Community health centers are often the first line of defense during health crises in America, including the opioid and HIV epidemics. More than 13,000 service sites operate as a safety net for 30 million patients who would otherwise struggle to access primary care, including 13 million patients living in poverty, 6 million uninsured patients, and 1 million patients experiencing homelessness.
Despite their vital role, health centers are in a precarious financial position. They rely heavily on Medicaid reimbursements, which are lower than Medicare and commercial health insurance reimbursements, and federal grant funds. Operating within tight financial margins leaves them with little room for investments in technology, staffing, and other resources; when financial uncertainty grows, health centers often impose hiring freezes or reduce services.
The COVID-19 pandemic exacerbated these challenges while creating new ones. Centers provide COVID tests and treatments while continuing access to their standard services, all in a safe environment. Further, patients are disproportionately from racial or ethnic minority groups, who are more likely to get seriously ill and die from COVID-19. In response, some health centers expanded outreach to ensure everyone could receive lifesaving care.
Federal and state policymakers supported centers through targeted funding and policy changes that promoted building capacity, improving technology, and maintaining revenues. To understand how these supports affected health centers, we analyzed responses from the 183 U.S. primary care physicians who reported working in a community health center in our Commonwealth Fund 2022 International Health Policy Survey of Primary Care Physicians.
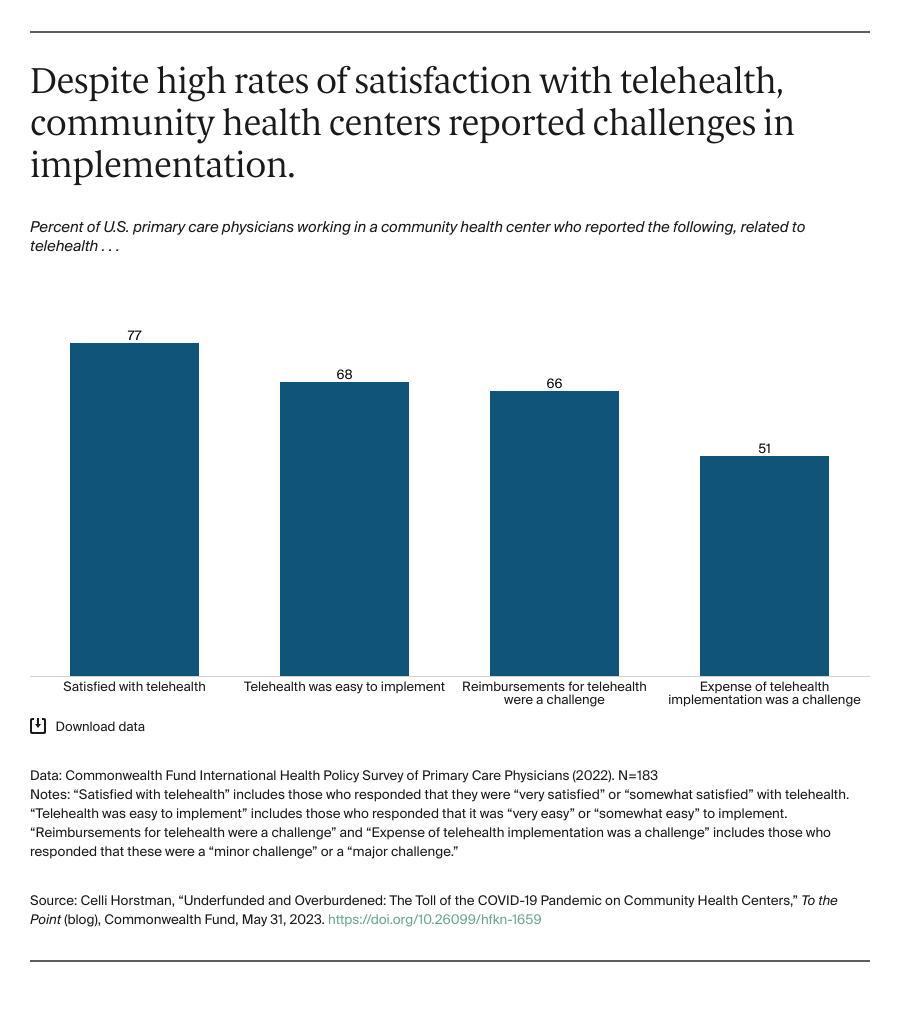
With Surge in Telehealth Use, Reimbursements and Expenses Were Challenging
Before the pandemic, telehealth use among community health centers was limited, owing to insufficient reimbursements and limited capital to purchase and maintain equipment. In an effort to maintain care, centers rapidly implemented telehealth, with the assistance of health center–specific funding and reimbursement policy changes. In the first year of the pandemic, the number of centers providing clinical services via telehealth more than doubled, increasing from 43 percent of centers providing these services in 2019 to 99 percent in 2020.
While most physicians working in community health centers reported they were satisfied with telehealth and found it easy to use, the majority said that reimbursements for the services and related expenses, either to implement or maintain telehealth platforms, were challenges.