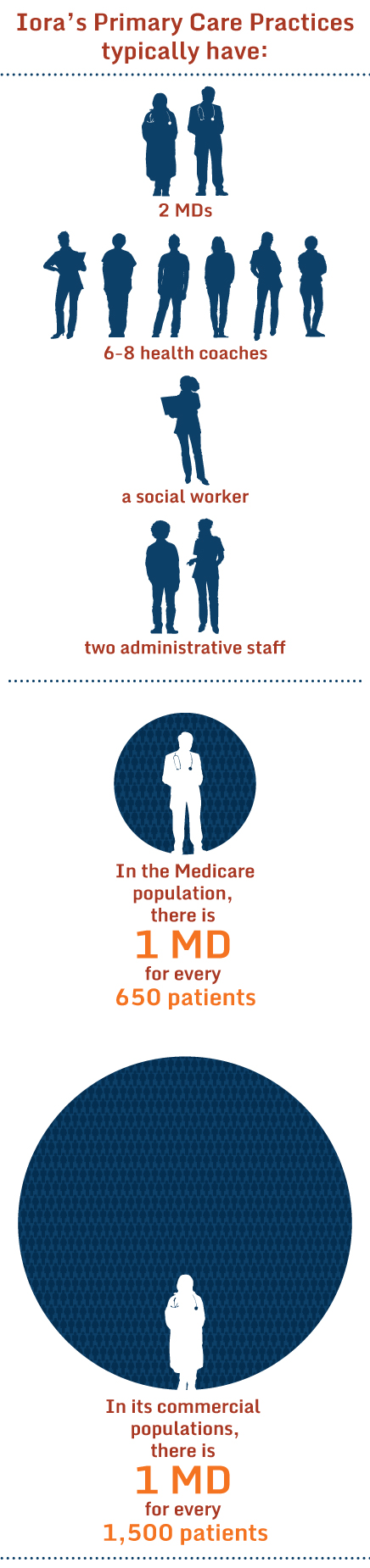
Primary care physician Rushika Fernandopulle, M.D., M.P.P., founded Boston, Massachusetts–based Iora Health in 2010 with the goal of rebuilding primary care from the ground up—using health care teams that include an abundance of health coaches (Iora’s term for community health workers) to provide practical and emotional support to patients. Iora customizes its care model to the needs of particular patient populations, including freelancers, casino workers, carpenter union members, health system employees, and Medicare beneficiaries. To enable this approach, Iora works with self-insured purchasers and health plans and accepts global payments. It now has a network of 29 practices and is set to open about 20 more in the coming year.
Q: Iora Health’s primary care teams are configured very differently than those in other practices—with far more health coaches than nurses. What’s the rationale for that?
A: The health coaches are what make our business model work. We have structured Iora Health completely as a value-based provider. We do no fee-for-service billing. As we see it, our job is not to see one patient at a time and do the best we can and bill for that. Instead we need to figure out how to improve the health of a population of patients and keep them out of trouble.
You really need health coaches to do that. They are the ones who help patients with all the blocking and tackling to execute the treatment plan. They help patients understand it. They will hold your hand when that is the right thing to do, and kick you in your behind when that is the right thing to do, help you navigate the system when that is the right thing to do.
Q: You’re ramping up your hiring of health coaches as you expand your practices across 11 states. How do you go about finding the right people for the job?
A: We want people who have minimal social distance from the people they serve—ideally they live in the community. We also look for empathy, that they are willing to learn, and that they work well in teams. We don’t care what they did before. Some of them do come from health care. That doesn’t disqualify you but it doesn’t qualify you, either. Some of our health coaches worked at Dunkin Donuts, and Target and Sears or Teach for America. They’ve worked on the buffet line at a casino. We’ve found the way not to pick them is to look at their resume, which is what everyone else does. You have to meet them. We do a form of speed dating. We bring in lots of people. They meet a lot of our folks and we look for those who are able to connect with different sorts of people.
Q: You’ve said before that health coaches are not low-cost substitutes for other providers, but how much do they make?
A: The salary varies dramatically depending on the geography and what other jobs people are coming from, but in general it’s close to the starting salary for a teacher. We say we’re not trying to make you poor or make you rich. We try to pay fairly and we give full benefits. We also have a career ladder: health coach, senior health coach, and after that health coach trainer. We pay for people to get further education if that is what they want. The whole idea is to turn it into a real career as opposed to a dead-end job.
All that said, health coaches are much cheaper for us than hiring nurses or doctors, and much easier to find. There are many, many more potential candidates. But that's not why we hire them. It’s because they can actually do the job better than a doctor or a nurse.
Q: Can you give us a sense of what they do day by day—what makes them different than the other members of the team?
A: Health coaches are very involved in office visits. When patients come in they first meet with the health coach who tees up the issues, finds out how things are going, what agenda the patient has, then they get the doctor. The health coaches will stay in the room while the doctor is there and their role is first to be the patient’s advocate and second to be a scribe. So they actually write up the notes while I can make eye contact with the patient. When I leave, the health coach stays and closes the loop using the teach back approach and talks about challenges the patient is going to face. They say things like, “O.K. you are going to exercise. When are you going to exercise? How are we going to make sure you do that? What are the barriers? What can we do to avoid them?” and so on.
The doctor’s involvement during visits could vary from 10 seconds if the patient is doing great—I walk in and say, “Hey, I hear you are doing great. Keep up the good work. I’ll see you next time.”—to an hour of doctor time if it is a really complicated case or a new patient.
Q: We have also heard that at the outset of the visit, the health coach meets with patients when they are fully dressed, sitting in a comfortable setting outside of the exam room. Why is that important?
A: Health care services have been turned into transactions: you document for billing and everyone’s job is to make the transaction as efficient as possible. So we have patients disrobe before the doctor arrives to save time. That is hokum: transactions have never healed anyone. The thing that heals is relationships. We focus on how to build a relationship with patients. That means putting them on equal footing and making them feel comfortable.
Q: So what are the health coaches doing outside of the office visit?
A: About half of a health coach’s time is spent outside of traditional visits. A lot of times it is emailing, texting, or video chatting with patients. They meet patients at least once in person but after that a lot of the checking in can be done virtually. It’s 2015. Why not, for God’s sake? They also go to people’s homes. They can evaluate how the patient is doing, whether their home is safe, if they have food. A lot of times the health coach goes to the grocery store with the patient. They encourage the patient to shop for everything they usually would, and then they’ll look in the cart and help the patient figure out why some of it is a bad idea and what possible substitutes are. Taking patients for walks is something else they do. It’s a really good way to talk about and model exercise behavior.
Q: As health coaches take on these roles, do you have any concern about patient safety or the accuracy of information they provide?
A: We invest in training quite a bit and the role they play varies by how experienced they are. So at the beginning a doctor will do a good part of closing the loop and the health coach will listen. And then when they are ready the health coach will do it and the doctor will stay and make sure it is right, then eventually the doctor can just walk out the door because you know they can do it because they’ve done it so many times. We have 30 or 40 different competencies they need to demonstrate. But what makes me feel better is they are doing it in front of our faces. This is why the integrated model is so much better—there are a lot of CHW models that are good, but the CHWs are free-floating out there in the community and not working as closely with the doctors. I overhear the health coaches when they are calling patients. They are in the huddle room sitting next to me.
Q: Can you give us a flavor of some of the competencies they must demonstrate?
A: They vary from the mundane such as how to take a blood pressure to something such as sitting with someone when they get bad news, which is much more touchy.
Q: You also use group visits, or clubs, for diabetes, for instance. What role do the health coaches play in running them?
A: Each coach will run at least one club, based on their particular interest. It really varies completely by the population we are serving. One of the things we’ve learned is that yoga is really helpful for stretching and meditation and mindfulness, and so with the Freelancers Union in New York, health coaches ran a yoga club. For our carpenters, if we run a yoga class, they don’t come. So one of the health coaches said we are not going to call it yoga we are going to have hammer time. They are doing yoga and holding tools in their hands. We have health coaches who teach tai chi, do walking groups, Zumba—all sorts of things.
Q: Can you give us an example of how the health coaches have made a difference in terms of health outcomes?
A: Sure. We had a Medicare patient in Seattle. She had moved from California after her husband died to live with her daughter. The problem was the daughter lived in the suburbs and the mom couldn’t get around and was getting isolated. Her diabetes and hypertension were getting worse. The health coach realized that the problem wasn’t that she needed more medicine; she needed to stop being isolated. So the health coach essentially taught her to use the bus, first by riding to the clinic together. The patient figured out how to do transfers and ride the bus back. Now this has nothing to do with health care and yet it has everything to do with health care. Now she can come to us, she can visit friends. And by the way her diabetes and blood pressure are in great control. We didn’t touch her medicine.
Q: It sounds like coaches are allowed some creativity in coming up with approaches.
A. Yes. People often ask us, “What are your protocols?” I always go back to the quote from Tolstoy that happy families are all alike and each unhappy family is unhappy in its own way. Patients are unique when it comes to their problems and they require very different approaches. Frankly, we as health care professionals are not smart enough to create protocols that work with this level of variation. Our view is to hire smart, creative people who are empathetic and let them figure out what patients need in order to fix the problem. Then let them do it. Don’t tell them what to do. It is a very heretical and different sort of culture.
Q: Do they have some discretionary spending if they see a need?
A: Absolutely. They have a small budget, which they can spend on patients if they think it would make a difference. We had a patient in Hanover, New Hampshire, who was not very engaged in her care. Her diabetes was out of control. The health coach noticed her toes were painted and remarked on it. The patient said, “I can’t afford to go to the spa anymore and I can’t reach and do it myself.” The health coach offered to paint her nails. She also pointed out that if she didn’t take care of her diabetes, she might lose her feet, which got her attention. The patient started asking what she could do to prevent it. So while she was painting her nails, the health coach taught her how to monitor and maintain her blood sugar. All of a sudden, she is engaged. It took a $2.99 bottle of nail polish and her diabetes is under control. The budget for these things is about $1,000 per practice per year.

Iora Primary Care health coach Brendalys Rosario takes senior Marina Haley on a tour of the new Iora practice in Hyde Park, Mass.
Q: We’re interested in some of the challenges you’ve encountered in integrating health coaches into care teams. You are bringing in people in who may have no background in health care and who are working with people who have advanced degrees. Do the typical hierarchies come into play and how do you manage that?
A: It could be an issue, and that’s exactly why we are starting from scratch. When we hire people, like doctors, we say this is how we work and if you don’t like it, you can go elsewhere. We’re also willing to fire people over this issue. And we have lots of cultural things that flatten the hierarchy such as the daily huddle. We all take turns running it. So the doctor gets to run it one out of 12 days. So does the health coach, so does the operations assistant. So does the social worker. Our concept is that the health coaches work for the patient and they are the closest to them. The doctor works for the health coaches—not the other way around. They drive the culture.
Q: How do patients react to the altered hierarchy? Don’t they prefer to interact with the doctor?
A: Often patients are a little skeptical. Who is this person? Why is he or she there? It’s key to have the patient meet the health coach the first time with the doctor’s arm around them. So you take this doctor magic that patients imbue in us and you transfer it to the health coach. I tell the patients the health coaches work closely with me and I say, when you tell her, you tell me. I also point out she is nicer than me and she is easier to get a hold of. And so that works. I think we are very quickly able to convince almost every patient that the health coach adds value.
Q: Despite their potential benefit, health coaches or community health workers have not been widely used within health care organizations. What might it take to spread the approach? Why isn’t it catching on?
A: The obvious elephant in the room is the payment model. No one pays for health coach visits let alone health coach phone calls or huddles. We also have these things we call cuddles where the health coach and the doctor will talk about their common patients together, and wuddles, which are weekly meetings where we try to identify common problems and new approaches to addressing them. The only way we can afford to do this is because we’re getting paid on a population basis.