Abstract
The Affordable Care Act gives states the option of providing less-generous Medicaid coverage to adults who become eligible through the law’s expansion of the program. Based on a review of the benefit design choices made by states that had expanded Medicaid by the end of 2014, we find that states have chosen to offer more generous coverage than what is required under federal law, either narrowing or eliminating the distinction between coverage levels for newly eligible adults and those for traditional adult beneficiaries, such as pregnant women, parents and guardians, or beneficiaries with disabilities. This suggests that states view the newly eligible beneficiaries as having the elevated health and health care needs that are common among low-income populations.
OVERVIEW
The Affordable Care Act (ACA) gives states the option of expanding Medicaid coverage to nonelderly adults ages 19 to 64 with incomes at or below 138 percent of the federal poverty level who do not fall into other eligibility categories (as parents or caretaker relatives of dependent children, pregnant women, adults receiving Medicare based on disability, or other adults with disabilities). The law also provides states with flexibility to choose the level of coverage provided to such adults. The coverage model is based on a benchmark linked to the benefit designs used by private insurers, rather than the broader coverage rules used for traditional Medicaid beneficiaries.
How states are implementing this benchmark approach to coverage is an important consideration for Medicaid policymakers. In particular, do states tend to view newly eligible adults as different from traditional adult beneficiaries in terms of their health and health care needs? In this brief, we describe the evolution of insurance benchmark design and present findings from our review of state benchmark coverage standards for newly eligible adults.
ORIGINS OF THE AFFORDABLE CARE ACT'S BENCHMARK COVERAGE STANDARD
The ACA’s benchmark coverage standard for newly eligible adults builds on longstanding precedent, with roots in the Children’s Health Insurance Program (CHIP) and the Deficit Reduction Act (DRA) of 2005.1
Children’s Health Insurance Program
Enacted in 1997, CHIP offers states two basic approaches to coverage design: traditional Medicaid benefits in states that use CHIP financing in whole or in part to expand Medicaid; and “benchmark” coverage in states that use their CHIP allotment in whole or in part to establish separate CHIP programs. States using a benchmark coverage approach have the option to define “child health assistance” in relation to one of several private health insurance benchmarks: coverage offered under the Federal Employees Health Benefits Program; the state employee plan; or the largest commercial HMO plan offered in the state. Alternatively, states can fashion a “benchmark equivalent” plan for approval by the Secretary of the U.S. Department of Health and Human Services (HHS); such plans must have an actuarial value equal to one of the named benchmarks.
In all cases, CHIP plans must cover certain benefits at a minimum: inpatient and outpatient hospital services, physicians’ surgical and medical services, laboratory and X-ray services, dental care, and well-baby and well-child care, including age-appropriate immunizations.2 States also may cover other services, including vision and hearing care and prescription drugs.3 Moreover, states can choose to supplement these services with additional categories of covered benefits, such as durable medical equipment or speech and physical therapy. Mental health parity requirements apply to CHIP plans.
Deficit Reduction Act
The Deficit Reduction Act builds on the CHIP model by giving state Medicaid programs the flexibility to substitute “benchmark benefits” for traditional Medicaid coverage for certain groups of beneficiaries, while requiring states to maintain traditional coverage rules for “medically frail” and other beneficiaries considered to have higher health needs.4 As with CHIP, the DRA requires that states electing this option select a “benchmark benefit plan” tied to a private insurance benchmark: the Federal Employees Health Benefits Program; the state employee plan; or the largest commercial HMO plan offered in the state. The law permits states to create a “benchmark equivalent” plan subject to approval by the HHS secretary, as does CHIP, and establishes a similar minimum “basic services” requirement for benchmark plans.5
Finally, like CHIP, the DRA permits states to supplement basic benchmark benefits with additional services—prescription drugs, mental health treatment, and vision and hearing treatment. The value of these supplemental benefits must satisfy a 75 percent actuarial equivalency standard; that is, federal funding is conditioned on the value of supplemental benefits reaching at least 75 percent of claims for a standard population. The DRA also requires states to augment benchmark benefits with certain treatments and services covered under their traditional Medicaid plans: Medicaid’s comprehensive early and periodic screening, diagnosis, and treatment (EPSDT) benefits for children up to age 19 (later raised to 21), and services delivered in federally qualified health centers and rural health clinics.6
The Affordable Care Act Amendments
To determine the scope of coverage for adults newly eligible for Medicaid, the ACA builds on the DRA benchmark approach while modifying it in key respects.7 First, the ACA substitutes the essential health benefit standard for the DRA’s “basic services” standard, thereby ensuring that 10 categories of service the ACA deems “essential” are part of benchmark coverage.8 For some preventive services (e.g., colorectal cancer screening, mammography, and adult immunizations), the essential health benefit standard may be more generous than that for traditional adult Medicaid beneficiaries, for whom most clinical preventive services are optional. Most states cover some, but not all, preventive services required under the essential health benefit standard.9
Second, the ACA extends mental health parity rules to plans providing Medicaid benchmark benefits—meaning that such plans cannot apply lifetime or annual dollar limits on mental health services that are more restrictive than those for medical services.10 Third, the ACA carries over to benchmark benefit coverage the traditional Medicaid rule guaranteeing free choice of family planning providers for those in managed care plans, regardless of provider network restrictions that would otherwise apply.11 The ACA also retains: the earlier benchmark exemption for medically frail and special needs beneficiaries, the EPSDT coverage standard for individuals under age 21, coverage of services provided in federally qualified health centers and rural health clinics, and states’ flexibility to add traditional state plan services to their benchmark plans. In addition, in implementing the ACA benchmark coverage reforms, the Centers for Medicare and Medicaid Services (CMS) also has added coverage of nonemergency medical transportation.
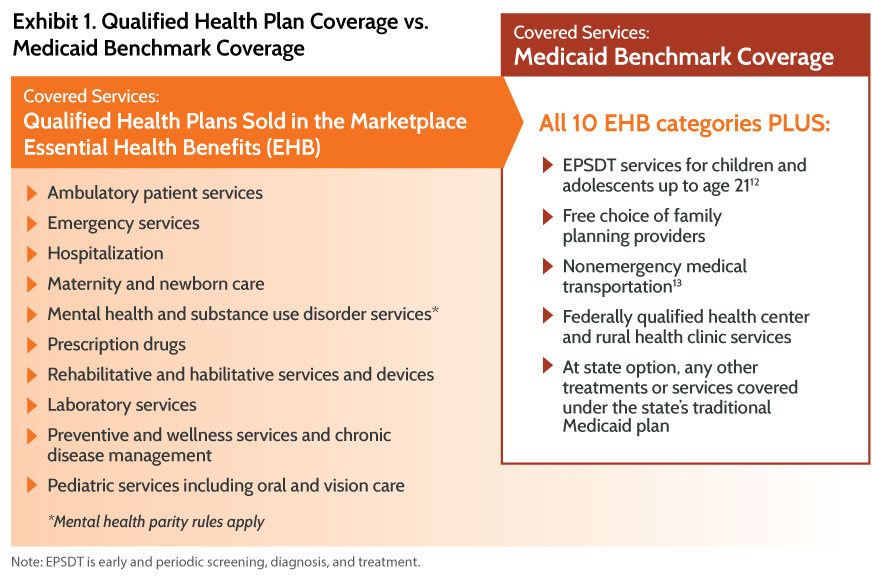
The result of these changes is that newly eligible Medicaid beneficiaries entitled to benchmark coverage receive the same benefits as those available under qualified health plans sold in the health insurance marketplace, plus additional benefits. In addition, states may further supplement benchmark coverage with treatments and services covered under their traditional Medicaid plans (Exhibit 1).
Benchmark coverage for newly eligible Medicaid adults is furnished through “alternative benefit plans”14 (ABPs), the term used to describe Medicaid managed care arrangements that comply with Medicaid’s benchmark benefit requirements. These plans must meet all of the requirements that apply to traditional Medicaid managed care plans.
HOW ARE STATES USING THEIR BENCHMARK COVERAGE FLEXIBILITY?
Traditional Medicaid coverage tends to be more comprehensive and generous than private health insurance, even private plans subject to the ACA’s essential health benefit requirements. For example, many state Medicaid programs cover certain classes of benefits (such as vision and oral health care) that are not part of the essential health benefit package for adults. Similarly, many Medicaid programs cover certain treatments in greater amount, duration, and scope than the level offered under private health insurance, such as care for patients with serious physical and mental disabilities. In addition, federal Medicaid law requires coverage of all FDA-approved drugs with rebate agreements—a far higher standard of coverage than that required for private health plans subject to the essential health benefit coverage standard.
Medicaid’s broader coverage standards are important, since the program is designed to address the needs of medically and economically vulnerable populations. As a group, newly eligible Medicaid adults may be in somewhat better health than the traditional adult population (which includes many people with severe disabilities).15 Still, the newly eligible adult population is likely to have a relatively high proportion of previously uninsured adults with serious physical and mental health conditions. Some of these adults will require more intensive services because their conditions went untreated while they were uninsured.16 This might encourage states to offer benchmark coverage with more robust services than are covered through essential health benefits.
We examined whether and how states are supplementing the minimum benchmark benefit requirements through analysis of state plan documents related to benchmark coverage for the 27 states and the District of Columbia that, as of December 2014, had expanded their Medicaid programs. This research sheds light on the question of whether and if so how states distinguish between traditional and newly eligible Medicaid beneficiaries in terms of their health care needs.
What We Found
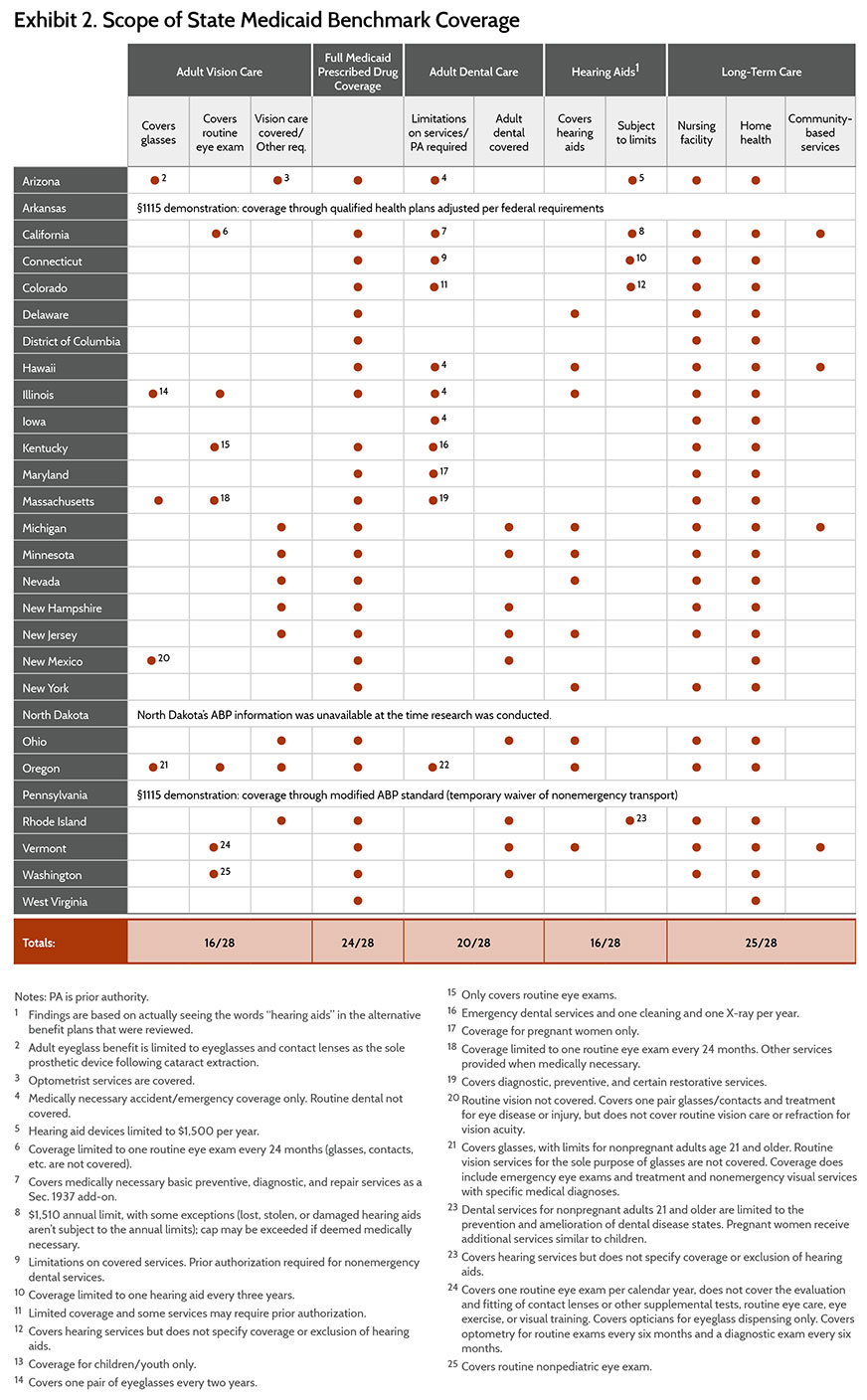
Our findings are presented in Exhibit 2. First, the 27 states plus D.C. all chose “benchmark equivalent” coverage, creating their own benchmarks for approval by the HHS Secretary rather than modeling them on private insurance coverage.17 Most states used their small-group plans as the starting point for the benefits to be offered under benchmark coverage.18
Notably, all of the states chose to bring their benchmark coverage up to the levels offered under their traditional Medicaid plans. In particular, each state’s ABP (except Iowa) includes supplemental prescription drug coverage on par with that provided to traditional Medicaid beneficiaries. Most states also supplemented their benchmark coverage, at least to some degree, with respect to long-term care, vision and oral health care, and hearing aids.
CONCLUSION
Under the ACA’s “benchmark benefit” authority, states have the flexibility to design Medicaid benefits and coverage for newly eligible adults. States can elect to follow the same essential health benefit standard applicable to qualified health plans sold in the health insurance marketplace, with certain supplementation required in the case of beneficiaries under age 21, family planning services, nonemergency transportation, and services provided in federally qualified health centers or rural health clinics. Alternatively, states can move beyond this minimum standard, offering a level of coverage comparable to that available to traditional adult Medicaid beneficiaries. Our analysis found that all states that have expanded Medicaid eligibility have chosen to supplement benchmark coverage for newly insured adults—through additional types of covered benefits as well as a broader amount and scope of benefits than what’s required under the essential health benefit standard. In particular, nearly all states have chosen to offer generous prescription drug coverage, and at least some vision and dental benefits (neither vision nor dental benefits are offered to adults under the essential health benefit standard).
These findings suggest that states view the newly eligible adult Medicaid population as closely aligned with traditional adult beneficiaries. They are extremely poor and likely to have been previously uninsured; many have health problems and some have gone without care for years.19 For such reasons, it makes sense that states expanding Medicaid would design coverage for newly eligible adults much as they have done for traditional beneficiaries.
Notes
1 Pub. L. 109-171 §6044, adding §1937 of the Social Security Act, 42 U.S.C. §1396u-7.
2 42 U.S.C. §1397cc(1) and (5).
3 42 U.S.C. §1397cc(2).
4 The law identifies, among other high-need groups, pregnant women, beneficiaries dually eligible for Medicare and Medicaid, beneficiaries receiving coverage based on a breast or cervical cancer diagnosis, or children in foster care.
5 42 U.S.C. §1396u-7(b)(1) and (2).
6 42 U.S.C. §1396u-7(b).
7 PPACA §2001, amending 42 U.S.C. §1396u-7.
8 Under the ACA, essential health benefits consist of 10 broad benefit classes: ambulatory patient services; emergency services; hospitalization; maternity and newborn care; mental health and substance use disorder services; prescription drugs; rehabilitative and habilitative services and devices; laboratory services; preventive and wellness services including chronic disease management; and pediatric services including vision and oral care.
9 A. Kates, U. Ranji, and L. Snyder, Coverage of Preventive Services for Adults in Medicaid (Menlo Park, Calif: Kaiser Family Foundation, Nov. 2014), available at http://files.kff.org/attachment/coverage-of-preventive-services-for-adults-in-medicaid-issue-brief. The ACA offers a modest incentive (a 1% increase in federal funding) to states that upgrade their preventive services coverage under their traditional programs. As of the end of 2014, the Kaiser Family Foundation reported that eight states had submitted proposals to CMS to expand adult preventive services.
10 42 U.S.C. §18022(j).
11 42 U.S.C. §1396u-7(b)(7).
12 The EPSDT coverage standard would govern the scope of pediatric coverage under an alternative benefit plan in the case of children and adolescents up to age 21. EPSDT requires comprehensive assessments of physical, mental, and developmental health; coverage of vision, dental and hearing care; and all medically necessary treatments and services falling within Medicaid’s definition of “medical assistance,” regardless of whether services are covered for persons age 21 and older.
13 Added by benchmark CMS regulation.
14 CMS, Medicaid Highlights of the Final Rule: Alternative Benefit Plans and Essential Health Benefits, http://www.medicaid.gov/State-Resource-Center/Eligibility-Enrollment-Final-Rule/Alternative-Benefit-Plans-and-Essential-Health-Benefits.pdf, accessed Jan. 12, 2015.
15 S. Decker, D. Kostova, G. Kenney et al., “Health Status, Risk Factors, and Medical Conditions Among Persons Enrolled in Medicaid vs. Uninsured Low-Income Adults Potentially Eligible for Medicaid Under the Affordable Care Act,” Journal of the American Medical Association, June 26, 2013 309(24):2579–86.
16Low-Income Adults Under 65—Many Are Poor, Sick and Uninsured (Menlo Park, Calif.: Kaiser Family Foundation, June 2009), available at http://kaiserfamilyfoundation.files.wordpress.com/2013/01/7914.pdf.
17 Arkansas and Pennsylvania maintain their coverage standards via their §1115 demonstrations rather than as a state plan amendment. Arkansas purchases qualified health plans from the insurance marketplace and supplements plans in accordance with the federal requirements. Pennsylvania provides a modified version of the alternative benefit plan required under law, with a temporary waiver of nonemergency medical transportation. Otherwise the state is obligated to maintain an alternative benefit plan standard known as the private coverage option. See https://www.medicaid.gov/Medicaid-CHIP-Program-Information/By-Topics/Waivers/1115/downloads/pa/Healthy-Pennsylvania-Private-Coverage-Option-Demonstration/pa-healthy-ca.pdf.
18 Recall that the ACA required Medicaid benchmark plans to supplement the “basic services standard” with an essential health benefits package.
19 A. Driscoll and A. Bernstein, Health and Access to Care Among Employed and Unemployed Adults: United States 2009–2010, NCHS Data Brief #83 (Washington, D.C.: Centers for Disease Control and Prevention, Jan. 2012) http://www.cdc.gov/nchs/data/databriefs/db83.pdf.
