Following the enactment of the sweeping drug pricing provisions included in the Inflation Reduction Act (IRA), lawmakers are again attempting to address high drug prices, this time by focusing on pharmacy benefit managers (PBMs) in a bipartisan fashion. PBMs are third-party intermediaries responsible for negotiating prescription drug price discounts with drug manufacturers and managing prescription drug benefits on behalf of payers. They have come under scrutiny in recent years for their role in high drug prices.
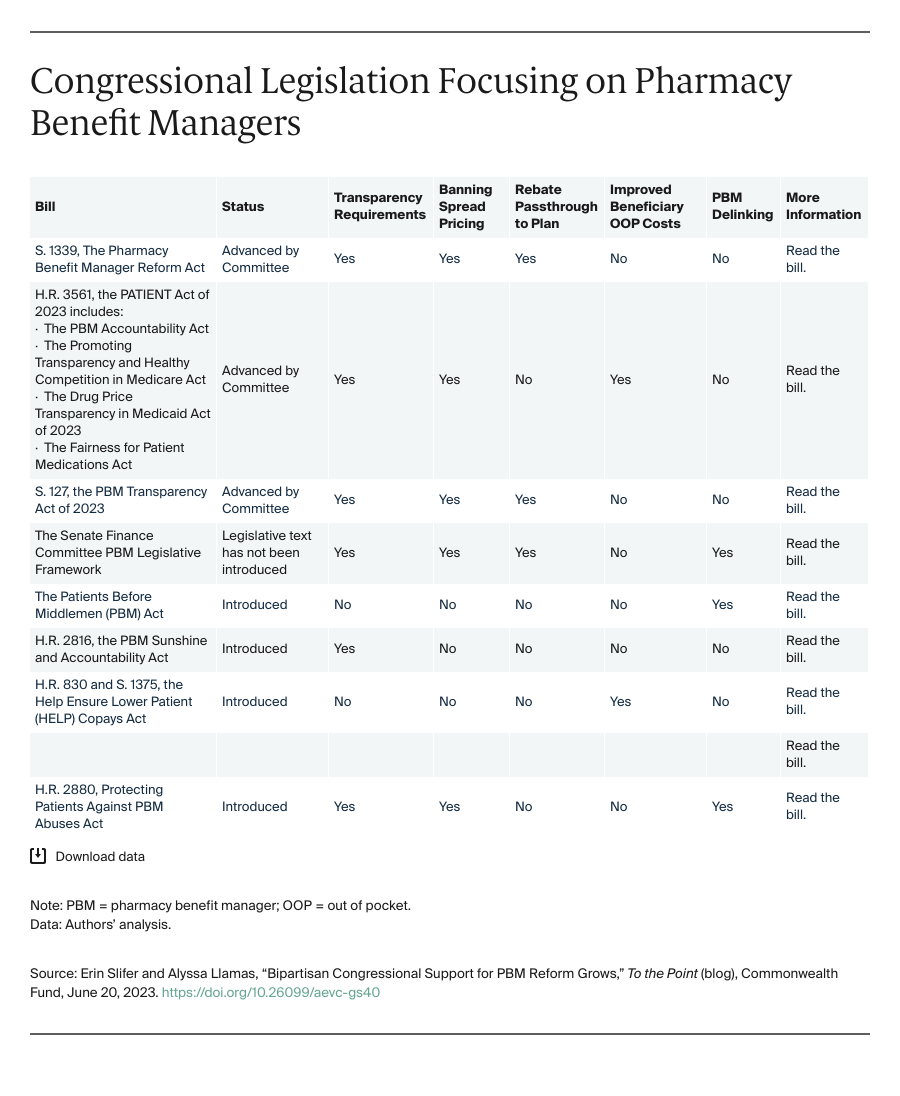
Congress has crafted several legislative packages that include reforms to increase transparency regarding the role of PBMs in the distribution chain for prescription drugs, overhaul how PBMs are compensated, and curb potentially anticompetitive behavior. In this blog post, we describe these legislative proposals.
Transparency Requirements. New reporting requirements to increase transparency could be the most easily accomplished provisions in the PBM overhaul, given ongoing interest from congressional Republicans and Democrats. Greater oversight would allow plan sponsors to make more informed decisions about contracts, which could lead to more competition between PBMs as well as lower prescription drug costs overall.
The Senate Health, Education, Labor, and Pensions (HELP) Committee and House Energy and Commerce (E&C) Committee unanimously approved bills that would establish reporting requirements for PBMs regarding their negotiations with pharmaceutical companies, drug price and rebate information, and formulary and benefit design. As part of a broader effort to address consolidation across the health care industry and concern about the growing trend of PBM-owned pharmacies, the E&C package also includes legislation to promote competition within the pharmacy market and insight into how PBMs reimburse PBM-owned pharmacies compared with other pharmacies.
Banning Spread Pricing. Lawmakers are also keen on ensuring that plans, employers, and patients are not overpaying for prescription drugs because of PBM tactics. Over the years, several states have taken actions to prohibit spread pricing in Medicaid managed care programs. This occurs when PBMs reimburse pharmacies less than what they are reimbursed by plans for a drug and retain the “spread” as profit, resulting in an overpayment by the plan. Lawmakers are considering proposals to extend the ban on spread pricing to all markets. The HELP-approved bill would prohibit spread pricing in employer-sponsored coverage and Affordable Care Act marketplace plans, while the E&C bill would ban spread pricing in Medicaid. The Protecting Patients Against PBM Abuses Act would also prohibit spread pricing in Medicare Part D plans.
Rebate Passthrough. PBMs negotiate rebates with drug manufacturers to lower the price plan sponsors pay for prescription drugs. PBMs then pass on a portion of the rebates to plan sponsors to reduce premiums and cost sharing and retain the difference as compensation. Some researchers assert this creates perverse incentives. It is also unclear how much of the rebate sponsors receive. The PBM Reform Act would require PBMs to pass on 100 percent of rebates, fees, alternative discounts, and other remuneration to plan sponsors.
Reducing Beneficiaries’ Out-of-Pocket Costs. Beneficiaries do not always benefit from the PBM-negotiated price (i.e., one that includes all rebates and discounts) because beneficiaries’ cost sharing is sometimes calculated as a portion of the drug’s list price, instead of the net price. The E&C package includes the Fairness for Patient Medications Act, which would cap monthly cost sharing and tie it to the negotiated net price, instead of the list price.
Additionally, the Help Ensure Lower Patient (HELP) Copays Act would prohibit PBM use of copayment accumulator programs, a practice in which PBMs exclude copayment assistance from accruing toward beneficiary cost-sharing obligations. The bill would instead require health plans to apply enrollees’ payments, including manufacturer coupons and assistance programs, toward cost-sharing requirements.
PBM Delinking. Lawmakers assert that high drug list prices translate into greater compensation for PBMs, which in turn creates added cost sharing for beneficiaries. The Protecting Patients Against PBM Abuses Act and the Patients Before Middlemen (PBM) Act aim to remove this incentive by prohibiting PBMs from earing a profit based on the Medicare Part D drug’s list price, and instead, limiting compensation to a flat dollar amount service fee. The PBM Act may be incorporated as part of a larger forthcoming Senate Finance Committee PBM package.
Conclusion. During the markups, lawmakers expressed more support for policies that were budget-neutral or generated savings, such as the transparency requirements and banning spread pricing. There is also the potential for a broader health care–focused package featuring PBM reform. For instance, the set of bills marked up by the E&C Committee features the reauthorization of several health care workforce programs that were approved alongside the PBM bills. Meanwhile, the Senate is considering taking up an insulin commercial cap bill that could feature PBM provisions.