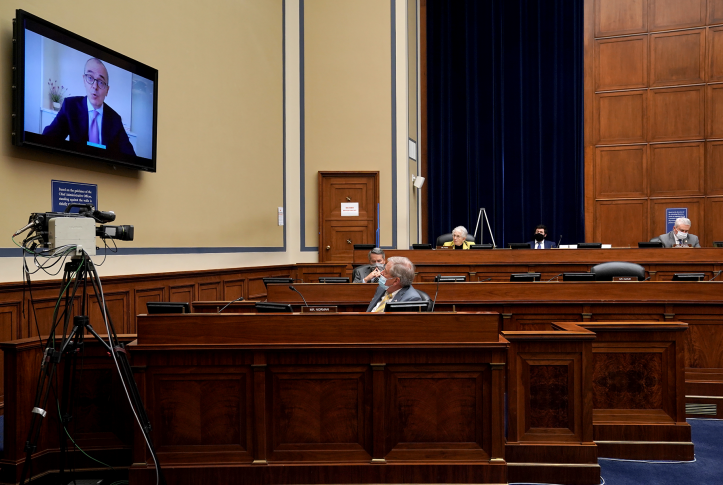
Yesterday, the House Oversight and Reform Committee announced a third hearing related to the ongoing investigation into prescription drug pricing. The upcoming hearing will focus on the manufacturer AbbVie after Chairperson Carolyn Maloney (D–N.Y.) issued a notice of intent to subpoena for information related to two products under investigation, Humira and Imbruvica. In this post, we will recap the first 18 months of the investigation as the Biden–Harris administration and Congress consider policy options to rein in drug spending.
What Was the Scope of the Investigation?
After years of high drug prices, then-Chairperson Elijah Cummings announced a sweeping investigation into 12 drug companies’ pricing practices for 19 drugs. These high-cost drugs were selected because they represent a considerable share of spending for the Medicare Part D program. The investigation looked into company communications on price increases, investments in research and development (R&D), and corporate strategies to preserve market share and pricing power.
What Did We Learn from the 2020 Reports and Hearings?
Last fall, the committee released five reports and held two hearings with chief executives from some of the companies involved: Amgen, Bristol Myers Squibb, Celgene, Mallinckrodt, Novartis, and Teva. Several key takeaways highlighted drivers of high prescription drug prices and policy options to address the issue.
| Key finding | Examples from reports | Policy options to address |
| Pharmaceutical companies claim that investments in R&D are driving drug prices higher and policies to limit prices would harm innovation. But the reports found revenue and profit from drugs far exceeded companies’ R&D investment. | Many of the drugs under review, including those from Celgene, Novartis, and Mallinckrodt, relied heavily on publicly funded R&D; these companies did not need to recoup the full cost of development. Celgene’s internal documents suggested R&D funding for Revlimid was intended to generate a 114% return on investment. Between 2009 and 2016, Novartis was earning $100 million every 13 days on the drug, significantly outpacing any investments in R&D. |
Require manufacturer transparency on R&D costs. Allow the government to negotiate drug prices, taking into consideration public and private R&D expenditures. Require that manufacturers invest a threshold amount of revenues into R&D, similar to a medical loss ratio concept. |
| Industry has claimed that price increases are needed to fund R&D for new products and existing products. However, the investigation found that investments in R&D and price increases are not related. | Teva spent $689 million in R&D on Copaxone since 1987, which is 2% of the $34.2 billion in revenue it has made from the drug from 2002 to 2019. From 2003 to 2018, Amgen invested $2 billion in Enbrel R&D, which was 3.5% of its $58.23 billion in revenue over the same period. In recent years, this declined to 2.2% while the price went up. |
Limit price increases to inflation. Require that a certain amount of a drug company’s revenues be committed to R&D, similar to a medical loss ratio for health insurance companies. |
| List prices have continued to rise but drug manufacturers say list price is not an accurate reflection of the true price of a drug because it does not take into account rebates that reduce net prices. The investigation found several examples where companies offered no rebates or rebates did not offset list price increases. | For Revlimid, Celgene did not offer any rebates to Medicare Part D. The largest discount it paid in the commercial market was 5% despite the price increasing 34% from 2014 to 2019. Novartis did not offer any rebates to Medicare Part D between 2009 and 2014; Novartis’s rebate on Gleevec was 1% in 2015. Gleevec launched with an annual list price of $26,400 in 2001, by 2016 that price more than quadrupled to $120,000. Between 2014 and 2019, Amgen raised prices for Enbrel by 84% and for Sensipar by 34%. These increases outpaced any rebates paid. |
Require manufacturer transparency in pricing, including disclosure of list price, net price, and price increases. Allow the government to negotiate drug prices for Medicare Part D. Limit price increases to inflation. |
| Rebates are generally described as a tool for negotiating price and formulary placement of a drug between drug companies and prescription benefit managers (PBMs). The investigation found that rebates are used as a strategy to hold on to market share and block generic competition. | Teva tied rebates for one version of Copaxone to a requirement that PBMs cover a higher-dose version as part of a broader strategy to block generic competition. | Prohibit the practice of “rebate traps,” which attempt to block generic competition by requiring exclusionary or preferred formulary placement of a brand-name product in exchange for a rebate. |
| Drug companies claim to make drugs affordable to patients through patient-assistance programs. The investigation uncovered that patient-assistance programs are tools to increase sales and drive revenue. | Teva donated $97 million to subsidize Medicare Part D beneficiaries’ cost sharing. This resulted in $300 million in sales. The company’s patient-assistance program for commercial patients yielded a 451% return on investment. Novartis’s patient assistance program returned $8.90 for every dollar invested. |
Improve oversight of patient-assistance programs to require transparency. Exclude the value of these discounts from commercial insurance out-of-pocket maximums. Require programs to cover cost sharing for generic versions. |
Data: Author’s analysis of House Oversight and Reform Committee’s reports on drug pricing.
What Should We Expect in the AbbVie Report and Hearing?
The House Oversight and Reform Committee’s work highlights several drug manufacturers’ anticompetitive behaviors and patent abuses that could be addressed through policy reforms. Patent gaming received significant attention in the 2020 reports and hearings.
The next hearing in the ongoing investigation will focus on AbbVie. The committee’s work will likely center on the company’s use of the patent system to protect brand monopolies. A patent is granted 20 years of protection based on the date the application was filed with the U.S. Patent and Trademark Office (PTO). There are certain protections when a potential patent owner files an application, as it informs competitors that the intellectual property is under review at PTO. The patent owner may be able to seek damages for infringement during the time the patent was under review.
A recent report by I-MAK, a nonprofit organization focused on research related to prescription drug patents, found that the medication Imbruvica has 165 patent applications with 88 granted to date; 58 percent are for different indications and formulations. These are known as secondary patents because they are not based on the drug’s active ingredient. Imbruvica’s extended monopoly means it is protected for 29 years, which will account for an estimated $41 billion in drug spending by private and public payers as a result of delayed biosimilar entry. Similarly, Humira, one of the best-selling drugs in the world, has 247 patent applications, which are delaying competition for 39 years and costing Medicare and Medicaid billions in additional spending because there are no lower-cost biosimilars on the market.
Unlike the prior hearings, this one will focus exclusively on AbbVie — which produced two drugs that cost Medicare Part D nearly $7 billion in 2019 — as an example of how manufacturers block competition and use government programs to generate profits. Key themes will likely include the company’s activities to block competition, its high revenues generated from government programs, and policy options for patent reform.