As states confront their most challenging budgets in decades alongside new responsibilities to implement national health reform, many are looking at opportunities to improve long-term care as a way to control costs and serve seniors and people with disabilities in the settings they prefer. This issue of States in Action describes provisions in the Affordable Care Act that assist states in expanding home- and community-based long-term care services, the growing grassroots movement to improve facility-based care, and innovative programs in Colorado, Michigan, and Rhode Island that seek to provide consumer-directed long-term care.
Long-Term Care Services and Supports
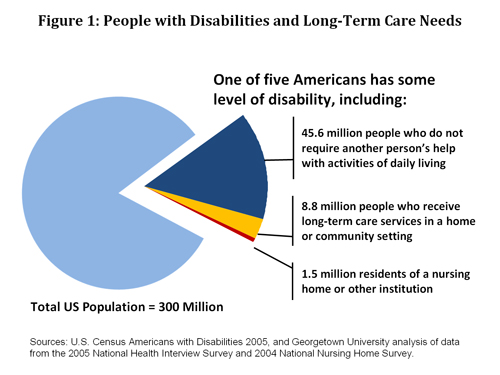
One of five Americans—56 million people—report having a disability that limits routine activities of daily living. Among this population, about 10.3 million people require long-term care, which includes a variety of medical and social services to help meet health or personal needs. Most long-term care is to assist people with basic tasks, such as eating or bathing, or activities necessary for independence, such as preparing meals or managing money. And most people who need long-term care services and supports (85%) receive them at home or in community-based settings, such as a daytime activity center. However, a significant number of people who require long-term care—1.5 million—reside in nursing homes or other facilities that attend to their long-term care needs (Figure 1).
Most long-term care is provided as unpaid help from family and friends: four of five people who receive long-term care in the community rely exclusively on unpaid assistance (National Clearinghouse for LTC). When unpaid assistance is not enough or not available, then people with disabilities rely on paid individuals or companies to provide services. These services are expensive and can quickly exhaust lifetime savings. When that happens, the Medicaid and Medicare programs provide assistance.
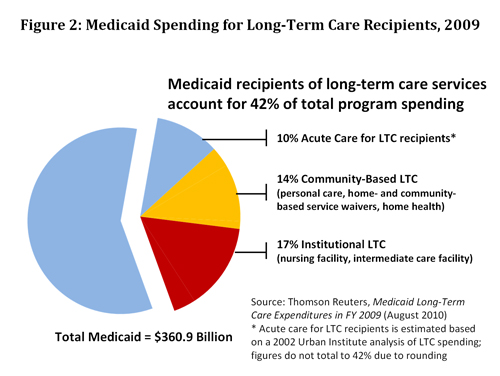
Medicaid pays the greatest share of total U.S. long-term care spending (40%), almost double the share paid by Medicare (23%) or individuals and families (22%) and more than three times that paid by private insurance (12%) (KCMU). In 2009, Medicaid spent $114.1 billion on long-term care services and supports, including $50 billion for community-based services and $63 billion for facility-based services. In addition, Medicaid spent approximately $38 billion on acute-care services for recipients of long-term care. Overall, Medicaid beneficiaries who receive long-term care services accounted for 42 percent of total Medicaid spending in 2009 (Figure 2).
Expanding Home- and Community-Based Services
Over the past three decades, states have been expanding Medicaid home- and community-based services (HCBS) in response to consumer preferences for alternatives to facility-based long-term care and, since 1999, in response to court-ordered mandates to serve people with disabilities in the least restrictive setting, taking into account the resources of the state. State Medicaid spending on HCBS programs has increased dramatically over the past 10 years, from 27 percent of total long-term care spending in 1999 to 44 percent in 2009 (Thomson Reuters). The shift toward HCBS also represents a budget strategy in most states to decrease Medicaid spending on higher-cost, facility-based services.
National health reform creates a number of opportunities for states to further expand access to HCBS programs. "I know, as a former governor," said Health and Human Services Secretary Kathleen Sebelius in a July 26 letter to governors, "that the federal government and states need to work side by side to deliver on the Affordable Care Act's promise of access to health care regardless of disability" and "provide greater opportunities for Americans with disabilities to live and work in their communities." The ACA creates new HCBS benefit options, higher income eligibility standards for these services, and federal financial incentives for states to further shift or "rebalance" long-term care budgets toward community-based settings. Major HCBS initiatives in the new law include:
- HCBS State Plan Option. Section 2402 (page 211) provides states with new flexibility to expand HCBS benefits and financial eligibility through a Medicaid state plan amendment instead of the more restrictive waiver process. However, this option includes new restrictions some states may find troubling. If a state creates an HCBS program using this option, it will automatically create an "entitlement" to that program and (unlike waiver programs) will be required to operate the program uniformly statewide without waiting lists. (There is more information about this option here.)
- Community First Choice Option. Section 2401 (page 206) allows states to provide HCBS attendant supports and services through a state plan amendment and receive a six percentage point increase in the Federal Medicaid Assistance Percentages (federal matching funds) for those services. This option also results in an entitlement that requires attendant services under the state plan to be offered uniformly statewide without waiting lists.
- Money Follows the Person Demonstration. Section 2403 (page 214) extends to 2016 the Money Follows the Person (MFP) rebalancing demonstration created through the Deficit Reduction Act of 2005. MFP provides states with enhanced federal matching funds for 12 months for each Medicaid beneficiary transitioned from an institution to the community during the demonstration period. (There is more information about this option here.)
- State Balancing Incentive Program. Section 10202 (page 845) provides enhanced federal matching payments to states to increase the proportion of Medicaid long-term care dollars that go toward HCBS. States that currently spend less than 50 percent of their Medicaid long-term care budget on HCBS are eligible to receive a two percentage point increase in federal matching funds on all HCBS programs, including waivers, mandatory home health benefits, optional personal care benefits, self-directed personal assistance services, and Programs of All-Inclusive Care for the Elderly (PACE). Eligibility for the enhanced match has not been determined, but will likely reflect HCBS spending reported here.
Changing the Culture of Residential Care
"States need to be careful not to focus too narrowly on just HCBS options," says Bonnie Kantor, executive director of the Pioneer Network. "Instead of focusing on the setting of care," she says, "the real goal is to create a culture of patient-centered care that creates a sense of home and community in every setting, including facility-based care."
This is particularly important for older adults, who are more likely than younger adults to receive facility-based long-term care: 22 percent of people age 65 and older who need long-term care reside in a facility, compared with only 4 percent of those under age 65, according to a Georgetown University analysis. Older adults' greater reliance on facility-based long-term care also is evident in Medicaid spending. Facility-based care accounts for 66 percent of Medicaid long-term care spending for older adults and people with physical disabilities, compared with 34 percent for people with intellectual and other developmental disabilities, who as a group are younger.
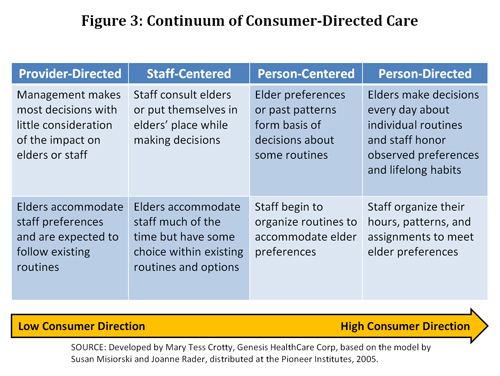
Consumers, patient advocates, providers, and policymakers are calling for "culture change" to improve long-term care. (See Ask the Expert for further description of the culture change movement.) The Pioneer Network, which focuses on culture change for seniors, was an early advocate of moving from provider-directed care toward consumer-directed care that preserves the dignity of individuals and enables them to make decisions about their daily routines (Figure 3). The provisions of the national health reform law described above promote culture change by seeking to integrate care around the person, increase workforce capacity, and improve the quality of care.
Culture change has begun to receive significant attention at the national and state levels. Philanthropic foundations, including The Commonwealth Fund, are funding programs to help foster culture change in nursing homes and other long-term care settings. At the federal level, the Centers for Medicare and Medicaid Services (CMS) has contracted with quality improvement organizations to train providers to engage in culture change efforts and sponsored several national meetings to bring the major stakeholders together. The Institute for Aging Services reports on these activities here.
Given that states are major players in financing and regulating long-term care, they have an important role to play in ensuring the quality of care and quality of life that people receive in nursing homes and other long-term care settings. Opportunities for states to improve long-term care services and support systems are described in the Ask the Expert column and Snapshots in this issue.