Published July 24, 2020, in the Harvard Business Review. Reposted with permission.
Confusion reigns concerning the future course and consequences of the novel coronavirus pandemic in the United States. But one thing is certain: The health care system that emerges from the pandemic will not be the same. The question is, how will it be transformed? We attempt to answer that by posing alternative scenarios based on assumptions about key parameters that can heavily influence how the pandemic evolves. The analysis makes clear that in its pending stimulus package, Congress needs to take steps to prevent potentially long-lasting damage that COVID-19 may inflict on the health care system.
Three factors will prove most critical to the pandemic’s future: the public’s use of non-pharmaceutical interventions (NPIs) such as facial coverings and physical distancing; the availability, efficacy, and public acceptance of one or more vaccines; and the availability and efficacy of anti-viral therapies. There are obviously dozens of other possible influences on the course of the pandemic such as whether “herd immunity” might someday slow the spread. But these three factors have the greatest potential to decisively alter the course of COVID-19 in the United States and elsewhere if we succeed in instituting one or more of them.
To explore how the pandemic may evolve, we posit three scenarios with respect to these three factors:
- A dream case in which everything goes as well as could reasonably be expected.
- A catastrophic case in which everything goes badly.
- A middle case in which some things go well, but others don’t.
In evaluating the consequences of these scenarios for the nation’s health care system, we make one important additional assumption: The linchpin for a return to the health care system’s pre-pandemic “normal” state lies with the nation’s ability to assure the safety of segments of the population that are most vulnerable to the pandemic, especially the elderly and the chronically ill. These groups comprise the 5% of the population that consumes 50% of health care resources. Only when they feel safe to venture out will health care institutions experience a vigorous recovery in demand for their services. While telehealth can partially compensate for the falloff in the use of services, it will go only so far. It cannot replace hips or knees, do colonoscopies, or insert cardiac stents.
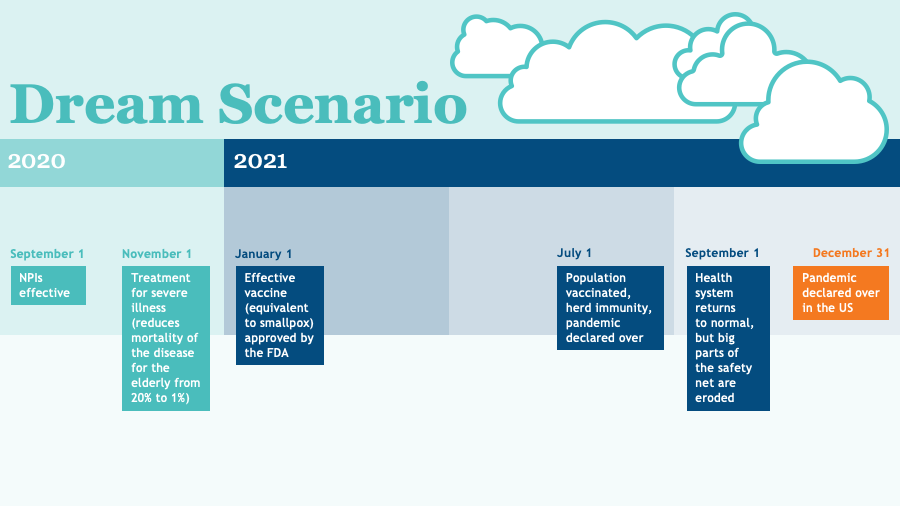
Scenario 1: The Dream Case
It plays out as follows:
- By September 1, governors and other political leaders have widely and aggressively implemented NPIs throughout the United States with strong public compliance.
- By November 1, highly effective anti-virals have reduced the mortality from COVID-19 among the elderly to the level of influenza: less than 1% of those infected.
- By January 1, at least one vaccine equivalent in efficacy to smallpox or measles is available for widespread use.
- By July 1, 60% of the American public is vaccinated, including most high-risk individuals, creating effective herd immunity.
- By December 1, 2021, the pandemic is declared over in the United States.
This highly optimistic scenario suggests that by early fall, viral transmission will be falling rapidly throughout the United States and that by late fall or early winter, it will be low enough for high-risk groups to feel safe. At that point, demand for health care services should begin to grow rapidly, accelerating with the arrival of effective therapies and a vaccine. Within 12 months, the health care system should be experiencing inpatient and outpatient volumes that equal or exceed pre-pandemic levels.
However, the health care system that returns to “normal” in 12 months will likely be different from the system of February 2020. A significant number of financially-weak hospitals and clinical practices will have closed their doors or merged with strong local institutions that have the capital to ride out the pandemic storm. There will be fewer primary care practices, community health centers, rural hospitals, independent small and moderate size hospitals, inner-city safety-net hospitals, and money-losing services of all types. Large systems will have grown larger and more dominant in local markets. The weak will be weaker and the strong stronger.
The market power of dominant local health care organizations may grant them even more leverage to negotiate higher prices from local payers in the future. Patients will have reduced choice of providers. The national capacity to offer effective primary care — the key to prevention and control of chronic illness — will be diminished, at least in the short term.
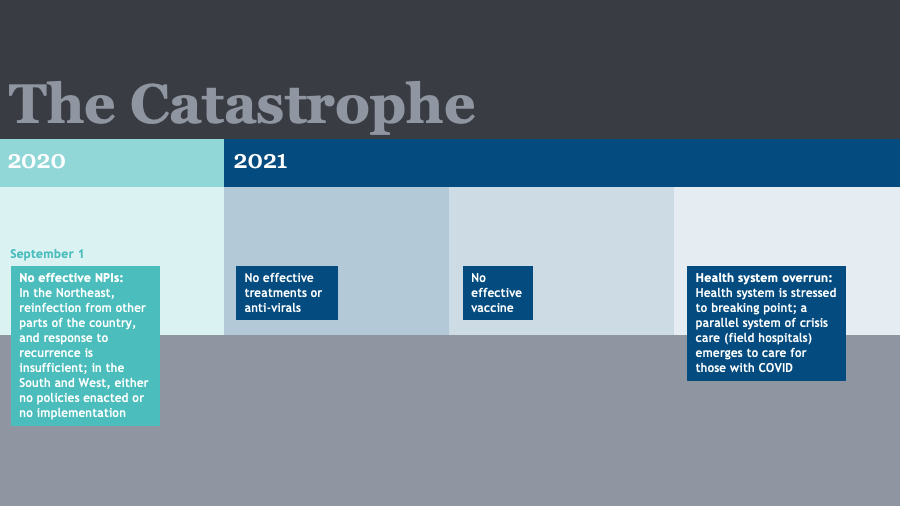
Scenario 2: The Catastrophe
Little works. What does isn’t implemented. The current failure to impose NPIs in the South and West persists, and even in areas like the Northeast, an exhausted populace balks at local shutdowns required to address outbreaks of novel coronavirus imported from elsewhere in the United States. No treatments more potent than Remdesivir and Dexamethasone materialize; nor does a vaccine that is safe and effective. The pandemic rages unchecked in current hotspots and reignites in the North and East. The U.S. health care system is overrun by COVID-19 cases to the exclusion of most other care. Field hospitals spring up everywhere. but demand still exceeds capacity. The United States steadily exhausts its supply of health care workers, personal protective equipment (PPE), testing supplies, and drugs. As the economy struggles, millions more Americans lose employment and their employer sponsored insurance. Population herd immunity proves illusory or far in the future.
This dismal picture suggests that demand for health care services other than COVID-19 care will remain at fractions of pre-pandemic levels for the foreseeable future. Compounding the reluctance of high-risk groups to visit health care facilities will be the swelling ranks of the uninsured. The result will be bankruptcy of large numbers of provider organizations and practices absent hundreds of billions of dollars of ongoing governmental support.
Such aid will constitute the creeping nationalization of the health care system. The failure of employer-sponsored insurance may create the national will for universal public insurance. The health care system that emerges after five years could resemble European models of public ownership and insurance more than the current largely-private enterprise.
Scenario 3: The Patchwork Middle
By September 1, half of states have effectively implemented NPIs, but adherence erodes over time in many areas because of partisanship, fatalism, or fatigue. An effective anti-viral regimen is available by January 1, which lowers mortality among high-risk groups to less than 1% among the healthy elderly and less than 10% among those with underlying conditions. An apparently safe vaccine is available on July 1, 2021, but it is only 60% effective in preventing infection and requires an annual booster. Because of its low efficacy and known side effects (equivalent to flu vaccine) or a lack of trust in the vaccine, only about 50% of Americans choose to get vaccinated over the following six months.
For the health care system, the implications are highly variable geographically. In areas with effective NPI regimens and high vaccination rates, viral transmission rates are very low by the end of 2021, but localized outbreaks are an ongoing threat. Vulnerable groups feel safe and gradually resume use of health care services starting in the fall of 2021, and by the spring of 2022, volumes of health care services have reached a steady state but are still 5% to 10% below pre-pandemic levels because of persisting sporadic viral transmission. Some local areas are tantalizingly close to achieving a localized dream scenario.
But in other locations, with poor NPI compliance and vaccination rates, the situation more closely resembles the catastrophic scenario. There, demand for services remains persistently low and provider bankruptcies and closures are widespread. For locations in-between, demand settles in at about 20% below pre-pandemic levels for the foreseeable future.
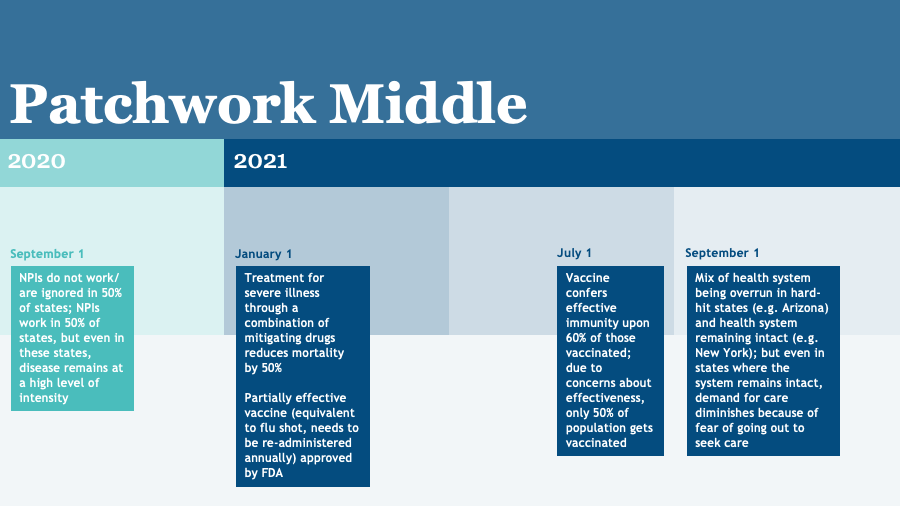
Overall the American health care system is significantly less capable than before the pandemic but is not as widely impaired as in the catastrophic scenario. In some areas, health care providers are heavily dependent on government aid and downsize dramatically to contain expenses; in other areas, the system is stable but consolidated with diminished primary care capacity, as in the Dream scenario.
The striking thing about these three scenarios is that under any of them, the U.S. health care system emerges very different from its pre-pandemic state and is hobbled in different ways. Even under the dream scenario, the loss of safety net institutions and increased inequities will require some type of government response. For advocates of European-style publicly-managed health care systems with universal coverage, the catastrophic scenario may offer the prospect of a more equitable and potentially more efficient system emerging from the ashes. However, the price of failing to control the pandemic in lives and treasure will be huge.
Under any likely future, the health care system will emerge from the pandemic less capable and smaller. The federal government can mitigate some adverse effects by supporting now — in its pending stimulus package — the critical services that are most at risk: primary care practices and safety-net institutions, including community health centers, critical access hospitals, and other providers in rural areas.
It can also confront the growing problem of non-competitive health care markets that will likely grow in number under almost any scenario. This would involve more aggressive enforcement of anti-trust authorities and/or the regulation of prices where competition has ceased to exist. For the catastrophic scenario, the government will have to plan massive investments to shore up the health care system on a scale never before contemplated in the United States.
When it comes to the future of a health system grappling with an unprecedented crisis, hoping for the best is not a strategy. It would be wise to act now to minimize long-term damage to the nation’s health care enterprise.