Background
It has been two years since the first COVID-19 vaccine was given to a patient in the United States. Since then, the U.S. has administered more than 655 million doses — 80 percent of the population has received at least one dose — with the cumulative effect of preventing more than 18 million additional hospitalizations and more than 3 million additional deaths. The swift development of the vaccine, emergency authorization to distribute widely, and rapid rollout have been instrumental in curbing hospitalization and death, while mitigating socioeconomic repercussions of the pandemic.
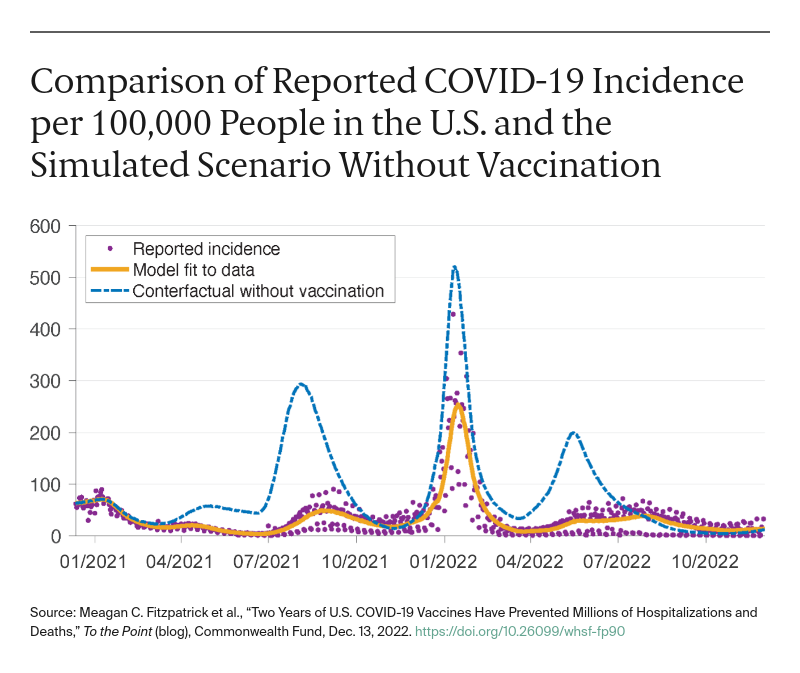
As more transmissible and immune-evasive variants have emerged over the past two years, the U.S. has responded by deploying additional doses and variant-specific boosters. The Omicron variants caused the largest wave of infections during the pandemic. COVID-19 monovalent vaccines available at the time were not as efficacious against the variant as bivalent boosters introduced later, but the wave would have been more devastating in the absence of vaccination.
As we mark the second anniversary of the U.S. COVID-19 vaccination campaign, understanding the impact of vaccines on reducing disease burden is needed to inform future, evidence-based actions. We therefore used a computer model of disease transmission to estimate hospitalizations and deaths averted through the end of November 2022. The model incorporates the age-stratified demographics, risk factors, and immunological dynamics of infection and vaccination. We simulated this model to compare the observed pandemic trajectory to a counterfactual scenario without a vaccination program. See “How We Conducted This Study” at the end of this post for further details on our methods.
Findings
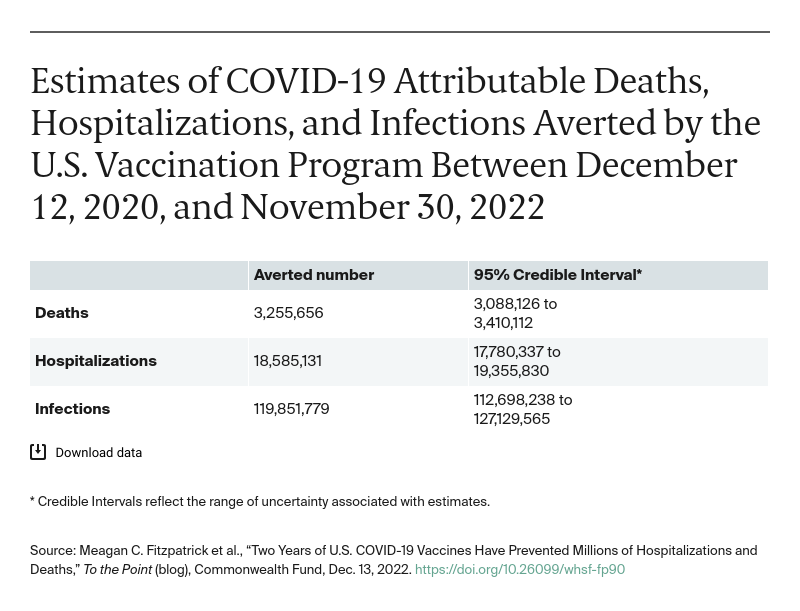
From December 2020 through November 2022, we estimate that the COVID-19 vaccination program in the U.S. prevented more than 18.5 million additional hospitalizations and 3.2 million additional deaths. Without vaccination, there would have been nearly 120 million more COVID-19 infections. The vaccination program also saved the U.S. $1.15 trillion (Credible Interval: $1.10 trillion–$1.19 trillion) (data not shown) in medical costs that would otherwise have been incurred.
Discussion
Our findings highlight the substantial impact of the U.S. vaccination program on reducing infections, hospitalizations, and deaths. Curbing hospitalization rates by reducing both COVID-19 incidence and symptom severity is particularly important amidst the strain on the health care system caused by unusually high levels of flu and RSV (respiratory syncytial virus). COVID-19 vaccination has preserved hospital resources for individuals who would otherwise have not received timely care.
Vaccination also has prevented many millions of COVID infections. Although the acute phase of these infections may not have required medical attention, each infection carries a risk of long COVID and debilitating symptoms. Many of the prevented infections would have been reinfections, which have higher risk of death compared to initial infections. In addition, as our previous analysis demonstrated, vaccines have kept children in school, highlighting the societal value of the ongoing vaccination program.
The estimated infections, hospitalizations, and deaths averted by vaccination are particularly striking when compared to the actual values observed during this time period. Since December 12, 2020, 82 million infections, 4.8 million hospitalizations, and 798,000 deaths have been reported in the U.S. In other words, without vaccination the U.S. would have experienced 1.5 times more infections, 3.8 times more hospitalizations, and 4.1 times more deaths. These losses would have been accompanied by more than $1 trillion in additional medical costs that were averted because of fewer infections, hospitalizations, and deaths.
The impact of the vaccination program is more remarkable given the challenges posed by the multiple variants that have arisen. The Omicron variants have been particularly immune-evasive and drove the largest surge in COVID-19 cases to date. However, the vaccines provided broader and more durable protection against severe clinical outcomes, including hospitalization and death. The reported “mild” nature of Omicron is in large part because of vaccine protection.
A limitation of our study is that we modeled only viral dynamics within the U.S. However, vaccines developed by the U.S. were also deployed around the world, changing the trajectory of the pandemic on a global scale. Without them, more variants could have emerged or there could have been greater importation of COVID-19 cases. In this regard, our study underestimates the true impact of COVID-19 vaccine development on U.S. outcomes.
The unprecedented pace at which vaccines were developed and deployed has saved many lives and allowed for safer easing of COVID-19 restrictions and reopening of businesses, schools, and other activities. This extraordinary achievement has been possible only through sustained funding and effective policymaking that ensured vaccines were available to all Americans. Moving forward, accelerating uptake of the new booster will be fundamental to averting future hospitalizations and deaths.




