The American Rescue Plan (ARP), signed into law earlier this month, uses a large investment of government funds to boost public health and health systems to respond to the ongoing pandemic. In addition to specific funding for COVID-19 testing, treatment, and vaccine administration, the ARP includes new funding for Medicaid and resources for states to address some effects of the pandemic.
Extending Medicaid Coverage and Covering COVID-19 Testing, Treatment, and Vaccination
Medicaid is an important part of the national response to COVID-19. The program has helped alleviate health coverage concerns for many individuals losing their jobs and job-based health insurance. The ARP builds on earlier legislation that requires Medicaid to cover testing and ensures coverage of COVID-19 vaccination and treatment for beneficiaries. States will receive full federal funding for vaccine administration for one year after the public health emergency ends. Medicaid enrollees will have no cost-sharing responsibilities for COVID-19 testing, treatment, or vaccination.
Thirty-six states and D.C. have expanded their Medicaid eligibility to 138 percent of the federal poverty level (about $17,800 for an individual); two others have adopted but not yet implemented expansion. Currently, the federal government pays 90 percent of the cost for the expansion group. The ARP creates an incentive for the remaining 12 states to adopt expansion by providing an enhanced federal match for their existing Medicaid populations. Under the relief bill, states newly expanding their Medicaid eligibility would receive a 5 percent increase to their federal match for traditional Medicaid groups (e.g., children, individuals with disabilities, and older adults) for two years. This is on top of the 6.2 percent increase all states received under the Coronavirus Aid, Relief, and Economic Security (CARES) Act. For example, Alabama has a federal medical assistance percentage (FMAP) of almost 79 percent with the CARES Act increase. The FMAP in Alabama would increase to almost 84 percent if the state expanded Medicaid eligibility during the public health emergency.
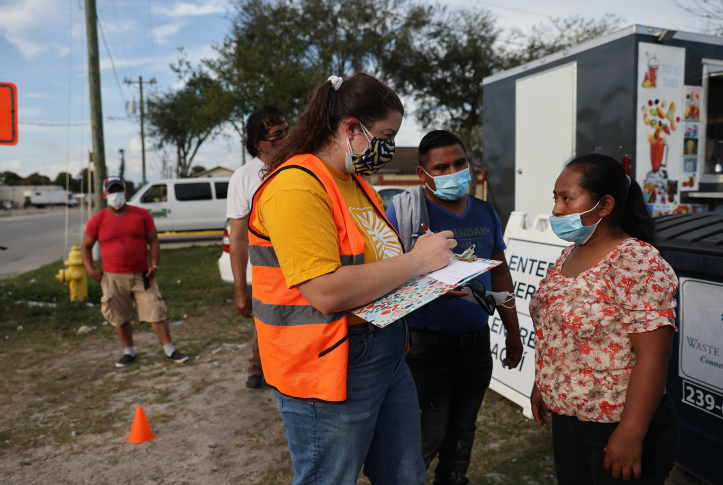
The first pandemic relief bill, Families First Coronavirus Response Act, gave states the option to cover COVID-19 testing for uninsured individuals through Medicaid. This means individuals who do not qualify for Medicaid and had no other source of affordable coverage, could receive a COVID-19 test at no cost. Less than half of states had taken up this option as of January 2021. The ARP adds coverage of vaccination and COVID-19 related treatment to cover uninsured individuals affected by the pandemic for the duration of the public health emergency. The addition of treatment coverage should make this a more appealing option for states.
Reducing Maternal Mortality
Prior to the pandemic, momentum had been building at the state and federal level to address the rise in maternal mortality. Blacks and American Indian/Alaska Natives (AI/AN) have the highest rates of maternal deaths in the U.S., as compared with other groups. Black, AI/AN, and Latinx people are also disproportionately impacted by the pandemic with higher rates of infection requiring hospitalization and death compared to whites. In addition to the coverage options discussed above, the ARP gives states the option to extend postpartum Medicaid coverage from 60 days to one year. The option is available for five years and could improve continuity of care and health outcomes at a time when having health insurance is more important than ever.
Supporting Long-Term Care and Behavioral Health
Early in the pandemic, nursing homes were primary epicenters for COVID-19 infections and deaths. Medicaid is the largest payer of nursing home care and other long-term services and supports. The pandemic has increased pressure on states to move people out of nursing homes if they can be cared for in less restrictive settings. The ARP includes a 10 percent increase in the federal match for home- and community-based services (HCBS) for one year. Funding could be used to provide personal protective equipment to home care workers, support workforce development to meet the growing demand for staff, or help states reduce the number of individuals on waiting lists to receive HCBS.
Many Americans are experiencing stress, anxiety, and sadness, partly driven by the economic challenges and social isolation. In a recent survey, Black and Latinx adults were more likely than white adults to report mental health concerns related to the pandemic. The ARP includes additional funding for a range of behavioral health services, including an option for states to develop and fund mobile crisis intervention services through Medicaid. Community-based mobile crisis teams can quickly respond to individuals experiencing a mental health or substance-use crisis in place of or alongside police. A behavioral health professional is required to be part of the response team. In addition, the team must have training in trauma-informed care and deescalation techniques.
Conclusion
Medicaid continues to be an essential tool for addressing the needs of vulnerable Americans. The ARP gives states new options for leveraging Medicaid to reduce potential spread of the virus, addresses health needs related to the pandemic, and boosts vaccination efforts. More steps are needed to ensure states take up the new options available to them and that individuals most at risk of hospitalization and death from COVID-19 are aware of their coverage options.