High deductibles and cost sharing are making health care unaffordable for many, even with insurance coverage. About half of working adults with employer, marketplace, and Medicaid coverage say they struggle to afford health care. According to recent estimates, almost 100 million people, or 41 percent of adults, have debt because of medical or dental bills. Medical debt creates significant financial burden for many low-income Americans, depleting their savings and forcing them to forgo basic necessities. About 460,000 bankruptcies every year can be attributed to medical debt. The burden of medical debt is borne disproportionately by Black Americans, people with disabilities, and low-income adults.
Some States Require Hospitals to Provide Financial Assistance to Low-Income Patients
The federal government and states have a patchwork of laws in place that are intended to protect enrollees from medical debt and its negative effects, but these protections vary significantly by state and have significant gaps. Requiring hospitals to provide financial assistance to certain eligible populations can help prevent patients from incurring debt.
Federal law requires nonprofit hospitals to have a written financial assistance policy in place and to “widely publicize” the policy. However, it does not set any minimum eligibility standards or requirements for how much financial assistance should be provided. Nineteen states and the District of Columbia fill the gaps in federal law by setting standards for the provision of financial assistance. Some states require hospitals to provide an unspecified amount of financial assistance to people with incomes under a specific threshold (for example, under 100% of the federal poverty level or FPL in Florida and under 400% FPL in California), while others require hospitals to provide free care for people with incomes below certain thresholds (for example, under 150% FPL in Maine and under 250% FPL in Vermont).
Requirements to Provide Financial Assistance Can Be Made More Effective by Also Removing Application Barriers
Simply requiring hospitals to provide financial assistance can be insufficient because it places the onus on patients to find out about the assistance and apply for it. Federal law and many states have long required hospitals to inform patients about their financial assistance policies, including by posting in a public place or online and providing information in billing statements. Simply relying on such notification requirements can be insufficient because patients are often focused on more pressing health care needs and can easily overlook signs and forms.
One report by a Maryland state agency analyzing data from 2017 to 2018 found that hospitals had classified 60 percent of bills that should have been eligible for free care under state law as “bad debt” and had attempted to collect from many of these patients. In 2020, Maryland began requiring hospitals to consider patients already enrolled in other need-based programs for low-income residents as “presumptively eligible” for free care. This means they would become automatically eligible for free care without having to apply for it. Illinois has had a similar fast-track procedure in place since 2014 to help patients qualify for financial assistance.
A few other states have followed suit and passed laws to institute stricter requirements for screening and to remove barriers related to the application process. In 2023, Oregon enacted a bill requiring nonprofit hospitals to screen patients for presumptive eligibility for financial assistance if they are uninsured or owe more than $500. Under the law, hospitals are required to conduct the screening and apply any applicable financial assistance before sending a bill to the patient.
While it does not explicitly require hospitals to screen patients for financial assistance, Minnesota’s new law enacted in 2023 requires hospitals to schedule uninsured patients or patients whose insurance status is unknown for an appointment with a certified application counselor who can make the application process easier to navigate.
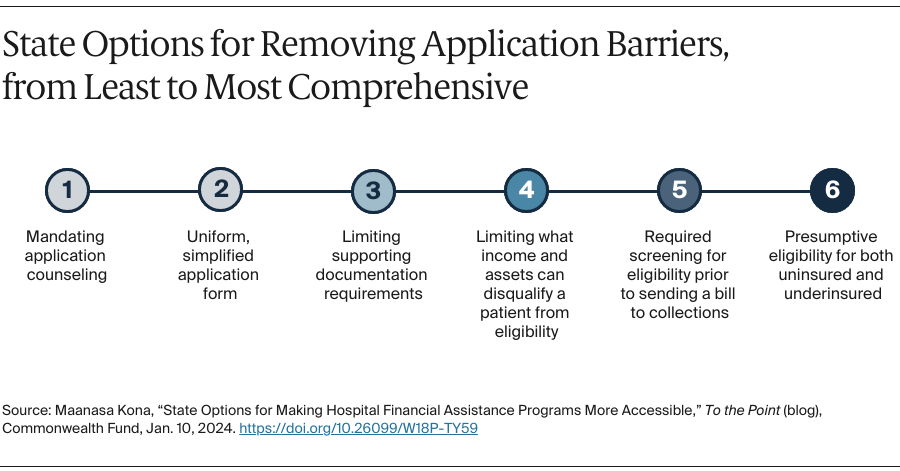
To improve access to financial assistance for applicants, Washington State now prohibits hospitals from considering certain types of assets in making an eligibility determination or placing an “unreasonable burden” on patients applying for assistance, including the kinds of documentation hospitals can ask patients to submit. At least five states require hospitals to use a state-developed uniform application form, which can make it easier for community-based organizations to assist patients. States have several options for making financial assistance accessible, ranging from less comprehensive options such as mandating application counseling or use of a uniform application form, to more comprehensive options such as establishing presumptive eligibility fast-track processes.