Services Administration recognized these challenges after holding listening sessions with providers. In a July 28 call with state Medicaid leaders, agency staff stated that “some of the smaller organizations just really weren’t aware [that they were eligible] . . . providers just really weren’t sure how to proceed,” and providers were hesitant to apply without “the full picture . . . with meeting the terms and conditions with reporting, use of funds, etc.”
Moving Forward: How to Protect Access to Medicaid Community-Based Providers
In addition to increasing the PRF’s available funds, the following actions could help ensure that Medicaid community-based providers have the resources to stay open during the pandemic and beyond:
- design the Phase III general distribution methodology to prioritize add-on payments (i.e., payments in addition to the 2% of patient revenue) to providers that are experiencing the greatest financial hardship and have the smallest operating margins
- establish a targeted distribution for community-based providers with a high proportion of Medicaid patients based on metrics such as the number of patients a provider serves
- release meaningful provider-level PRF payment data to allow states and policymakers to assess where need is the greatest
- simplify future communications and application processes.
Medicaid providers serve 20 percent of the U.S. population, including four of every 10 children; Medicaid finances nearly half of all births. Medicaid community-based providers have been on the front lines providing treatment for people suffering from the opioid crisis and will be key to distributing a COVID-19 vaccine once it is available. Their patients are among the hardest hit by COVID-19. That harm will extend well beyond the pandemic if they are forced to close their doors.


