Improving maternal health for Medicaid beneficiaries must involve comprehensive Medicaid managed care plans, which today enroll more than 70 percent of all beneficiaries nationwide. These plans not only pay for care but are also responsible for organizing and delivering care by establishing accessible provider networks, developing and applying coverage and treatment standards, ensuring health care accessibility and quality, and coordinating clinical care and social services. The contracts between Medicaid managed care organizations and states serve as blueprints and guide plan performance.
Developing these blueprints can be challenging for both states and plans. Their design can be influenced by the strength of the underlying health care system, the performance capabilities of the managed care industry, and states’ own policy priorities. State contracts differ in terms of issues addressed, the specificity of priorities, and the amount of autonomy granted to plans to make coverage and care decisions.
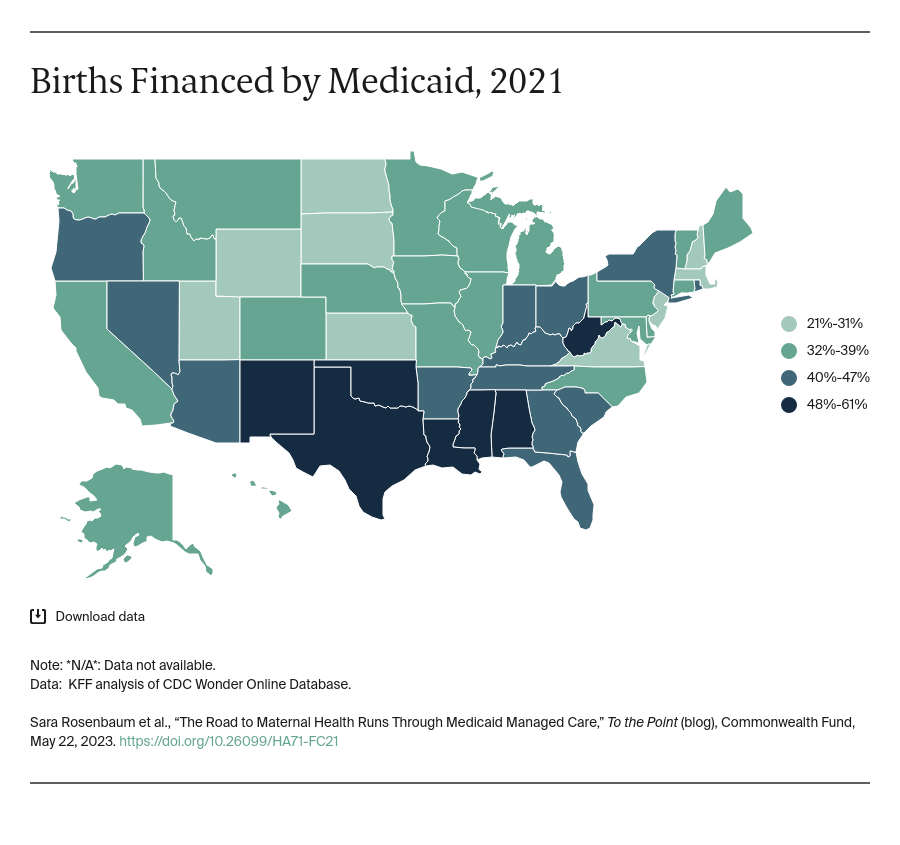
To better understand the relationship between managed care performance and maternal health, we analyzed Medicaid contracts from all states that used comprehensive managed care in 2022 (39 states and the District of Columbia). We conducted an extensive review of maternal health "best practices" from pre-pregnancy through postpartum to develop a contractual review instrument. Key findings from our contractual review are captured in tables that summarize our results and include the detailed contract language.
The following themes emerged during our review:
Contracts tend to approach the maternal health continuum in a fragmented and incomplete way.
Our single most important finding concerns how the contracts address the maternal health care continuum. Although maternity care is a core element of all agreements, we found that the contracts take a fragmented approach to maternal health rather than framing plan performance along the full continuum. Individual services (e.g., family planning, prenatal care, delivery) are described, but overall, the contracts lack a holistic approach that expresses plan performance as occurring along a continuous trajectory.
Contracts reflect variation among states in how key aspects of maternal health care are addressed.
Within this fragmented approach, there is notable variation across states in whether services are addressed at all as well as if they are available throughout the continuum of maternal health care. For example, six states address early entry into care, seven states explicitly require networks to include specialists in maternal and fetal medicine, nine states specify doula services, six states address maternal oral health, and eight states address lactation support. Among the 40 contracts, 29 expressly identify mental health and substance use disorder services as part of maternal health care, 29 specifically address maternal care access as an element of overall access considerations, and eight address transportation to some degree. Payment reforms to improve maternal health care performance are an element of 18 contracts. Additionally, the contracts show wide variation in their degree of specificity and precisely what services are available throughout the entire maternal health cycle as opposed to only at distinct times — that is, a service is explicitly available during pregnancy, but there is no information regarding availability during the postpartum period. Contracts also show how states defer to plans regarding adherence to evidence-based standards. In a clear example of the latitude states give plans, California permits its contractors to devise their own risk-assessment tools comparable to the state’s long-established and highly-regarded Comprehensive Perinatal Services Program.
Recommendations for Plans, States, and the Centers for Medicare and Medicaid Services
Strengthening managed care and maternal health begins by reinforcing the underlying contracts, which serve as the blueprints for measuring performance. This includes developing comprehensive maternal health care treatment guidelines that span the full continuum of care and guide state purchasing expectations and plan performance. Today, various professional societies produce guidelines on specific aspects of maternal health care, but we lack fully integrated guidelines for purchasers and plans spanning all the services and disciplines involved in maternal health care improvement. Developing a fully integrated maternal health care guideline can make use of the vast literature on the services that make a difference to maternal health.
The Centers for Medicare and Medicaid Services (CMS) and states could use these guidelines to develop new Medicaid demonstrations to help states align their contracting practices with comprehensive guidelines to expand coverage and care. There is precedent for this strategy. CMS did this with Medicaid 1115 substance-use disorder demonstrations, where approval is tied to state adoption of American Society of Addiction Medicine treatment guidelines.
Finally, CMS, states, and plans, working with providers, consumers, and experts, could develop a best practices initiative that shares innovative approaches to managed care and maternal health to ensure access to the full maternal health continuum.
With these changes, managed care can become part of the solution to the maternal health crisis.