Today it is well known that social and environmental factors linked to poverty such as lack of housing, nutritious food, or transportation can be harmful to health. This awareness, combined with the shift from volume- to value-based health care provider payment, have prompted a growing number of health providers and insurance plans to take steps such as building supportive housing, opening “food pharmacies,” or offering case management services to help patients meet their nonmedical needs. In some cases, this has led to better health outcomes and lower health care costs.
The next challenge for health care organizations is figuring out which interventions work best, how to pay for them, and how to take them to scale. The Commonwealth Fund’s Program on Delivery System Reform has supported several efforts to learn how health care payers and providers can effectively and sustainably support approaches to addressing patients’ nonmedical needs. Here we highlight some of what we’ve learned so far.
Making the Business Case
While many health care organizations have launched efforts to address patients’ nonmedical needs, most investments have been modest and time-limited — in part because it has been difficult to show how offering such services can improve their bottom line. We supported development of two tools that can make social interventions a core part of health care organizations’ business models.
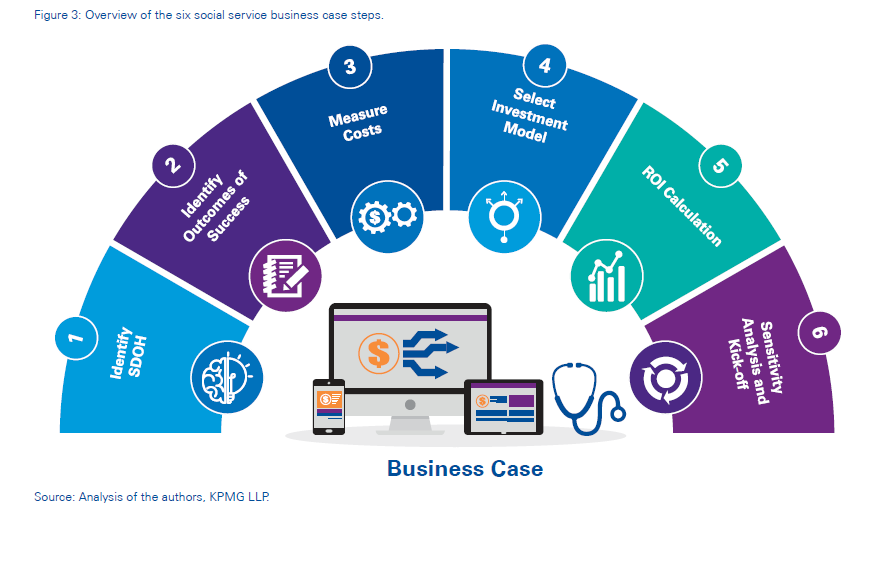
Researchers at KPMG’s Government Institute held expert interviews and conducted case studies of 10 health care organizations to create a step-by-step guide for making the business case for addressing patients’ nonmedical needs. It offers practical advice to help health care organizations identify patient populations in need, choose interventions, measure their potential impact on health outcomes and costs, gauge startup and fixed costs and potential savings, structure the investment (e.g., as a new program, benefit, or partnership), and calculate the projected returns.
One of the case examples describes the efforts of WellCare, a managed care plan serving 2.8 million Medicare, dually eligible, and Medicaid beneficiaries. Through its Community Impact Model, the plan makes small grants to community-based organizations, nonprofits, and social service providers to help them develop infrastructure to track the services they provide and gauge their impact. The plan also created a national call center to help members find social services. WellCare calculates that this effort saves $3.47 for every $1 invested.
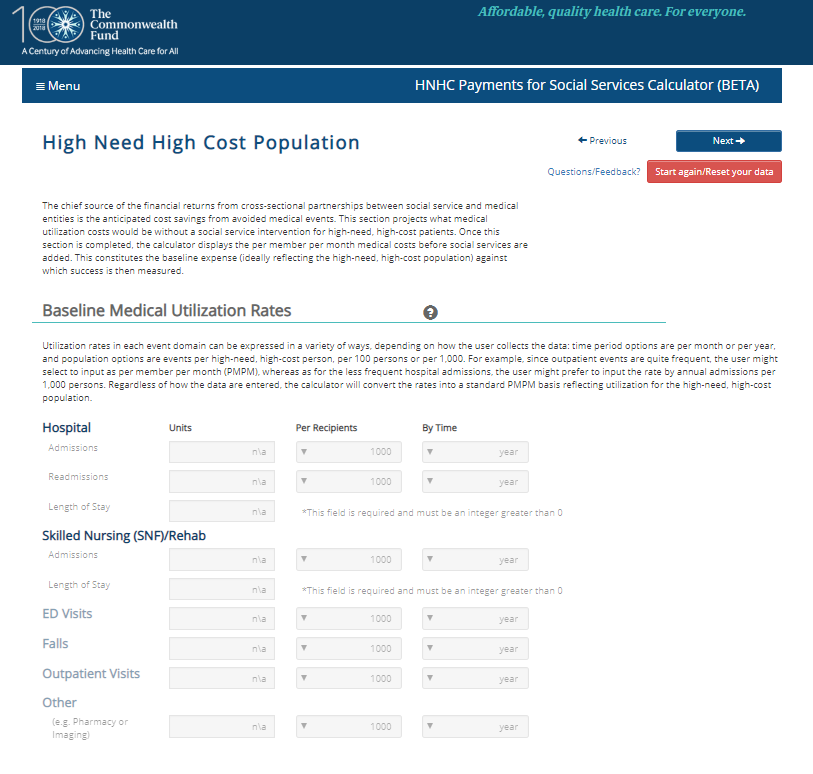
The second tool is the ROI Calculator, created by Victor Tabbush, professor emeritus of the UCLA Anderson School of Management. It is designed to help health care organizations and their community partners forge mutually beneficial financial arrangements to fund the delivery of nonmedical services. The tool calculates the return on investment (ROI) from such partnerships and shows how the financial returns and risks can be shared under a variety of payment arrangements (e.g., fee-for-service, capitation, or gainsharing).
Tapping Varied Funding Approaches
A Commonwealth Fund–supported brief by the Center for Health Care Strategies (CHCS) outlines the financing mechanisms state Medicaid programs can use to support health care providers’ efforts to integrate medical and social services. The authors note that pilot efforts can be funded through federal or private grants or use social impact financing (in which a state agrees to pay only for interventions that produce results). States also can set up trust funds or use Medicaid waivers to support new services.
For example, Minnesota’s Hennepin Health is a county‐based accountable care organization (ACO) that provides services to high‐need Medicaid beneficiaries. To pay for physical health, behavioral health, and social services (including permanent supportive housing and job supports), it uses a “braided” financing strategy, receiving a fixed per-member per-month payment for Medicaid health services and deploying funds from the human services department and grants to cover other costs. The ACO shares savings with participating providers and reinvests a portion in efforts such as hiring community health workers or assigning paramedics to a homeless shelter to avoid unnecessary emergency department visits.
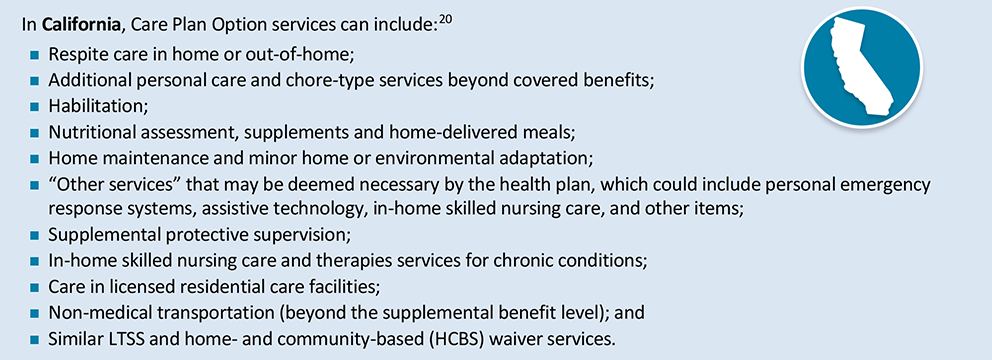
In another brief, CHCS researchers discuss how managed care plans can provide “value-added” services to help address the nonmedical needs of beneficiaries enrolled in both Medicare and Medicaid. While services such as housing, transportation, and nutritional supports are not part of Medicare or Medicaid’s benefit packages, some plans are betting that investing in them will lead to improved health and offset costs in other areas. Some states set specific rules on what value-added services plans can provide, while others leave it up to plans.
Forging Effective Cross-Sector Partnerships
In their efforts to address patients’ nonmedical needs, health care organizations have struggled to build partnerships with public health authorities, nonprofits, social service organizations, and local governments, given challenges in sharing data and forging formal working relationships. To help providers create successful partnerships, Ruben Amarasingham, former president and CEO of Parkland Clinical and Community Innovations, reviewed 300 cross-sector partnerships and identified the ingredients for success: close coordination, including referral tracking and help in making transitions; financial alignment among organizations around shared goals; and systems to promote transparency of data and results.
The Fund also supported Health Leads in creating a Social Needs Roadmap, a blueprint to guide health care organizations in launching partnerships that address patients’ social needs. The Social Needs Roadmap offers a library of tools, implementation guides, and best practices to help organizations at every step of integration — from selecting screening procedures to adapting workflows and garnering buy-in from administrators, providers, and others.
Building the Evidence Base
These and other initiatives are helping us understand how health care providers and plans can identify patients’ needs, beyond medical care, and connect them with services to help.
However, stronger evidence of the effectiveness of interventions themselves, complemented by convincing implementation and dissemination research, is needed to build a solid foundation on which to address patients’ holistic needs. UCSF’s Laura Gottlieb is leading a national effort to build SIREN (Social Interventions Research and Evaluation Network), a curated database of best practices and evidence of the effectiveness of social interventions and evaluation tools.
While much work still needs to be done, we offer these resources as a starting point to help health care organizations launch, improve, and scale efforts to address their patients’ nonmedical needs.


