With the news that promising vaccines are close to approval comes hope that the COVID-19 pandemic will soon end. The federal government is working with states on the herculean task of distributing the vaccine safely and efficiently. Equally important is making sure people can receive the vaccine for free, regardless of their insurance status.
Thanks to the Affordable Care Act (ACA), most people with private insurance should have Centers for Disease Control and Prevention (CDC)–recommended vaccinations covered with no cost-sharing obligations. In March 2020, Congress enacted the Coronavirus Aid, Relief, and Economic Security (CARES) Act, which added to the ACA mandate by requiring insurers to cover a COVID-19 vaccine 15 days after the CDC’s Advisory Committee on Immunization Practices (ACIP) recommends its use. These requirements set a minimum standard; states may impose additional requirements on insurers.
Federal Rules Help Fill in Some Potential Coverage Gaps
In October, a federal regulation clarified several questions about the vaccine coverage mandate. The rule requires plans and insurers to cover the vaccine and its administration even when delivered by an out-of-network provider. Health plans will be required to reimburse these providers at a “reasonable” rate. Additionally, under the ACA, insurers must cover vaccines for “routine use.” These rules clarify that they must cover any COVID-19 vaccine recommended by ACIP, regardless of whether it has been designated for routine use. The requirements in this rule will last throughout the federal public health emergency period.
For the uninsured, the federal government has already advance purchased millions of COVID-19 vaccine doses. They will be free of charge to the providers who administer them. These providers must agree not to balance bill recipients, and they can be reimbursed for serving the uninsured through the CARES Act Provider Relief Fund (PRF). However, once the initial federal purchases and PRF funds are exhausted, Congress may need to provide additional funding to ensure that uninsured individuals can continue to obtain free vaccinations.
States Can Help Address Some Coverage Challenges
Most Americans with private insurance should be able to get immunized at no cost. However, there are potential gaps that could result in unexpected charges. First, the federal coverage requirement does not apply until 15 days after ACIP issues its recommendation. While ACIP will be under considerable pressure to review any Food and Drug Administration (FDA)–approved vaccines quickly, they are not required to do so. States can require insurers to cover COVID-19 vaccines upon FDA approval without waiting for ACIP to act, as Maine and Nevada have done.
Second, insurers may conduct their own assessments of vaccines produced by different manufacturers. It is possible that an insurer could decide to cover only the vaccines produced by one company, meaning that consumers who receive a different company’s vaccine would be uncovered. States could clarify that insurers must cover all FDA-approved COVID-19 vaccines during the emergency period. Third, the federal rules apply only to ACA-compliant health plans. Grandfathered plans, short-term plans, fixed-indemnity products, health care sharing ministries, and Farm Bureau plans are not required to cover vaccinations at all. States have the authority to mandate that they do so. Fourth, the federal requirement to cover vaccine administration by out-of-network providers only applies during the public health emergency, scheduled to expire on January 20, 2021. States may wish to extend this protection.
Lastly, the federal mandate for vaccine coverage hinges on the ACA, a law the Trump administration has been arguing is unconstitutional. Should the Supreme Court agree, among the many resulting harms would be the loss of guaranteed, free vaccine coverage for millions of Americans. States can enact these protections in state law, but they would not apply to self-funded employer plans, which cover over half of Americans under age 65.
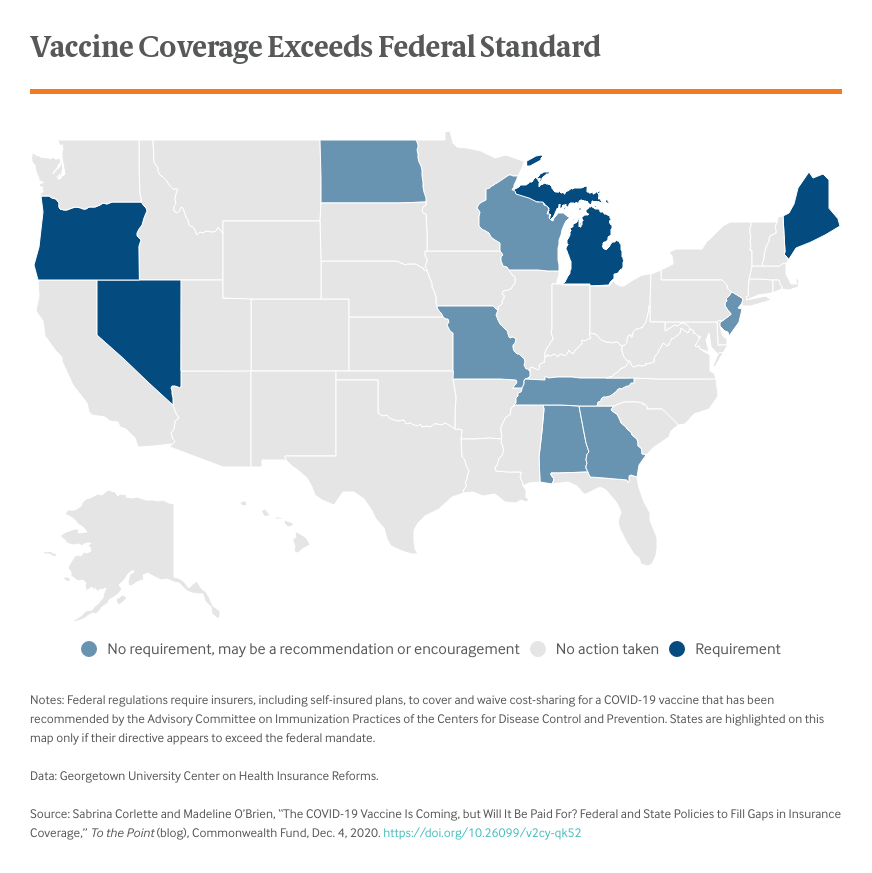
What Have States Done to Ensure Vaccine Coverage to Date?
Early in the pandemic, a number of states issued directives requiring coverage of COVID-19 testing and treatment. Several included a future COVID-19 vaccine.
For example, eight states (Kentucky, Louisiana, Maine, Maryland, Massachusetts, Nevada, New York, Rhode Island) and the District of Columbia required insurers to cover and waive cost-sharing for a future vaccine; seven states (Alabama, Georgia, Missouri, New Jersey, North Dakota, Tennessee, Wisconsin) issued guidance encouraging insurers to do so. Two states (Michigan and Oregon) announced they had negotiated an “agreement” with insurers to guarantee such coverage. As noted above, two states, Maine and Nevada, are requiring insurance coverage to begin immediately, without requiring that the vaccine first receive an ACIP recommendation. Most of the state directives, however, are consistent with federal requirements.
Looking Ahead
Vaccinating millions of Americans over a short period is a huge logistical operation, requiring massive coordination across federal, state, and local governments. These challenges will only be compounded if consumers fear they could face high, unexpected bills for the vaccine or its administration. Thanks primarily to the Affordable Care Act, federal law provides significant protection to millions of privately insured individuals. However, some consumers could fall through the cracks, and both federal and state officials will need to stand ready to help.