By Isabelle Durand-Zaleski, AP-HP and Université Paris-Est
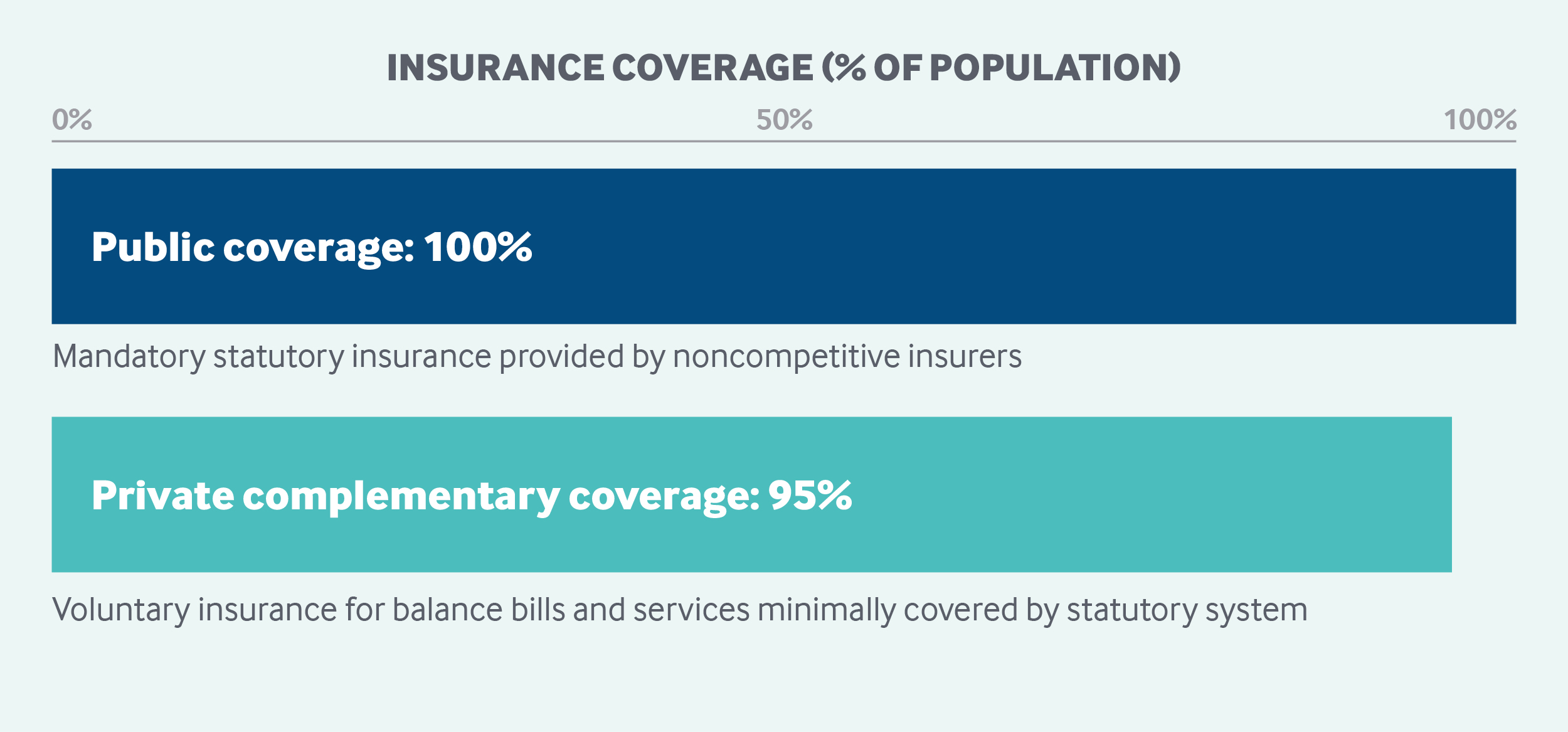
The French government sets the national health strategy and allocates budgeted expenditures to regional health agencies, which are responsible for planning and service delivery. Enrollment in France’s statutory health insurance system is mandatory. The system covers most costs for hospital, physician, and long-term care, as well as prescription drugs; patients are responsible for coinsurance, copayments, and balance bills for physician charges that exceed covered fees. The insurance system is funded primarily by payroll taxes (paid by employers and employees), a national income tax, and tax levies on certain industries and products. Ninety-five percent of citizens have supplemental insurance to help with these out-of-pocket costs, as well as dental, hearing, and vision care.
Sections
How does universal health coverage work?
Universal coverage was achieved over seven decades by extending statutory health insurance (SHI) to all employees (in 1945), retirees (in 1945), the self-employed (in 1966), and the unemployed (in 2000). In 2000, the Couverture maladie universelle (Universal Health Coverage), or CMU, was created for residents not eligible for SHI, although the program required yearly renewals and entitlement changes whenever a beneficiary’s professional or family situation changed. After the implementation of CMU, fewer than 1 percent of residents were left without baseline coverage.
In January 2016, SHI eligibility was universally granted under the Protection universelle maladie (Universal Health Protection law), or PUMa, to fill in the few remaining coverage gaps. The law also replaced and simplified the existing system by providing systematic coverage to all French residents. It merged coverage for persons previously covered by the Universal Health Coverage and immigrants covered by the state-sponsored health insurance.1
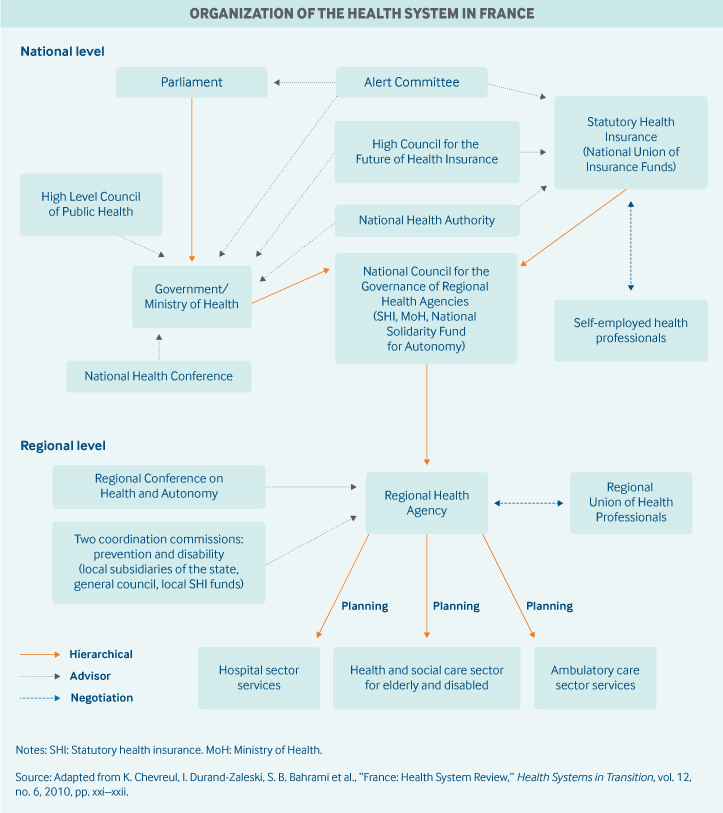
Role of government: The provision of health care in France is a national responsibility. The Ministry of Social Affairs, Health, and Women’s Rights is responsible for defining the national health strategy. It sets and implements government policy for public health as well as the organization and financing of the health care system.
Over the past two decades, the state has been increasingly involved in controlling health expenditures funded by SHI.2 It regulates roughly 75 percent of health care expenditures on the basis of the overall framework established by Parliament. The central government allocates budgeted expenditures among different sectors (hospitals, ambulatory care, mental health, and services for disabled residents) and regions.
The Ministry of Social Affairs, Health, and Women’s Rights is represented in the regions by the Regional Health Agencies, which are responsible for coordinating population health and health care, including prevention and care delivery, public health, and social care.
Other key government agencies include:
- The French Health Products Safety Agency, which oversees the safety of health products, from manufacturing to marketing.
- The Agency for Information on Hospital Care, which manages the information systematically collected from all hospital admissions and used for hospital planning and financing.
- The National Agency for the Quality Assessment of Health and Social Care Organizations, which promotes patient rights and develops preventive measures to avoid mistreatment, particularly in vulnerable populations such as the elderly and disabled, children, adolescents, and socially marginalized people. The agency also produces practice guidelines for the health and social care sector and evaluates organizations and services.
- The National Health Authority, the main health technology assessment body. In addition to assessing drugs, medical devices, and procedures, the agency publishes guidelines, accreditates health care organizations, and handles certification of doctors.
- The French Agency for numerical health (ASIP Santé), which seeks to expand the uptake and interoperability of existing health information systems.
- The Public Health Agency (Santé publique France), created in 2016 to protect population health. It conducts epidemiological surveys, scans for health threats, and pursues health protection and promotion efforts.
Role of public health insurance: Total health expenditures constituted 11.5 percent of GDP in 2017, which amounted to EUR 266 billion (USD 337 billion); 77 percent of those expenditures were publicly financed.3,4
SHI financing is supplied as follows5,6:
- Payroll taxes provide 53 percent of funding, with employers paying 80 percent of the tax and employees paying the rest; contributions are calculated from the actual salaries, capped at EUR 3,311 (USD 4,191) per month.
- A national earmarked income tax contributes 34 percent of funding.
- Taxes levied on tobacco and alcohol, the pharmaceutical industry, and voluntary health insurance (VHI) companies provide 12 percent of funding.
- State subsidies account for 1 percent of funding.
Coverage is compulsory, and is provided to all residents by noncompetitive statutory health insurance funds; historically, there have been 42 funds. Annual contributions are determined by Parliament. The SHI scheme in which workers enroll is based upon the type of employment. Unemployed persons are covered for one year after job termination by the SHI scheme of their employer and then by the universal health coverage law. Citizens can opt out of SHI only in rare cases, such as when they are employed by foreign companies.
The state finances health services for undocumented immigrants who have applied for residence. Visitors from elsewhere in the European Union (EU) are covered by an EU insurance card. Non-EU visitors are covered for emergency care only.
Role of private health insurance: Most voluntary health insurance (VHI) is complementary, covering mainly copayments and balance billing, as well as vision and dental care, which are minimally covered by SHI.
Complementary insurance is provided mainly by not-for-profit, employment-based associations or institutes. Private for-profit companies offer both supplementary and complementary health insurance, but only for a limited list of services. Voluntary health insurance finances 13.5 percent of total health expenditures.7 Ninety-five percent of the population is covered by VHI, either through employers or via means-tested vouchers (see more under “Safety nets,” below). As of 2016, all employees benefit from employer-sponsored VHI, for which employees pay at least 50 percent of the cost.
The extent of coverage varies widely, but all VHI contracts cover the difference between the SHI reimbursement rate and the official fee on the national fee schedule. Coverage of balance billing is also commonly offered.
In 2013, standards for employer-sponsored VHI were established by law to reduce inequities stemming from variations in access and quality.
Services covered: Covered benefits under SHI are defined at the national level by the Ministry of Social Affairs, Health, and Women’s Rights and the SHI funds, which are grouped under the National Union of Health Insurance Funds, or UNCAM, an umbrella organization. SHI covers the following:
- hospital care
- treatment in public or private rehabilitation or physiotherapy institutions
- outpatient care provided by general practitioners, specialists, dentists, physical therapists, and midwives
- all maternity care services, from the 12th week of pregnancy through six months after delivery
- newborn care and children’s preventive health care up to age 4
- diagnostic services prescribed by doctors and carried out by laboratories and paramedical professionals
- prescription drugs
- medical appliances, including durable equipment such as wheelchairs and prostheses, that have been approved for reimbursement
- prescribed health care–related transportation and home care.
SHI also partially covers long-term hospice and mental health care and provides minimal coverage of vision care, hearing aids, and dental care.
In general, there is limited coverage of preventive care; however, there is full reimbursement for priority services — immunizations, mammograms, and colorectal cancer screenings, for example — as well as for preventive care for children and low-income populations.
Injection sites under the supervision of health professionals were legalized in 2015 for the treatment of especially vulnerable drug addicts; these are fully covered under SHI until 2021.8
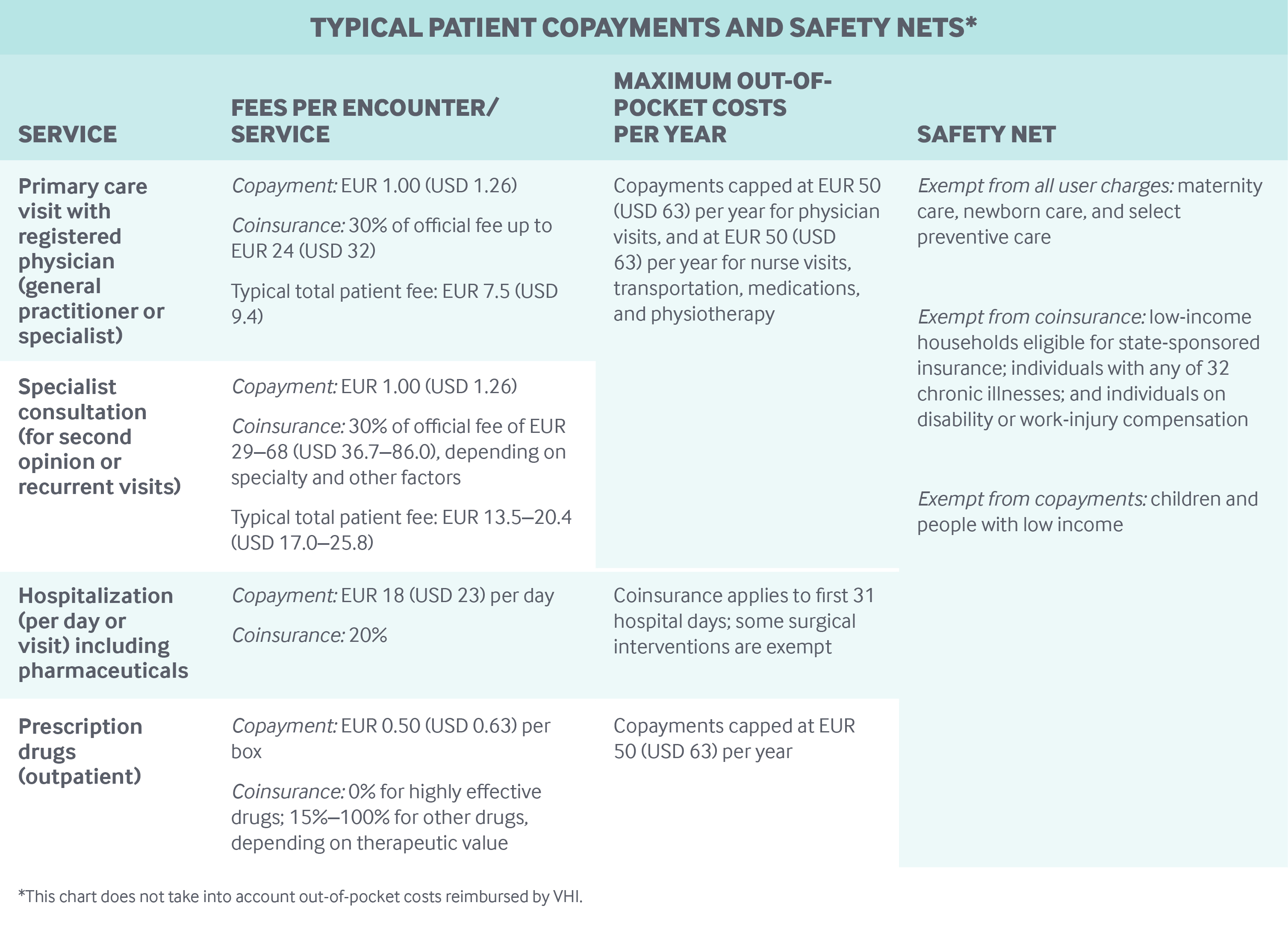
Cost-sharing and out-of-pocket spending: There are no deductibles. Cost-sharing for primary and specialist care takes three forms: coinsurance, copayments, and balance billing. Some physicians are allowed to balance-bill above the national fee schedule; authorization is based upon the duration of their hospital residency.
In 2015, total out-of-pocket spending made up 7 percent of total health expenditures (excluding the portion covered by supplementary insurance). This share has been decreasing in recent years, probably because of an agreement signed between physicians’ unions and the government to cap balance billing at twice the official fee. This contract also offers patients partial reimbursement of balance billing through SHI and reduced social contributions for physicians.
Most out-of-pocket spending is for dental and vision services. Official fees for these services are very low, no more than a few euros for glasses or hearing aids, and the maximum fee for dentures is EUR 200 (USD 253). But providers commonly balance-bill for these services at more than 10 times the official fee. However, the share of out-of-pocket spending on dental and optical services has been decreasing because of higher voluntary health coverage for these services.
At the same time, out-of-pocket expenditures on drugs have been steadily growing because more prescription drugs are being taken off the national formulary. The number of over-the-counter drugs has also risen.
The table below lists copayments for various services. Coinsurance rates are applied to all health services and drugs listed in the benefit package and vary by:
- Type of care: 20 percent for inpatient stays, 30 percent for outpatient doctor and dentist visits.
- Effectiveness of prescription drugs: highly effective drugs like insulin carry no coinsurance, while rates for all other drugs range from 15 percent to 100 percent, depending on the drug’s therapeutic value, whether patients seek a referral from their primary care provider, and whether they seek specialist care or treatments directly without a referral.
Hospital coinsurance applies only to the first 31 days in hospital, and some surgical interventions are exempt; there are no caps on other coinsurance.
Safety nets: People with low incomes are entitled to free or discounted health insurance, free vision care, and free dental care. Individuals are considered low-income if they make EUR 8,723 (USD 11,040) or less per year. For households, the qualifying income level increases with each member. The total number of low-income beneficiaries is estimated at around 9 percent of the population, with 6 percent receiving means-tested vouchers for VHI and 3 percent getting free state-sponsored coverage.
How is the delivery system organized and how are providers paid?
Physician education and workforce: Once a year, the Ministry of Social Affairs, Health, and Women’s Rights determines the maximum number of students that can be admitted to medical, dental, midwifery, and pharmacy schools, which are all public by law. Tuition fees are approximately EUR 500 (USD 633) per year.
The number of medical professionals is controlled at the point of entry into medical education. In addition, 12 percent of the current medical workforce are foreign-trained medical professionals. To date, there are no limitations on the number of practicing physicians by region. However, since 2013, outpatient physicians can enter into contractual agreements that guarantee a monthly salary of EUR 6,900 (USD 8,734) if they practice in a region with insufficient physician supply and agree to limit extra billing. For physicians who work full-time in medical centers in underserved areas, the guaranteed salary is approximately EUR 50,000 (USD 63,290) per year.
Primary care: There are roughly 102,299 general practitioners (GPs) and 121,272 specialists in France (a ratio of 3.4 per 1,000 population). About 59 percent of physicians are self-employed on a full-time or part-time basis (67% of GPs, 51% of specialists).9
More than 50 percent of GPs, predominantly younger doctors, are in group practices. An average practice is made up of two-to-three physicians. Seventy-five percent of practices are made up exclusively of physicians; the remaining practices also include nurses and a range of allied health professionals. The average patient panel size is about 900 patients for GPs.
There is a voluntary gatekeeping system for people aged 16 and older, with financial incentives offered to those who opt to register with a GP or specialist. About 95 percent of the population have chosen a GP as their gatekeeper, but specialists can also serve as gatekeepers.
Self-employed GPs are paid mostly on a fee-for-service basis, with fees determined by SHI funds and the Ministry of Social Affairs, Health, and Women’s Rights. In 2018, GP fees were EUR 25 (USD 32) per consultation. GPs can also receive a capitated per-person annual payment of EUR 40 (USD 51) to coordinate care for patients with chronic conditions. In addition, GPs receive an average of EUR 5,000 (USD 6,330) a year for achieving pay-for-performance targets.
In 2014, the average income of primary care doctors was EUR 86,000 (USD 108,860), 94 percent of which came from fees for consultations and the remainder from financial incentives and salary.10
GPs can bill above the national fee schedule, and 25 percent do. Specialists earn, on average, 1.3 times what GPs earn.
Experimental GP networks are being piloted that provide chronic-care coordination, psychological services, dietician services, and other care not covered by SHI. These networks are financed by earmarked funds from the Regional Health Agencies. In addition, more than 1,000 medical homes provide multi-professional services (usually with three-to-five physicians and roughly a dozen other health professionals) and after-hours care.
Outpatient specialist care: About 36 percent of outpatient specialists are exclusively self-employed, either in offices or private clinics, and are paid on a fee-for-service basis; the rest either are fully salaried hospital employees or have a mix of income sources.
Specialists working in public hospitals may see private-pay patients on either an outpatient or an inpatient basis, but they must pay a percentage of their earned fees to the hospital. A 2013 report estimated that 10 percent of the 46,000 hospital specialists in surgery, radiology, cardiology, and obstetrics had treated private patients.
Half of specialists are in group practices, and this percentage is increasing among specialties that require major investments in technology and equipment to serve patients, such as nuclear medicine, radiotherapy, pathology, and digestive surgery. The specialist fee set by SHI ranges from EUR 25 (USD 32) to EUR 69 (USD 88). Specialists can balance-bill, and nearly 43 percent do.
The average yearly income of self-employed specialists is EUR 140,610 (USD 177,800).11 All specialists who are self-employed can participate in pay-for-performance programs. Specialists must meet disease-specific quality targets in addition to those targets that apply to GPs. The average annual income derived from pay-for-performance is EUR 5,480 (USD 6,937) per physician, which constitutes less than 2 percent of total funding for outpatient services.
Patients with a referral can choose among specialists. Seeing a specialist without a referral from a gatekeeping physician results in reduced SHI coverage. However, some specialists can be directly accessed without a referral, including gynecologists, ophthalmologists, psychiatrists, and stomatologists.
Administrative mechanisms for direct patient payments to providers: Patients pay the full fee (reimbursable portion and balance billing, if any) at the end of a physician visit. After the insurance claim is filed, patients are reimbursed the full sum or less, depending on their coverage, minus the copayment.
After-hours care: After-hours care is organized by the Regional Health Agencies and delivered by contracted hospital emergency departments, self-employed physicians who work for emergency services, and medical homes financed by SHI and staffed by doctors and nurses on a voluntary basis. Primary care physicians are not mandated to provide after-hours care.
There is no systematic method to ensure that information from the patient visit is transferred to the patient’s GP.
There is currently no national or regional medical advice phone service, but teleconsultation became legal in September 2018 and can be used for after-hours care in certain localities.
Hospitals: Public institutions account for about 65 percent of hospital capacity and activity. Private for-profit facilities account for another 25 percent, and private nonprofit facilities make up the remainder.
All hospitals are reimbursed under SHI via the diagnosis-related group (DRG) system set by the Ministry of Social Affairs, Health, and Women’s Rights, which applies to all inpatient and outpatient admissions and covers all medical services and physicians’ salaries in public and not-for-profit hospitals. Neither bundled payment nor performance incentives exist.
Hospitals are reimbursed for certain expensive and innovative drugs and devices in addition to the DRG tariff. A list of covered drugs and devices is updated every year by the Ministry of Social Affairs, Health, and Women’s Rights, based on semitransparent criteria of innovativeness, price, and the share of the DRG population requiring the innovative drug or device.
Public hospitals are funded mainly by SHI (80%), with voluntary insurance and direct patient payments accounting for their remaining income. Public and private nonprofit hospitals also receive research and teaching grants (up to 13% of hospital budgets) and provisions for providing emergency services, organ harvesting, and organ transplantation (on average, 10%–11% of budget).
Private, for-profit clinics owned either by individuals or, increasingly, by large corporations have the same funding mechanism as public hospitals, but the share of respective payers differs. Physician fees are billed in addition to the DRG in private clinics, and DRG payment rates are lower there than they are in public or nonprofit hospitals.
Mental health care: Services for people with mental illness are provided by both the public and the private health care sector, with an emphasis on community-based provision. Public care is provided within geographically determined areas and includes a wide range of preventive, diagnostic, and therapeutic inpatient and outpatient services. Ambulatory centers provide primary ambulatory mental health care, including home visits.
SHI covers mental health care provided by GPs and psychiatrists in private practice, public mental health care clinics, and private psychiatric hospitals. Care provided by psychologists, psychotherapists, or psychoanalysts is fully paid by patients or covered by VHI. Copayments and the flat-rate fee for accommodation can also be fully covered by VHI. Copayments do not apply to persons with diagnosed long-term psychiatric disorders, including schizophrenia, bipolar disorder, severe anxiety, and depression.
Mental health care is not formally integrated with primary care, but a large number of disorders are treated on an outpatient basis by GPs or private psychiatrists or psychologists.
Long-term care and social supports: Health and social care for elderly and disabled people comes under the jurisdiction of the General Councils, which are the governing bodies at the local (departmental) level. The total number of frail elderly is estimated at about 1.25 million, or 2 percent of the population.12 Total expenditures for long-term care were estimated to be EUR 30 billion (USD 37.9 billion) in 2015, or 1.7 percent of GDP.13
Institutional long-term care is provided in retirement homes and long-term care units, totaling roughly 10,000 institutions with a total of 728,000 beds.10 Of these institutions, currently 54 percent are public, 28 percent private nonprofit, and 18 percent for-profit, although the percentage of for-profit institutions is increasing.
SHI covers the medical costs of long-term care in facilities, while families are responsible for the housing costs. These out-of-pocket costs average EUR 1,500 (USD 1,900) per month, some of which can be covered by VHI. End-of-life care in hospitals is fully covered.
Funding of home care and services for the elderly and disabled comes from the National Solidarity Fund for Autonomy, which is financed by SHI and the revenues from an unpaid working solidarity day. One day a year, employers pay the SHI their employees’ daily wages. Local authorities, the General Councils, and households also participate in financing these categories of care.14
Home care for the elderly is provided mainly by self-employed physicians and nurses and, to a lesser extent, by community nursing services. It is covered by SHI and VHI, based on medical need; there is no means testing.
In addition, temporary care for dependent patients and respite services for their caregivers are available without means testing from the states or regions.
Means-tested cash allowances are provided to the frail elderly to pay for in-kind nonmedical services. The allowances are adjusted in relation to the individual’s dependence level, living conditions, and needs, and may be used for any chosen service and provider. About 1.1 percent of the total population is estimated to be eligible. Informal caregivers also benefit from tax deductions but do not receive a cash allowance.
To address the loss of autonomy among the elderly, a law enacted at the end of 2015 established local conferences of stakeholders that meet yearly to define priorities, identify existing services, and create new programs as necessary.15
What are the major strategies to ensure quality of care?
An average of EUR 5,000 (USD 6,330) per physician annually is provided for achieving pay-for-performance targets related to the following:
- use of computerized medical charts
- adoption of electronic claims transmission
- delivery of preventive services, such as immunizations
- compliance with guidelines for diabetic and hypertensive patients
- generic prescribing
- limited use of psychoactive drugs for elderly patients.
Population health surveys are undertaken based on disease, population segment (such as newborns, students, elderly patients), or theme (like nutrition). In addition, there are regional disease-based registries for specific conditions, including cancer, multiple sclerosis, and congenital abnormalities. The CONSTANCES Cohort is a 200,000-person representative sample of the population, surveyed yearly with linkages to the national claims database. National surveys showing regional variations in health and access to health care are publicly reported.
There are national strategies for the treatment of chronic conditions like cancer and for rare diseases, as well as for prevention and healthy aging. These plans establish governance, develop tools, and coordinate participating organizations. For example, the national cancer plan sets goals for coordinating cancer research and treatment and establishes medical practice guidelines as well as minimum volume thresholds for complex procedures. All plans emphasize the importance of supporting caregivers and ensuring patients’ quality of life, in addition to enforcing compliance with guidelines and promoting evidence-based practice.
To date, the National Health Authority has published evidence-based basic benefit packages for 32 chronic conditions. These benefit packages describe all the services needed for patients with those chronic conditions. Further guidance on recommended care pathways covers chronic obstructive pulmonary disease, heart failure, Parkinson’s, and end-stage renal disease.
Provider networks of participating professionals share clinical guidelines and protocols, agree on best practices, and have access to a common patient record. In addition, telemedicine pilot programs aim to improve care coordination and access to care for specific conditions or populations, like newborns or the elderly.
For self-employed physicians, certification and revalidation are organized by independent bodies, such as medical societies approved by the National Health Authority. For hospital physicians, certification and revalidation can be performed as part of the hospital accreditation process.
Doctors, midwives, nurses, and other professionals must participate in continuous medical education activities, which are audited every fourth or fifth year. Optional accreditation exists for a number of high-risk medical specialties, such as obstetrics, surgery, and cardiology. Accredited physicians can claim a deduction on their professional insurance premiums.
Hospitals must be accredited every four years; criteria and accreditation reports are publicly available on the National Health Authority website ( www.has-sante.fr). CompaqH, a national program of performance indicators, also reports results on selected indicators. Quality assurance and risk management in hospitals are monitored nationally by the Ministry of Social Affairs, Health, and Women’s Rights, which posts hospital-acquired infection rates and other information online. Information on individual physicians is not available. Currently, financial rewards or penalties are not linked to public reporting, although the issue remains contested.
Nursing homes are also accredited by the National Health Authority (formerly by the Agence Nationale d’Evaluation Sociale et Médico-sociale) with a specific focus on preventing elder abuse. Home care provided by hospital subsidiaries is accredited by the National Health Authority with public reporting available online.
What is being done to reduce disparities?
Reducing disparities in regard to social determinants of health and access to care is a national priority. There is a 6.3-year gap in life expectancy between males in the highest social category and those in the lowest,16,17 and poorer self-reported health among those with state-sponsored insurance and no VHI.
The 2004 Public Health Act set targets for reducing geographic and financial inequities in access to services and inequities in preventive care related to obesity, cancer screening, and immunization. Toward these goals, disparities are being addressed through physician contracts. For example, financial incentives encourage physicians to practice in underserved areas. Furthermore, physician contracts under SHI prohibit physicians from denying care to beneficiaries of state-sponsored health insurance and put a cap on balance billing.
There are published national statistics on nutrition, physical activity, and tobacco use, analyzed by social class and type of employment.18 Differences in access to care are measured by participation in systematic screening programs and differences in health outcomes.
In March 2018, the Minister of Health presented the national plan to reduce health inequities with a EUR 400 million (USD 506 million) investment over five years and 25 measures that concern all age groups.19
What is being done to promote delivery system integration and care coordination?
Inadequate coordination in the health care system remains a problem. In addition to financial incentives provided to GPs (EUR 40 per patient with a chronic condition), various quality-related initiatives aim to improve the coordination of hospital, out-of-hospital, and social care. They target the elderly and fragile populations and attempt to streamline the health care pathway, integrating providers of health and social care through the use of case managers and a shared portal for both communication and data sharing. The Health Pathway of Seniors for Preserved Autonomy was launched five years ago to improve the coordination of care for the elderly. It did not improve health outcomes as expected, but will nevertheless be continued until the end of 2019.20
What is the status of electronic health records?
The electronic health record (EHR) project (Projet dossier medical partagé) covered roughly 1,882,503 patients at the end of 2018, and an estimated 731 hospitals (one-third of all hospitals). Hospital-based and office-based professionals and patients have a unique electronic identifier, and any health professional can access the record and enter information subject to patient authorization. Interoperability is ensured via a chip on patients’ health cards.21
The initiative to fully integrate EHRs has faced multiple delays, and the integration of information systems between health care professionals and hospitals remains limited.22 By law, patients have full access to the information in their own records, paper or electronic, either directly or through their GP. The sharing of information between health and social care professionals is planned as part of the deployment of EHRs to nursing homes, which started in 2019.23
How are costs contained?
SHI has faced large deficits over the past 20 years, but they have fallen from EUR 10–12 billion (USD 12.6 –15.2 billion) in 2003 to EUR 4.1 billion (USD 5.2 billion) in 2016.24 This trend is the result of a range of initiatives, including:
- a reduction in the number of acute-care hospital beds
- the removal of 600 drugs from public reimbursement
- an increase in generic prescribing
- a reduction in the price of generic drugs
- the use of over-the-counter drugs
- a reduction of official fees for self-employed radiologists and biology labs
- the inclusion of central purchasing to better negotiate costs
- an increase in the proportion of outpatient surgery
- the institution of earlier post-surgery and post-delivery discharge
- a reduction in duplicate testing.
Competition is not used as a cost-control mechanism in SHI.
Global budgets are used only in price-volume agreements for drugs or devices. Patient cost-sharing mechanisms include increased copayments for patients who refuse generics or do not use the voluntary gatekeeping system.
The increasing price of drugs is being addressed through an increased use of generic and biosimilars incentivized by the pay-for-performance scheme, price-volume agreements, and undisclosed rebates with manufacturers.
There are also a number of initiatives to reduce low-value care, launched by SHI and the National Health Authority, including25:
- reductions in avoidable hospital admissions for patients with heart failure
- early discharge after orthopedic surgery and normal childbirth
- the use of DRG payments to incentivize shifts to outpatient surgery
- the establishment of guidelines for the number of allowable off-work days according to disease or procedure
- strengthened controls over the prescription of expensive statins and new anticoagulants
- incentives for the use of less-costly biosimilar drugs.
What major innovations and reforms have recently been introduced?
A controversial part of the 2015 Touraine law recommended making physician consultations totally free at the point of care: practitioners would be paid directly by social security and SHI for all visits. However, in view of the strong opposition from doctors, the extension of third-party payment to the entire patient population has been postponed indefinitely.
The mounting discontent over excessive balance billing revealed in the press, together with claims by private clinics of unfair competition, has prompted several public inquiries. The latest inquiry resulted in recommendations to increase public control over these activities.
Experiments with new payment mechanisms are in their early stages. These experiments are inspired by the creation of accountable care organizations. At the national level, bundled payments are to be tested in 2019–2020 for orthopedic and colorectal surgeries. In addition to the national program, regional initiatives are encouraged, with the objectives of integrating care and improving quality, relevance, efficiency, and prevention. These five criteria will be considered when decisions are made as to whether to allow regional pilots, which will run for a period of five years and benefit from funding of care not currently covered by SHI. Disease types selected are stroke, heart failure, and acute coronary syndromes. A total budget of EUR 20 million (USD 25.3 million) is earmarked for 2019 for the payment pilots.

