
In Corona Question Corner (CQC), the Commonwealth Fund’s Eric Schneider, M.D., will answer our more personal questions about coronavirus using his own knowledge of medicine, health care research, and analogies ranging from baseball to bad television. Also, with levity and hope. Have a question for Dr. Schneider? You can submit to [email protected] and, if selected, he will publish and answer (to the best of his ability) your question without disclosing your name or affiliation. We’re all in this together. Please wash your hands before proceeding.
FINE PRINT DISCLAIMER: The opinions expressed here are not official policy of the Commonwealth Fund. They are not a substitute for medical advice from a health professional, directives from government or public health authorities, or your own good judgment.
Protests in June, bump in cases... when?
If COVID is dispatched by sunshine, why are cases climbing?
Super spreaders, R0, and kappa walk into a pool
Contact tracing and American values?
Case counts are declining - is it time to travel?
COVID-19, disparities data, and structural racism
Why do African Americans have higher case and death rates from COVID-19?
Can a garment steamer kill coronavirus on my mask?
Can I lunch with friends without ending up on COVID's menu?
We can protect monkeys from coronavirus?! What about me?
Clearing up the confusion on testing
Will next year's flu season be much worse?
Can mosquitoes carry the coronavirus?
How can it be than my symptoms are more likely the result of a cold virus than the coronavirus?
What is happening with mutation?
Why aren’t we doing more to identify infected people?
Are there different distances that should be adhered to depending on the situation?
Any idea how long COVID-19 germs live in the refrigerator?
What drugs seem to be helpful for treating patients so far?
My roommate just got sick. Now what?
Why does the disease seem to be affecting different demographics in different countries?
Once you recover from coronavirus are you immune?
What really is “herd immunity”?
We were exposed to a person with COVID-19. What should we do?
How long can the virus live on surfaces?
Once a person has a positive test for COVID-19, how long are they a risk to infect others?
Why have we not seen a significant bump in new COVID-19 cases from protests that occurred in early June?
As of July 29, 2020.
After so many days of isolating inside and being warned by officials about the dangers of crowding, it seemed unthinkably risky to join thousands of people protesting the needless deaths of George Floyd, Breonna Taylor, Ahmaud Arbery, and others. Many states and cities were just beginning to reopen under controlled conditions. Of course, others had reopened businesses even earlier. The images of massive protests several weeks ago with people in close contact, without masks, and running through tear gas sent shudders through public health officials. And the protests were happening in communities most afflicted by the coronavirus. After months of shutdowns finally brought the pandemic under control in New York City, it seemed inevitable cases would soon surge again.
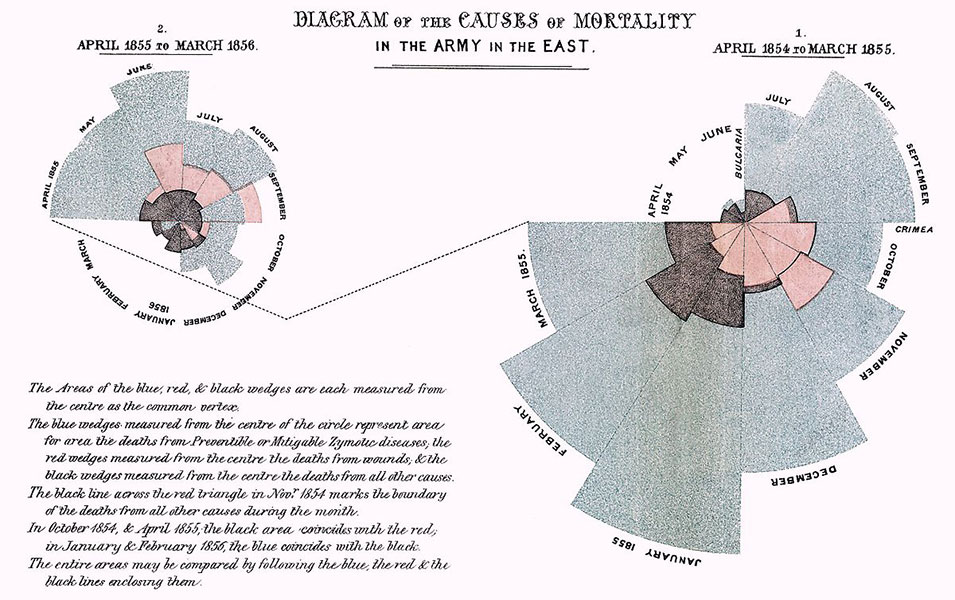
But as scientists know, appearances can be deceptive. Epidemiologists are not shy about trying to calculate health risks. They have been doing so at least since Florence Nightingale and William Farr began analyzing statistics on mortality in the 1800s. Nightingale was a pioneer in data visualization, including as the inventor of the pie chart, or the “Nightingale Rose Diagram.”
Their work may come in handy as we move toward the second wave of COVID-19. Farr’s insights about cholera are nearly as relevant today as they were in the mid-19th century.
The massive protests that began in early June created what scientists call a “natural experiment.” That is a big change that occurs unexpectedly (street protests) in an unusual situation (a spreading pandemic), making it possible to study the impact on health outcomes (infections, cases, hospitalizations, and deaths).
Natural experiments often happen before scientists can organize themselves to collect the baseline data needed to measure the change. But sometimes, the baseline data are available. In this instance, public health departments were already collecting data on COVID-19 daily cases, hospitalizations, and deaths before the protests. Also, before devoting effort to a natural experiment, scientists want to have some confidence that the study will produce a valid and credible result. When nothing is known about a question like “how many novel coronavirus infections and deaths will occur at protests?” even a less-than-perfect analysis may be better than total ignorance. Also, the cost is low because the data already exist. That’s the beauty of a natural experiment.
To prepare for a natural experiment, scientists use a special tool known as a “back-of-the-envelope” calculation (BOTE on Twitter):
- Start with some basic facts that have numbers attached — “input numbers.”
- Put them together in a reasonable way to calculate “guesstimates.”
- Calculate a high and low case guesstimate by using input numbers from the low and high ends of what seems reasonable. This produces a confidence “range.”
Put the cocktail shaker lid on and shake vigorously. Serve with a sprig of skepticism. The epidemiologist Trever Bedford stepped into the breach to create one such estimate.
When using the back of an envelope, half the battle is to decide which factors matter; the other half is to get believable numbers.
For the protest calculation, we want to know:
- How many people protested during the first several weeks and how many police and spectators were there?
- How many were contagious?
- How easily could infected protesters, police, and spectators transmit the virus to others?
- How many people back home will be infected if protest participants bring it home?
- What is the probability of dying if a person gets infected?
Bedford estimated that approximately 600,000 people protested. If 1 in 200 (0.5%) are infected, that means roughly 3,000 infected people would have been mingling with the protesters. Many of the protesters are from populations especially vulnerable to COVID-19, like Black and Latinx people. That could increase risk. But most protesters are younger, and the risk of dying is much lower for people under 45. The bigger concern is secondary transmission AFTER the protest. People can infect many others in households, bars, night clubs, and restaurants. Because much of America had not yet full reopened at that time, the effective reproductive number is around 0.9. That means every 10 infected people infect only nine other people. The number of infections tends to drop off as shown in the graph below.
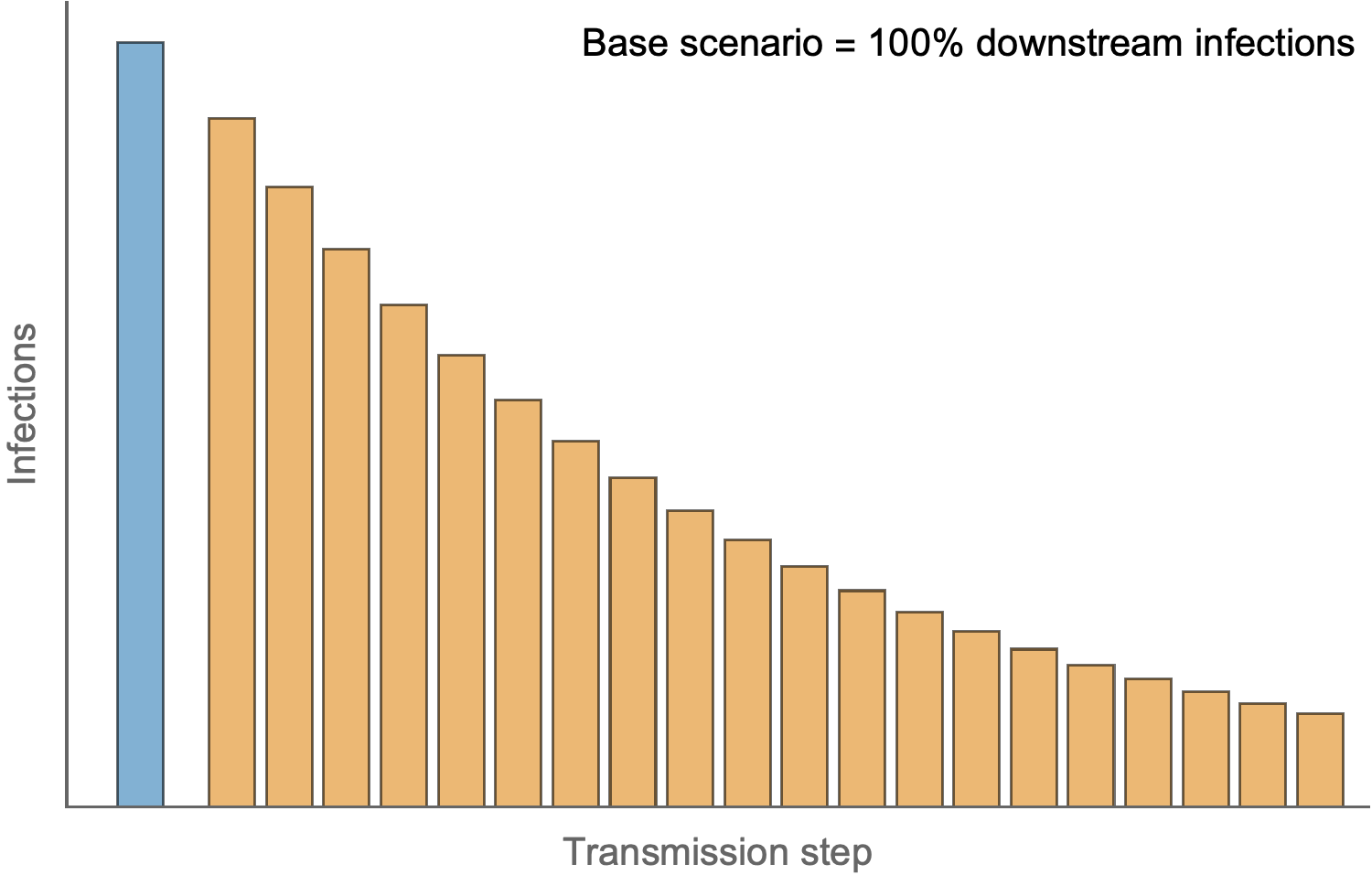
Source: Trevor Bedford
For the low scenario, assuming a fatality rate of 1 in 200 (0.5%), there will be 1,500 new infections each day and 15,000 secondary infections among protesters’ friends and family, eventually causing 50 to 75 deaths. The higher scenario assumes a reproductive number of 0.95 and a fatality rate of 1 in 100 (1%). The high scenario produces 3,000 new infections a day and a total of 54,000 secondary infections. Those 54,000 infections cause between 500 and 540 deaths.
So, the number of extra deaths from protests by BOTE is somewhere between 50 and 500. That may seem too low to be credible, especially since there were approximately 1,000 COVID-19 deaths per day when the protests began. Yet it has turned out to be probably correct. Over a month later, we have yet to see spikes in cases. In New York City, where more protesters gathered than anywhere else, new cases are still declining. More accurately, we are seeing spikes across the U.S., but not in the places where protests happened.
This is one of the key challenges of natural experiments. With many other things changing —reopening businesses and beaches, for instance — it may be nearly impossible to tease out the effects of any one set of large events. The excess deaths caused by protests are simply swamped by all the other human activities under way.
But aren’t excess deaths a problem? Even a small number is tragic if they could have been avoided. But consider that approximately 1,000 civilians are killed by police each year and Black Americans are 2.5 times more likely to be shot than whites. Is it worth 500 deaths now to reduce many thousands of future deaths from police brutality? There is no easy answer. Science can tell us about trade-offs, but not what to choose.
For that we turn to art. Like Delacroix’s famous painting of the French Revolution, Liberty Leading the People.

Caption: Eugène Delacroix, Liberty Leading the People (La Liberté guidant le people), 1830. Oil on canvas, 260 cm × 325 cm (102.4 in × 128.0 in). Collection Musée du Louvre
Or an updated version.
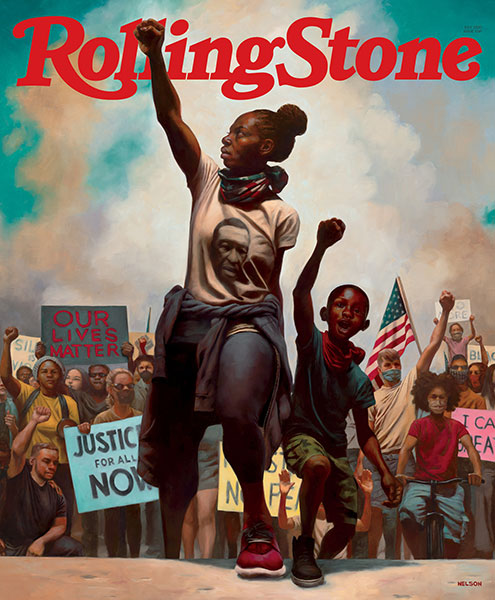
Sometimes social change is important enough to take some calculated risks. When the status quo is unacceptable, one may have no choice but to face the music. Decades of civil rights protests tell us the path to justice is not an easy one.
Why are the COVID-19 case counts going up in southern and western states while they go down in the northern and eastern states? Is it the weather?
As of July 22, 2020.
Some people thought coronavirus would magically disappear once the heat of April arrived. Now people say both the heat and humidity (or as they often say, “It’s not so much the heat, but the humidity!”)
Without question, coronavirus is spreading like wildfire in places where temperatures go up to around 100 degrees each day. But that spread is not likely caused by the heat (or humidity — some of these sunshine states are deserts). Coronavirus itself is quickly dispatched by heat and sunshine. Instead, coronavirus likes crowds, especially indoor crowds. And in the heat, crowds like air conditioning. And air conditioning is indoors, using recycled air. Like tuberculosis, coronavirus traveling on aerosol droplets may make the rounds more efficiently in air-conditioned spaces, where people are gathered to eat, drink, and be merry. Coronavirus is such a social butterfly!
But air conditioning exists everywhere in the U.S. What else could explain these different state experiences?
From 1776 on, the U.S.A. has been continuously falling apart as it holds together. Rebellion and secession are never far from the minds of some people. Even after the newly defined “Americans” in the “colonies” had slipped from under British taxation to form a “United States,” they quickly turned their resistance to new authorities, like the federal government and fellow states. By 1830 a crisis was afoot. You may have passed the Daniel Webster statue at the 72nd street crossing of Central Park.

That inscription? Words spoken during the Webster–Hayne debate of 1830. South Carolina began a movement to nullify tariffs — essentially a state declaring its own sovereignty and independence from the Union of States. Senator Webster was making the case for continuing a strong U.S. government. Those famous words also became the state motto of North Dakota. Lincoln paraphrased part of Webster’s speech in the Gettysburg address as he sought to bind the wounds of the Civil War.
The strength of our nation — a federal function that keeps borders open for commerce and maintains defense, taxation, and redistribution of resources to help economically weaker states — can also be a grave weakness if independent states pursue conflicting strategies. Controlling a pandemic may pose one of the greatest stress tests faced by any nation. Pandemics require a strong central coordinated and timely response. That is not something independent sovereign states do naturally.
Coronavirus thrives on open borders and people traveling freely. The rational response is to lock down. But by our constitution, states can’t close borders and people can’t usually be detained by the government.
This sentiment was best expressed in an essay early in the pandemic that asked, “why should the country play by New York rules?” Well, it turns out New York rules might have been better than reopening businesses too early. How do we know that? It can be summarized easily by R0, the reproductive number. As you recall, that’s the number of other people each infected individual will infect on average. With some fancy math, it is possible to calculate a daily reproductive number (Rt) for a spreading virus. It can be plotted for each state.
Here is New York:
And Florida:
Rt is a handy summary of all the actions taken by leaders and the people of a state to contain spread. Whether business continues or not, whether people stay at home, whether they wear masks, whether they stay away from one another. The more time a state spends in the red, the more likely there will be an outbreak eventually. Comparing the two graphs, you can see why Floridians now face an explosion of cases and a mandatory 14-day quarantine if they travel to New York.
You may have heard the term schadenfreude. You know, that warm and fuzzy feeling you get when the mean kid at school finally gets punished or when a massive coronavirus outbreak happens in another state that thought the virus would never, ever affect it. (Looking at you, Florida.) Many states decided not to play by New York rules. That was their right under our federated system of sovereign states.
New Yorkers, having driven new case counts down to “only” 600 per day, will be tempted to feel schadenfreude and celebrate their New York State of Mind. But the Rt that was less than 1.0 for a while is trending above 1.0 in recent weeks. As states reopen, even carefully, cases may start to increase again. Perhaps New Yorkers and all Americans would do well to put schadenfreude aside and meditate instead on Proverbs 16:18: “Pride goeth before destruction.” And repeat many times each day, “Liberty and union, now and forever, one and inseparable.”
Everyone expected that states like Georgia and Florida would pay dearly for reopening so early. Florida was flaunting crowded beach pictures. Georgia reopened its tattoo parlors and restaurants. But cases and deaths did not increase right away. Were the epidemiologists wrong? Shouldn’t these states be punished by the pandemic if they reopen too soon?
As of July 15, 2020.
CQC does not recommend conflict between northern and southern states. When in a war, don’t get distracted. Focus on the big picture. Some people can’t get enough trouble. They will invite new troubles to your party. They may congregate for the wrong reasons; like in Missouri, where a COVID-19 pool party drew many enthusiastic participants on Memorial Day weekend.

Missouri might have lucked out — the coronavirus super-spreaders must have missed this one since we didn’t see much of a bump there. Or maybe the outdoor pool just made it hard for the super-spreaders to get the virus out. We now know that the virus doesn’t transmit easily outdoors.
To your other question: should these states be punished for their irresponsible reopening policies?
You seem obsessed with notions of biblical justice. You must know that the grim reaper operates on his own timetable, usually working steadily to get the job done, but occasionally working overtime. The reaper seems to have plenty of bandwidth available when war, famine, or earthquakes come along.
Leaving justice aside, the scientific answer to your question is R0. And kappa. R0 you will recall as the reproductive number — the number of individuals that a person who is infected will infect. For coronavirus, the estimated R0 — without changing the way humans interact — is somewhere around 2.5 to 3 people. When the pool party gets going, it seems like one person can infect three others, then those three infect three more, and then those nine infect three each, resulting in 27 infected people.
But two funny things about R0. First, it has no time dimension. One person can infect three people, but we don’t know whether that will happen within five minutes or five days. Second, R0 is an average. One person infects three others . . . on average. Why does that matter? Imagine 100 people are infected. If R0 equals three, we would expect the 100 infected people to infect 300 people. But that could play out in different ways. Perhaps each of the 100 people infects three people. But what if one of the 100 infected people infects 300 people and the other 99 infect zero people? Or three of the infected people infect 100 people each while the other 97 infect zero? Or 50 infected people infect six people each while the other 50 infect zero? Or . . . you get the point.
In every one of the scenarios above, R0=3 but the pattern of transmission is different. This pattern is known as dispersion — some people in the population infecting more than others — and it is measured by kappa. When kappa is low, then only a special few people infect many others and the rest infect zero. These special few people are known as “super spreaders.” They are in the right place (i.e., living in close quarters) at the right time (i.e., maximally contagious). Contagiousness may be short-lived, lasting only four or five days. But with SARS-CoV-2, two or more of those days may happen before super-spreader feels too sick to attend the pool party.
The point is, if there are super-spreaders, then the risk is not evenly distributed everywhere at the same time. Even after reopening, most pool parties — even indoor ones — may turn out just fine. Whether a pool party turns into a super-spread event depends on the right person being in the pool at the right time. If super-spreader decides to go for a free solo climb rather than attending the pool party, there will be no transmission chains at the pool and the alcohol-fueled swimmers will have lucked out.
That might have been the story of Georgia and Florida after Memorial Day. They may have simply been lucky because the super-spreaders stayed away from the pool parties. But as Californians who have lived through earthquakes and fires know, and as every gambler knows, luck has a way of running out eventually.
And now, just over a month later, luck has run out — not just in Florida and Georgia, but in Arizona, California, Texas, and many other states that opened early. Tragically, once it arrives, viral punishment tends to be sure and swift — especially when the grim reaper is standing by, ready to heed the call.
Image caption: Albrecht Dürer, The Four Horsemen, from The Apocalypse, 1498. Woodcut, image: 15 1/4 x 11 in. (38.7 x 27.9 cm); sheet: 15 1/4 x 11 7/16 in. (38.8 x 29.1 cm). Gift of Junius Spencer Morgan, 1919 19.73.209.
Hospitalizations and deaths are rising. You are tempted to say, “I told you so.” But as all the U.S. states try to reopen, keep in mind that you may not want to tie your happiness to the fates of others.
People are suggesting that apps on our smartphones could help control the pandemic by making it easier for people to know if they were exposed to coronavirus. Can Silicon Valley help defeat the coronavirus? Should I download an app?
As of July 8, 2020.
CQC keeps up on all the latest technology. It has been so since that first tech purchase back in the 1960s.

This Motorola transistor radio could pull in all the AM stations from Detroit, Flint, and Saginaw. It offered a handy way to track Al Kaline all the way to the Tigers’ World Series win in 1968. And a gateway to new music. All that in distant Midland, Michigan. Silicon chips were invented around 1960, but Silicon Valley and the billions of silicon chips that surround us every day were still a faraway future.
Transistor radios probably wouldn’t stand a chance against coronavirus, but smartphones? There’s a reason they’re called “smart.” They seem like the perfect solution for contact tracing, especially against a disease people can spread for days before symptoms appear. Here is the value proposition (as they used to say back in day of huge tech conferences):
Person A has coronavirus but doesn’t know it. Person B is a stranger, standing for several hours next to person A at a huge indoor political rally. Both are hollering and waving signs. Two days after the rally, person A feels sick, and tests positive for coronavirus. The friendly contact tracer calls person A to learn about the past two weeks.
Person A: “I was at an indoor rally.”
Contact tracer: “How many people were there?”
Person A: “Ten thousand, I think?”
Contact tracer: [crickets]
Now imagine both Persons A and B have their smartphones switched on. And both downloaded the app. The app recorded every phone that came within 10 to 15 feet, using Bluetooth technology.

Now Person A can activate the app on her phone and push the button that says “OMG, I had a positive test for coronavirus today!” Instantly, the other rallygoers with the app running get a notification “Tag! You’re it! You got too close to someone with coronavirus!” Now Person B and thousands of other tagged rallygoers can isolate, get tested, wear masks, and chew their fingernails as they wait to see whether they will get sick from the coronavirus.

For privacy’s sake, that’s all the information Person B gets. Person B won’t know whether it was the rally or a trip to the grocery store that triggered the alert.
But as you can imagine, a lot can go wrong. And a lot is going wrong. First, most people have to download the app. Who wants to add another app to their smartphone, especially one that only delivers bad news? People prefer to download good news apps or games. In countries where these apps are available, fewer than a third of people downloaded them. That’s a problem. Modelers estimate that more than half of people have to download an app for it to be effective. Outside of authoritarian countries, getting so many people to download an app is a Herculean task. The app would probably have to promise to deposit $500 a day into your bank account. Even then, most people might decide the app was another Internet scam. See how important trust is?
Now imagine having to stay home for 14 days every time your smartphone alerts you. Chances are that most of the alerts would be false alarms — like the phone of the person in the apartment next door who you have never met. Or the kid hacker who thought it would be cool to hack the system and send an alert to everyone who downloaded the app.
And people have to trust the app with their privacy. What if the app is sending their personal information to Russia-based gangsters, state-sponsored cyberwarriors, or Facebook and its targeting advertisers? Norway recently pulled an app over privacy concerns.
Smartphones may be smart, but they aren’t human. Even though smartphones have played a pivotal role in social justice, documenting racial violence and bringing it into public view, smartphones and apps are not yet ready to help in the war against coronavirus. Celebrating coronavirus apps is definitely premature.
Instead, you could celebrate the two recent Supreme Court rulings protecting LGBTQ rights under Title VII of the Civil Rights Act and protecting DACA beneficiaries, saved again by sloppy disregard for the Administrative Procedure Act!
Celebration may not feel easy in the midst of so much tragedy, anxiety, and stress. If you are feeling down, it might help to recall the people who create joy against unholy odds. Like Clifford Brown, a one-of-a-kind jazz trumpet player you have probably never heard of.

The 1954 recording of his composition “Joy Spring” is pure celebration. It reminds CQC that joy and tragedy are two sides of the same coin. Two years after Brown recorded the song (and many other great ones), he was killed in an auto accident as his band drove to Chicago. He played his last gig in a racially segregated night club. He was 25 years old.
Still, he reminds CQC that even if sadness is inevitable, joy is also within reach. If the complexity of bebop is not your musical thing, try a more danceable joy. Gloria Gaynor has that covered. You will survive.
Everyone talks about testing and determining who has had contact with those who tested positive and then quarantining those people. How does this work? What if people don’t want to quarantine, or what if they don’t want to stop working or are the primary caregiver of a child or ill person or don’t like being told what to do by the government? Also, if someone dies from COVID-19 is the corpse still contagious? If so, is it safer to keep it off ice?
As of July 1, 2020.
That last question is hard-boiled. Perhaps you have been reading Raymond Chandler. The noir style of filmmaking emerged during and after World War II. Films like The Big Sleep and Double Indemnity entertained audiences who had lived through an economic great depression, moral injustices, war, and anxiety about an uncertain future. These movies, shot in black and white, revealed a grim and gritty world where ordinary people struggling to survive were surrounded by rich titans, mobsters, gamblers, and political grifters. Starting to sound familiar?
The corpse of a coronavirus victim is probably not very contagious. Coronavirus is transmitted by aerosol droplets from people when they are breathing, coughing, or sneezing. Not much of that happening in a morgue. Coronavirus patients tend to be most contagious just before they develop symptoms and during the first week of illness. Most people who die of coronavirus have been sick for a week or more. By that time, they may no longer spread very much virus, ice or no ice.
If you want to understand the challenge of contact tracing without trying it yourself, the movie Panic in the Streets offers a surprisingly accurate noir portrait. Shot on location in postwar New Orleans, a place where people are living in quiet desperation, silently drinking coffee, crowded in a bar, packed into the longshoreman’s hall waiting for jobs, lugging bananas and sacks of coffee at the wharf, laboring on a merchant marine ship under a tyrannical captain, living in cramped rooms attached to nightclubs and restaurants, or answering questions in a police station.

Richard Widmark plays the underpaid public health officer called to the morgue on his day off. He learns that a dead man had more wrong with him than bullets in his chest. He was also sick with a strange airborne disease that was about to kill him even before the lead got in the way. Worse, he probably infected everyone including his killers.
You won’t see a more vivid portrayal of what makes contact tracing work: people have to trust you. No one is ready to trust a college-educated public health doctor in a crisp uniform or cooperate with the chief of police, especially not the people living under the thumb of poverty.
If you think fear of a pandemic is all the justification one needs to gain public trust, think again. Just look at Arizona. Or resistance to masks. Read about the Anti-Mask League of San Francisco. These skeptics were marching in 1918 as the worldwide flu pandemic was carrying away tens of thousands of souls.
Authority is not enough. Liberty, privacy, and resistance to authority are deeply embedded in the American psyche and wind throughout American history. So it should come as no surprise that modern contact tracers face the same challenges Richard Widmark faced. Members of the new Massachusetts Community Tracing Collaborative (CTC) illustrate that one needs cultural empathy and language skills. CTC leaders succeeded with contract tracing and quarantines to contain Ebola outbreaks in Africa. But they have met their match in Massachusetts: “The critical element the American system seemed to lack, which made tracing especially hard, was the social safety net — the CTC was forever trying to stitch together its holes.” It is difficult to get people to isolate or quarantine themselves for the good of their families and neighbors if they are at risk of losing a job, an income, an apartment, and food to eat.
Even in liberal Massachusetts, a good safety net is hard to find. And if it is hard to find a safety net there, if cases are rising in nearly half the states, and if contact tracing is not really an option in America, this may be a good time to look for the panic button.

Because if Americans decide that New Hampshire (“Live Free or Die”) has it right, 200,000 deaths by October will be another underestimate of the power of coronavirus. It is difficult to argue with viruses. Panic in the Streets ends with the outbreak contained. If only Richard Widmark were here to rescue us today.
I acquired a loaner car, making activities like camping possible. Even more tempting is a D.C. visit but I worry about bringing my N.Y.C. cloud to D.C. Should I bring a tent? Get a test when I arrive? Or tamp down the temptation and stay away?
As of June 24 2020.
The lockdown time is clearly drawing to a close. The time of Exodus approaches. Wandering spirits are dreaming of the open road.
And why not? The case counts are declining in some places. Infections have gone down because of our successful collective efforts to stay away from each other.
And people are breaking the rules. Like the chief advisor to a famous British politician. Are you surprised to learn that the advisor who brought Brexit to the U.K. would break the lockdown rules to drive 260 miles with his spouse even as they had symptoms of coronavirus? This urgent trip, supposedly to deliver children to relatives, went sideways with a little jaunt to a nearby tourist destination. Price? A fine of 60 pounds sterling and a bit of widespread condemnation for disregarding the law.
Fortunately, you do not live in England. Travel in the U.S. is not prohibited. The liberty to drive your car as you wish is a nearly absolute right, almost as guaranteed as the right to bring high-caliber guns into statehouses, churches, and schools.
Science supports car travel, as long as you never get out of the car. Cars may be the retro secret to bringing back the movie business. Why stream cinema on your laptop when you can visit the Great American Drive-In!

With Charlton Heston to lead you out of bondage, what can go wrong? Note that the 10 plagues visited upon the Egyptian slave masters did not include coronavirus.
And camping? Why not? It seems like the perfect physical and social distancing activity as long as you avoid the outhouse.
That trip to D.C. though? Maybe not so great. Not because travel is forbidden, or the loaner car might break down, or you might be unexpectedly called by nature to use a public restroom. But because it is difficult to forecast the current COVID-19 risk in all the places you’ll go.
To eliminate risk, you and anyone you would visit should quarantine for 14 days. No contact with others. That makes for a long trip to anywhere. But haven’t you mostly been doing that already? It seems like your risk of having the infection is nearly zero already. If the person you intend to visit has done the same, getting together also should have a risk of nearly zero.
Eliminating risk entirely is not compatible with living. So you could base your decision on estimating and controlling the risk. For now, only about 4 percent of the American public is thought to have been infected, according to a report from Imperial College. In New York, the estimate is around 16 percent and in D.C. it is about 11 percent. For now, the I-95 corona corridor still seems pretty risky.
However, most of those infected people either died, recovered, or were never symptomatic. Few of them will be contagious right now. You are less interested in how many people had the infection (which the antibody test can tell you) than how many are actively contagious. The best measure is how many new cases are occurring each day in a local area. Fortunately, some websites offer daily case counts and even the current effective R0 (i.e., how many people are getting infected on average by each infected person). New case counts are declining in N.Y.C., but still a bit higher than you might like. Case counts in D.C. and its immediately surrounding counties have also been declining but may still be too high for your liking. The question is: Are you bringing an N.Y.C. cloud or going into a D.C. cloud?
Either way, thanks to control measures, the effective reproductive number has been near 1 for a while. So overall, your risk of encountering a coronavirus-infected person is low. If you keep physical distancing during your visit you can make the risk even lower. Like they do in Japan, avoid the 3 C’s (closed spaces, close contact, and choirs — er, crowds). And since indoor crowds are banned, hopefully there will be no crowds to avoid.
Last week, CQC answered a question about the higher relative rate of COVID-19 infections and deaths among Black people. This CQC takes a deeper dive to examine how big the differences are and why this is happening.
As of June 17, 2020.
Why is this happening? In epidemiology of infectious disease, the answer is always community. Viruses need communities to spread themselves. They need people and geography. And viruses move through communities depending on social conditions. Communities have different abilities to resist, depending on conditions. Infectious diseases of all kinds thrive where there is deprivation. And there lies the answer to racial disparities in cases and deaths: structural racism. In the U.S., deprivation has been imposed for decades on communities of color.
Even for states that like to imagine themselves enlightened, history is complicated. Massachusetts, for example, is proud of its role in the abolition movement in the 1800s, and it has achieved some degree of equity over the years. But, even there, it is not hard to guess which towns are most affected by coronavirus. In the map, you see the hot spots in salmon and red colors.
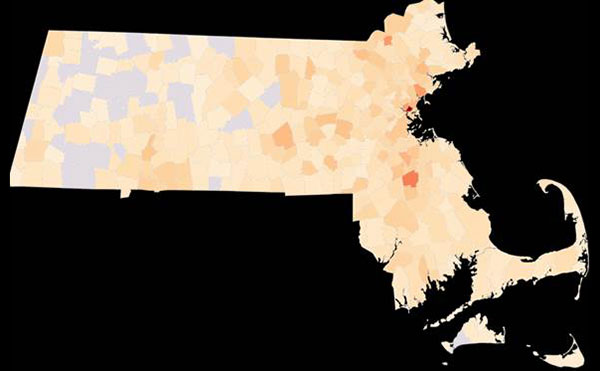
Springfield, Worcester, Lawrence, Lowell, Brockton, Boston, Chelsea, Fall River, Everett, Lynn, Revere, Randolph, and New Bedford. Why is CQC not surprised? It isn’t difficult to predict COVID-19 attack risk: more Black people, more Latinx people, and more people living in poverty. If one or more of those factors describes the population, the virus will spread. It may also be more lethal.
Do all the people in those communities, including white people, have a higher risk of catching, transmitting, and dying from coronavirus or is the risk higher only for Black, Latinx, and poor people in those communities? If communities with larger shares of Black populations also have more COVID-19 cases, then doesn’t it follow that more Black people are becoming infected by COVID-19? That may be true. Or it may not. Making claims about the experience of individuals within communities based on comparing communities is known as the ecological fallacy.
Start with two groups of counties and the people who live in them. One group of counties has a higher percentage of Black people than average (13% is the average among U.S. counties). The other group of counties has a lower percentage. Now, we analyze which group of counties has the higher rate of COVID-19 cases. If the cases are higher in the counties with the higher percentage of Black people, then we conclude that Black people are more likely to be at risk of COVID-19.
However, we must be careful drawing that last conclusion. If urban counties have higher percentages of Black people and also more travelers from other places, then case counts could be higher among people who live in urban counties that happen to have larger percentages of Black people. That is what is called a confounder: a characteristic (urban) that turns out to explain the effect we thought was due to another characteristic (race). There may be no race-related difference within the urban counties. It might even be that another group, such as Latinx people, have the larger share of cases. We can’t know for sure which scenario is true until we have the individual-level data.
Still, it is possible to adjust for some of the confounders using statistical models. Below is the graph that shows the relationship between the rate of cases in a county (y-axis) and the percentage of the county’s residents who are Black. Clearly the rate of cases is higher in counties with a higher percentage of Black residents, as the right side of the picture shows. But the graph is not a straight line. The line to the left of the graph ticks up on the left, showing a higher rate in numerous counties with very few Black people. That seems odd until you realize that we have been reading about meat-packing plants and prisons with epidemic outbreaks in predominantly white rural counties.
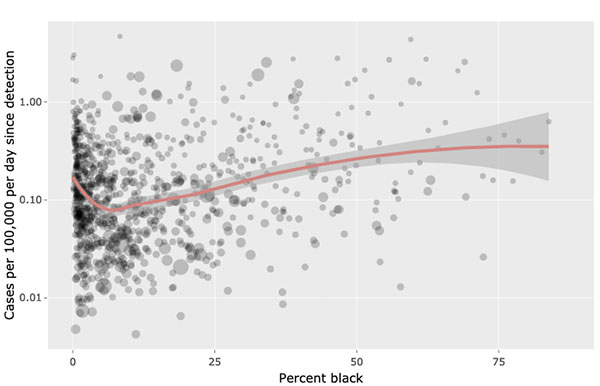
Even that uptick in nearly all-white counties may be because of new cases among meatpacking workers, who are overwhelmingly Latinx, and their families and communities. Over time, as the pandemic moves to rural America, county-level analyses could paradoxically reverse. They might show a higher risk in counties with smaller percentages of Black people. In a county-level analysis that can happen even if the Black residents of those counties are at higher risk of infection and death from COVID-19. That is the core problem of the ecological fallacy. You can’t really say what is happening to the individuals living within counties if all you can see is county averages.
Studies with individual-level data can tell us more about why some people are at greater risk than others. A big part of the story is about exposure to the coronavirus. As we are learning, Black and Latinx people are more likely to work in occupations where they cannot work from home, their workplaces are less likely to be amenable to physical distancing, they are more likely to live in multigeneration households that allow spread within families, and they are more likely to rely on public transportation. The list of other factors is long.
If structural racism is the answer that ties together all the factors, what can be done? Three months into the worst pandemic in a century, the Black Lives Matters protests, gradually built over many years of tireless work by dedicated activists, may finally be breaking through the seemingly immovable door that has been stuck shut for at least 40 years.
It will be an irony if it takes a global pandemic to finally bring us to the verge of a harvest for the world.
Why do African Americans account for such a high percentage of COVID-19 cases and deaths? Is it because of genetics or other risk factors?
As of June 10, 2020.
CQC is often startled by questions about race that include the word “genetics.” Since the sequencing of the human genome several years ago, many geneticists have called for an end to the use of race as a biological category. Why? Because genome science finds very few differences in the genes of humans. Genomes from people across the world are more than 99.9 percent similar. Observed differences, with very few exceptions, are rarely sufficient to explain differences in diseases or outcomes. Like the coronavirus, with its minor differences from random mutations as it spreads, humans have small genetic differences. Mostly they are inconsequential, of the kind that allow Ancestry.com to tell you whether you might be related to famous celebrities or their descendants.
So, putting genetics aside, there is a simple answer to your question and a more complex answer.
The simple explanation for differences in COVID-19 (or other diseases) cases and mortality is whether you live in a country organized and structured to discriminate against some of its people, whether by skin color, ethnicity, or social class. The complicated explanation is multifactorial: the long list of risks that are a result of discrimination.
With infectious agents like COVID-19, anything that might increase the risk of transmission is a factor. That includes inability to physically distance because you work in a job that demands close contact (like a nursing home, a hospital, a prison, or a meatpacking plant), using public transportation, or living in a multigenerational household or with roommates in a small space because of high rents. And that doesn’t even include factors like inability to get access to health care or trust the health care you can get. Nor does it include the emotional stress of trying to avoid dangerous random encounters with bigots. Prolonged emotional stress weakens immunity and increases the likelihood of certain chronic diseases.
The problem with the scientifically correct answer “multifactorial” is that while it sounds serious and scientific, it also offers a distraction from the main overarching cause of the multiple factors: racism. One thing racism seeks is a place to hide in plain sight. Like the coronavirus, racism seems designed to multiply and spread, infecting the people who will inflict its effects on others.
If your goal is to understand why COVID-19, or any other infectious disease, affects some people more than others, don’t look to the virus. It doesn’t discriminate. Ask about the social conditions that lead to transmission of the virus. If someone is living in those conditions, they will be more likely to get sick. And if a person’s health has been weakened by the conditions of life, they are prone to get sicker and are more likely to die.
When answers are hiding in plain sight, complex regression analyses to control for that long list of factors may not be all that helpful. That is especially so if your country can engineer the outcome through its actions. To become #1 in the world in coronavirus cases and deaths, your country need only create the conditions that make people unhealthy, perpetually disregard or oppress the people affected by those conditions, and be willing to delude yourself that oppressed people are to blame for their own situation. The U.S. may be #1 in coronavirus, but other countries aren’t far behind, notably Brazil, Russia, and India. Guess what those countries have in common.
If you said poverty in the midst of wealth, you could be on to something. Or a history of ignoring the coronavirus? Once, not long ago, we were mobilizing for the war against coronavirus. You might have thought government would still be mobilizing. That war is far from over. But at least some U.S. leaders have decided the coronavirus is boring — or that they have more to gain politically by starting other wars.
As James Baldwin said, “[I]gnorance, allied with power, is the most ferocious enemy justice can have.”
In the places where we have really been distancing/locked down since mid-March (NY, NJ, PA), who is still getting COVID?
As of June 3, 2020.
A) Rule-breakers
B) Essential workers and families
C) People in residential facilities (like prisons or your home after all your teen/adult children migrated there)
D) All of the above
You guessed it. The answer is D. Even in lockdown, transmission is still possible. Until the robots take over all our jobs, we humans will still be encountering each other one way or another.
Also, the other answer to your question is “yes.” WHO is still getting COVID. That international health organization “got” COVID from the beginning. They knew how serious it would be. They warned the U.S. And we ignored them. And now we are in a pickle. Also, WHO is still on first.
Remarkably, New York, New Jersey, and Pennsylvania have reduced the community transmission of coronavirus. New cases are dropping every day! In the epidemiology business we call that reducing R0 (pronounced “R naught”). R0 is the number of people one infected person can infect. If R0 is larger than 1, then an infection will spread. If R0 is less than 1, each infected person, on average, is infecting less than one other person. When R0 is less than 1, coronavirus is going nowhere. Case counts drop. Deaths drop. Things eventually can get back to normal.
And remarkably the calculated R0 is less than 1 in many parts of the U.S. including NY, NJ, and PA! Seems like great news. But the bad news is that R0 is an average. Why does that matter? Because there is variation around the average. Some people are staying at home and living alone and, even if they get infected somehow, will infect zero other people. R0 literally equals naught. If they have one roommate and infect that person, R0=1. On average, R0 will be less than 1 because of all those other people who are not infected and not infecting others.
Where it gets dicey is when people leave home and are exposed to each other in closed spaces for longer periods of time. Like going to work or school. Or living in prisons or care homes for the elderly. How dicey? Read this handy summary of the science on transmission. Once infected people get out in the world, they can infect others. And they can infect dozens of people. South Korea had zero new cases of COVID-19 for 18 days straight. Amazing! So it started to open up businesses, including dance clubs. That didn’t last long. One 29-year-old partygoer fell ill after his night on the town. COVID-19 hangovers are the worst. Apparently, more than 100 new cases have now been traced to this one person having one wild night on the town.
So the dance clubs are closed again.

Notices of the Seoul city emergency administrative order to ban gatherings are seen posted at the entrance of a temporarily closed dance club. Photo: Simon Shin/SOPA Images/LightRocket via Getty Images
As the sign says, “No Power Dance: You Are Still Hot.” Hey. Thanks for that. I think?
Keeping R0 low is the best policy option we have while waiting for a cure. But R0 has to be kept low everywhere all the time. R0 was heavily featured in a recent confusing roadmap released by the U.K. government.
Seems intuitive, right? But let’s do the math. If there are just over 100,000 new infections each day in the U.S. and R (the rate of infection) is 1, then the COVID Alert Level (CAL) will rise from 100,000 to 100,001. Hmmm. Something is wrong. Let’s say R is 2. The CAL shoots up to 100,002. That doesn’t seem impressive either. Maybe there was a typo and the plus sign was actually a multiplication sign? If R is 2 and number of infections is 100,000, CAL is 200,000. Okay that sounds a little more like it. If R goes down to 1, CAL drops to 100,000. Suddenly, CQC finds this math not very helpful.
Let’s stick to basics. The goal is no new cases. That means R0 must be really low to get case counts down. Imagine zero cases for 18 days! The U.S. is only 100,000 cases per day above that.
Don’t give up hope though. Slow and steady wins the race.
As long as R stays below 1, cases will drop. We won’t see large outbreaks. Like the tortoise we may not be out on the dance floor quickly. It may be the last dance for a little longer. But remember, like Donna Summer forever, “You Are Still Hot.”
I have a handheld garment steamer used to remove wrinkles from clothing. It puts out a very strong stream of live steam. Would this be effective to kill virus on my masks, allowing them to be reused safely?
As of May 28, 2020.
The topic of masks remains a hotbed of confusion, misinformation, and conspiracy theories. To cut through the fog, turn to the Hollywood Reporter for the truth about the masked man. Armie Hammer? Or tune into that new hit unreality show The Masked Singer. You could lose your mind even more than it is already lost through the effects of extended physical distancing.
Questions about masks have become a staple of cable news interviews and water-cooler chatter (even in the absence of news and a water cooler). Do masks work? How do I clean my mask? Can my mask infect me? How obnoxious can I be if someone in the street is not wearing a mask? What if I encounter a masked man armed with an AK-47? What about one armed with a garment steamer?
To understand masks, CQC recommends a new approach. CQC calls it “precision.” Most questions are stated generally. Science is not about answering general questions. Science is about asking precise questions so you can make general statements. If your answer to a general question is, “it depends” or “what do you mean?” then you are taking the first steps in the quest to be scientific.
Take the question: “Do masks work against COVID-19?” Scientific answer: “It depends. What do you mean by ‘work?’”
To tackle mask questions, we need to distinguish the purposes of masks. They are:
- To protect me, the rugged individualist, from the rest of humanity.
- To protect everyone else (i.e., my community) from me.
- To make people feel in control in the midst of an overwhelmingly stressful pandemic.
- To create mysterious and oddball characters in countless inane TV shows, movies, and theater productions.
We can easily dispense with #3. There is no way to feel in control and, as Zen masters might say, control is an illusion like everything else.
We can also dispense with #4 using these handy images. Seems unlikely any of these would work against COVID-19.

BTW, for Masked Singer fans, hot off the press: the frog is the new front-runner in the final four!
If the question “Do masks work?” is about protecting me from everyone else, the answer is simple: N-95. The N-95 respirator/mask is the only one that filters enough fine particles to give you a chance against thick clouds of the coroanavirus. What about those KN-95 masks? They are more or less equivalent, except the KN-95 is the Chinese standard.
But if you want to protect the community like a true heroic first responder when stepping out, your options expand considerably. They include the surgical mask (you know what those look like) and the face covering (that stylish alternative):

Trendy and cool, right? Also, way more comfortable than all the other mask options. Good for working out (you can actually breathe), listening to music (ear buds don’t get tangled up), and arguing with strangers in the grocery store (easy to look a bit threatening).
Based on a cursory review of that dubious section of every scientific journal known as “letters to the editor,” it seems surgical masks might be helpful for some diseases and some situations. For example, guinea pigs appreciate when people wear masks: “Mask wearing by patients with pulmonary tuberculosis (an airborne infectious disease) has been shown to reduce infectivity to guinea pigs by 56 percent.” And there is the laser light evidence that masks reduce droplet transmission among people who say the phrase, “Stay Healthy.” CDC guidance suggests cloth face coverings in areas where there is community transmission.
CQC, you seem to have forgotten my question: Can a garment steamer kill coronavirus on my mask? Ha. CQC was so busy striving for precision that your question got lost. Seems likely the garment steamer should work. RNA viruses break down in heat. But whether garment steaming is a worthwhile activity to reduce COVID-19 transmission to you personally or to the community? It depends. Different question. Different answer.
Masks are also big among bank robbers and horse thieves. If you are not a big city type worried about being a good citizen in your community, you could follow the frontier way. Each of us, rugged individualists, crafts our own plan. Want to go outside without a mask? Have lunch with a friend? Don’t give a damn about civil society? CQC suggests you go out on horseback. Good physical distancing. It is hard to get too close to a fellow rider while on horseback. You probably won’t want to eat lunch up there. And horses get restless if you linger too long in one place. Yes. This seems like the perfect maskless American solution to COVID-19. And if you want to become a horse thief, all you need is a mask.

Photo courtesy Michael Schneider
My aunt is going to visit my mother today so they can go for a walk together. My aunt lives about a half hour away by car; they have not been quarantining together. They also decided they should have lunch together. My aunt has been going out a lot more than my mother. I’m worried she’s been more exposed. When can people start to see each other or share a meal when they haven’t quarantined together? What kind of precautions should they take? My aunt has been chafing at the stay-at-home order and now I’m worried my mother will get sick.
As of May 26, 2020.
Humans are social creatures. Regardless of age, most people find it challenging to stay in isolation. Even astronauts, aquanauts, and Antarctica-nauts find isolation challenging. Isolation was a problem before COVID-19. Just ask the U.K. Minister of Loneliness. But COVID-19 introduces a whole new set of problems. “We can expect depression to kick in, and depression and anxiety are kissing cousins.” Kissing? See? Even mental health problems don’t like isolation.
Experts say the negative psychological impact of isolation in quarantine can be reduced. Samantha Brooks, researcher at King’s College London: “A huge factor in the negative psychological impact seems to be confusion about what's going on, not having clear guidelines, or getting different messages from different organizations.” Well, maybe we still need to work on this one.
In any event, it is a natural psychological consequence that your aunt and your mother want: to have lunch. And CQC can relate. We miss lunch — and in-person happy hours.
Your question brings up bubbles. Soap and handwashing aren’t the only activity generating bubbles in the COVID-19 era. Look, bubbles in Central Park.

Image courtesy Antonio Cinotti via Flickr
And then there’s us. We are producing our own little isolation bubbles. In a pandemic, under stay-at-home, those bubbles are de rigueur. Bubbles have to stay small to “stop the spread,” “crush the curve,” and “kill the undead COVID.” As we know, the virus floats through the air with the greatest of ease.
And when people go out into the world looking to mingle their bubbles, say on a cruise ship, or a lunch outing, they offer a most appetizing lunch for COVID-19 — humans in motion. Humans in motion are also an all-you-can-eat buffet for contact tracers. To see just how fertile a field human travel can be for COVID-19, check out this study based on a single docking of the Diamond Princess cruise ship in Taiwan. Just one of the 3,000 visitors to Taipei was able to potentially infect 13 other people, according to the digital fingerprints left by his or her cell phone.
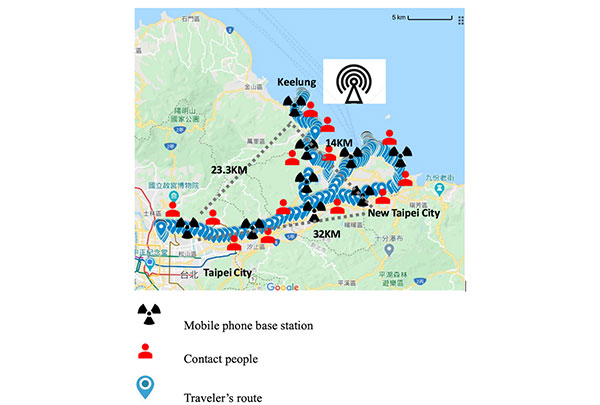
Overall, passengers encountered 627,386 people during their brief visit to the island. Ouch! But the story has a happy ending. Public health officials quickly texted all 627,386 people that they may have been exposed to COVID-19 and asked them to self-isolate for two weeks. The result? People in the contact group had a lower rate of respiratory illness and hospitalization than the general population. There were virtually no COVID-19 infections.
Could they have just been lucky? Possible. If so, 627,000 people are feeling lucky that the Diamond Princess sailed away without ruining their country. Way more lucky than the 1.6 million Americans infected with COVID-19.
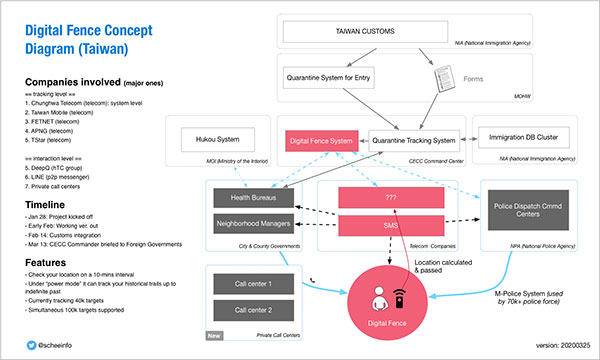
The government of Taiwan even has a plan to keep their bubble clean. They call it the digital fence concept.
Without a digital fence, your aunt should not visit for lunch. At least not yet. And if she must go out, she should skip lunch. Unless they can eat it in less than five minutes and 10 feet apart.
Maybe they can enjoy a baseball game. Turns out baseball is back! In South Korea! The masks are funny and no fans in the stands, but who needs fans when you have TV and radio? I mean, how many of you went to baseball games anyway? You didn’t want to be showered with beer and pizza. And if you did, you can probably shower yourself with beer and a slice in the comfort of your own TV room.
So fire up ESPN in your mini-bubble and enjoy some live baseball. Game time is tomorrow at 5:30 a.m. on ESPN2 featuring SK Wyverns vs. Doosan Bears. Look, South Korea is not going to accommodate America’s schedule. You want baseball, get a plan, America! At least you don’t have to worry about taking the subway to the game. In fact, you couldn’t take the subway if you wanted to. For the first time in 115 years, the subway is closed every night between 1:00 a.m. and 5:00 a.m.
This weekend, drunken middle-of-the-night subway riding is not an option. That’s probably a good thing. Until we have contact tracing like Taiwan and South Korea, cleaning the subway bubble is at least a plan. And even a weak plan is better than no plan at all.
Someone told me there are 102 candidates for a vaccine already being tested. And that monkeys are getting immunity. How can this be happening so fast when it takes months each year to come up with the flu shot? How soon can I get the corona shot?
As of May 21 2020.

Did you notice that bioscientists are always holding those weird injector things that work by thumb? That’s called a pipette. In a lab before med school, CQC’s job was to pipette hundreds of miniscule bits of liver and enzymes into little plastic tubes. Turns out the key qualification to be a research assistant in a Nobel-prize-winning laboratory is to have an opposable thumb. What the heck is an opposable thumb? It is a thumb that can be placed opposite the fingers of the same hand. Not all animals have opposable thumbs. Check your cat or dog. Then check a primate — monkey or orangutan. Having an opposable thumb enables primates like you and CQC to use tools: hammers, typewriters, and of course, smartphones. That thumb played a key role in cinema history, enabling one of our monkey ancestors to throw a bone that turns into a spaceship.

At any rate, CQC can tell you pipetting is really hard on the thumbs. We should be grateful to these essential thumb workers. They are sacrificing their opposable thumbs to do vaccine development that may save the human race.
Also, our opposable thumb first cousins are in on the vaccine testing action. Scientists have reported a vaccine that protects monkeys from coronavirus! Now you aren’t so embarrassed to think your immune system may be closely related, are you?

There are indeed 102 candidates entering vaccine trials. But make no mistake. Vaccine development is challenging. Once human testing begins, the long-shot candidates fade. One bad trial and those vaccine candidates could be gone. Even seemingly sure things can flame out unexpectedly.
So what is the secret to successful vaccine development? Screwups. Scientific discovery relies on screwups more than you imagine. One of the very first vaccine successes was the result of a screwup in the lab of the famous Louis Pasteur.
Pasteur was studying fowl cholera by injecting chickens with live bacteria and recording the fatal progression of their illness. Seems a bit mean. He had instructed an assistant to inject the chickens with a fresh culture of the bacteria before a holiday. The assistant, however, forgot. When the assistant returned a month later (nice holiday!) he gave the chickens a weakened bacterium shot. The chickens, while showing mild signs of the disease, survived. When they were healthy again, Pasteur injected them with fresh bacteria. The chickens did not become ill. Eureka! That screwup was central to our understanding of how vaccines activate the immune system.

So the next time you screw up, remember that screwups are important to science. Remember those chickens, not only saved from cholera death, but precursors of the vaccine technology that has saved countless human lives over the past hundred years.
CQC counsels patience. One hundred vaccine candidates are a great running start. Vaccine scientists are off to the races. All they need now are pipettes and thumbs, a big supply of humans (and some monkeys, not chickens), and a lucky screwup to turn a long shot into a winner.
If shots are on your mind, dance to this classic song. Or attend another contest between Mabel and Olive, called by the famous sportscaster Andrew Cotter.
I am confused about the testing. Some people are still using the nose swabs that take a week; there are also 15-minute tests and antibody tests. Why are there so many options?
As of May 19, 2020.
CQC will try to untangle the testing mess using point-by-point analysis. Point-by-point analysis was developed by scientists for use in hazardously confusing situations like congressional hearings, closing arguments of jury trials, and Project Runway. Point-by-point analysis is a feature of Sun Tzu’s The Art of War. CQC is an update to the AOW. Let’s call it the Art of the Corona Deal (the AOTCD). AOTCD aims for the clarity of a Zen koan.
Point 1. Despite millions of available tests, there are not enough actual tests. Zen masters refer to this type of koan as the “identity of opposites.” Someone wants you to believe testing is widely available, but once you achieve enlightenment, you understand that “available tests” are an illusion. Only governors with their governor superpowers can convert available tests into real testing.
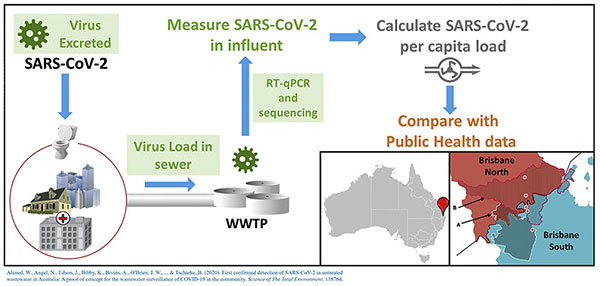
Point 2. You need only remember two tests: the nasal swab test and the blood serum test. Nasal swabs detect the virus in your nose. They check whether your body is making virus and might be contagious now. Whether they take 15 minutes or five days to produce a result, it is all the same. They answer only one question: was your body producing viral particles at the time the swab was in your nose. The blood serum test does not test for virus. It tests for your body’s reaction to virus. It turns out that large amounts of virus end up in your stool too, but let’s not go to that dark place. Sewage is better left for experts in the appropriate handling of feces, also known as either gastroenterologists or public health officials. No fart jokes, please.
So what’s with the fast test? What makes it faster? If you read the press releases and the news articles, you will see that this handy dandy little test kit is a machine that everyone describes as “the size of a toaster.” The corona chef puts a corona swab directly into the machine. When the bell rings, the result pops up. If it doesn’t pop up right away, unplug the machine and use a knife to dig out the result before it burns. Served with butter and marmalade, the coronavirus result is a delightful morning treat.

Worse than burnt toast, the corona toaster/tester can produce false negative results, especially if the swab is not inserted directly into the machine.
Point 3. Bodies make antibodies. Hey, that sounds like the identity of opposites. CQC told you this AOTCD Zen thing would come in handy. Specifically, the human immune system is highly attuned to foreign chemicals that should not be inside the body. The immune system has sentinels like those spidery machines in the Matrix movies or K-9 sniffer beagles at the luggage area at international arrivals — roving T-cells and B-cells that are always on the lookout for something that is not quite right.
If something is amiss, human T-cells call for reinforcements from other T-cells and B-cells. Those cells immediately begin to produce immunoglobulins (Ig, for short). The Igs come in two flavors: IgM and IgG. The Igs latch on to parts of the virus like defensive tackles sacking a quarterback. They harass the virus, slow it down, block it, tackle it, and even commit technical fouls, punching and kicking it in a big sticky pile until it has to be carried off the field.
IgM comes first. Through a process that is poorly understood, the IgM provides temporary protection while the B-cells are still home schooling, learning the exact type of IgG that will best target the invading virus. How long does this take? Well, as the graph below shows, the virus has about a week to run amok before IgM is up and running. Symptoms usually begin around the time IgM arrives. IgM beats up the virus a little and the viral RNA begins to decline. The patient begins to recover just around the time IgG reinforcements arrive. If you have survived the first assault, IgG mops up and then stands guard against any attempts at reinfection. Once IgG gets through with SARS-CoV-2, whatever particles are still shedding from your nose (or stool) are too damaged to harm others.
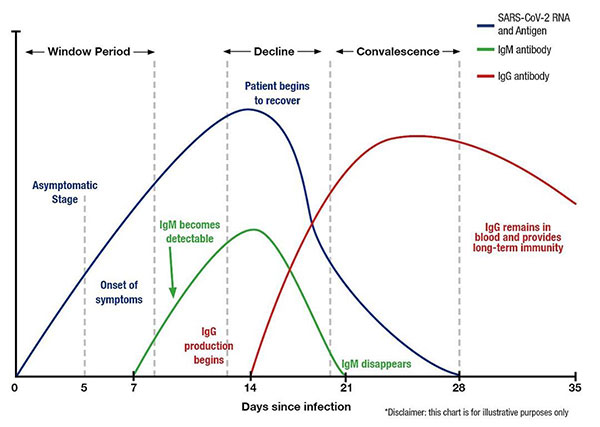
Why not test for IgM? Wouldn’t that give an answer sooner? Maybe, but IgM doesn’t hang around. It may be gone by the time you give a blood sample. That makes testing for IgG the better strategy. But it also means testing too early can produce a false negative. The IgG may not have ramped up yet. Of course, you could always get a second test a week later to be sure. That is, if testing is available and if it is real.
Once it is real, antibody testing will be very useful. It will confirm that someone was exposed to the virus. And a positive test may mean they are immune to future infection and cannot pass the virus to other people.
In any case, be on the lookout for bad appliances. Device manufacturers may tell you their toaster is greatest thing since sliced bread, but the proof is in the toast.
I have a sour view of standardized testing. We spent a fortune for my high school juniors to prepare for PSATs, SATs, and ACTs while eating PB&Js. Now all we hear is “testing, testing, testing” before the economy can reopen. Is this a scam?
As of May 14, 2020.
Desperation is powerful. Until recently, desperation was about people trying to gain admission for their children to the college of their choice. Even celebrities were breaking the bank (and the law). Desperation can drive people to seek a better life in the United States. It can spur people to get a job, or two jobs, or even three jobs.
But nothing beats the desperation that motivates innovation. L. Ron Hubbard famously wrote, “Ideas and not battles mark the forward progress of mankind.” Who is L. Ron Hubbard? CQC will refer you to Tom Cruise, but give him a moment while he finishes his latest impossible task.

Let’s have a quiz while we wait for Tom. You believe standardized testing is a A) a scam, B) boring, C) overpriced, or D) all of the above.
Most of you picked D, probably because you recalled CQC’s sage advice that “all of the above” is nearly always the best answer on a medical board exam. As often happens, D is the correct answer.
But not all testing is bad, especially in a pandemic when what we really need is testing, testing, testing. Let me explain why.
Innovation is the soul of America. Desperation and innovation come together in the unique art form known as the Shark Tank! For this shark tank to work, we need a panel of judges. These fine panelists will determine whether the innovative testing ideas are worthy of $1 billion in taxpayer money.

Fortunately the judges only need to consider three different testing options: PCR, antigen testing, and antibody testing.
The primary test for coronavirus is a polymerase chain reaction or PCR test. The polymerase is an enzyme that reads ribonucleic acid (RNA) strands. Used in this way it can amplify millions of copies of a fragment of SARS-CoV-2 genetic material. But it only amplifies if the SARS-CoV-2 sequence is present. Don’t worry, it only amplifies a fragment. No danger. But as the picture shows, that swab goes way deep in the nose!!
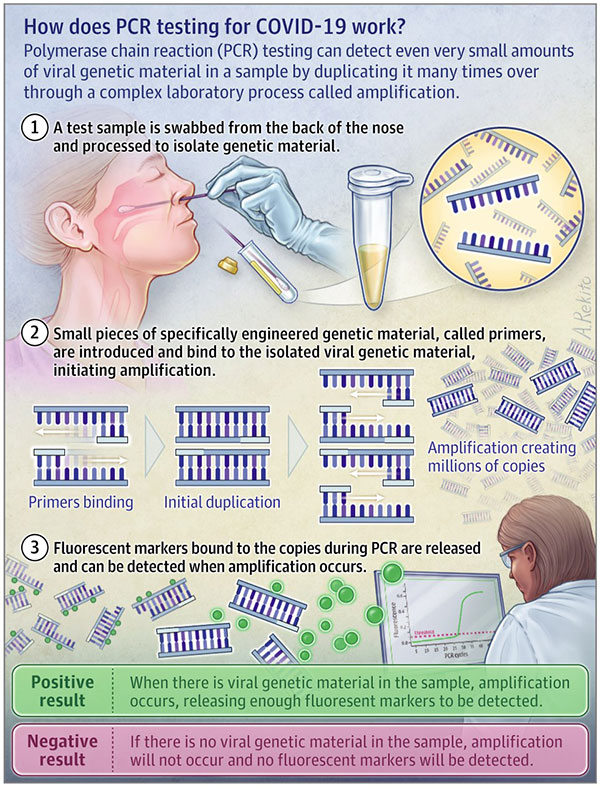
For coronavirus, it is specifically RT-PCR testing. The RT stands for reverse transcriptase. Why reverse? Normally, the cells of your body use DNA to make (or transcribe) new copies of RNA. Transcriptase is the little enzyme that does this. But since SARS-CoV-2 is an RNA virus, the copying is backward from RNA to DNA. Hence “reverse” transcription that translates a single copy of RNA to millions of copies of DNA. Those mirror-image DNA copies make your COVID-19 test light up.
But RT-PCR testing is slow, ponderous, and mentally and physically taxing. Each test requires a special machine with a special process and hours of chemical reactions. So scientists are looking at a faster alternative: antigen testing. You may have heard rumors about speed — less than 15 minutes!
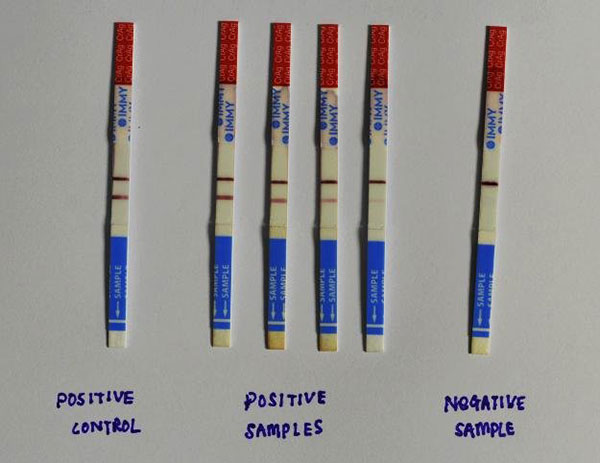
“The test works by taking a nasal swab from a patient and introducing that sample into a solution . . . exposed to one end of a series of paper strips. The strips contain artificial antibodies specially designed to bind to coronavirus antigens. As the solution moves up the strip, any antigens that are present will bind to it and give a visual readout. The whole thing takes less than 30 minutes, and it doesn’t require special equipment or training.” If you ever took a rapid strep test, that was an antigen test.
That sounds cool. Where can we get these magic strips?
“I would say antigen testing for COVID-19 would be a total game changer, except for one aspect: it won’t work,” says Alan Wells, the medical director of clinical laboratories at the University of Pittsburgh Medical Center.
Scientists can be such downers.
Why not? “An antigen test for a bacterial disease like strep works well. But respiratory viruses like coronavirus are a whole other game. For example, the antigen test for influenza has a decent sensitivity of about 70 percent to 80 percent when run properly on a good nasal swab — but only for children, because the quantity of the virus in children is typically much higher than in adults. When you use the same tests on adults, the sensitivity drops to less than 50 percent. This is observed across the board for respiratory viruses. In a PCR test, the viral genetic material is amplified so that it’s easier to identify signs of COVID-19. There’s no amplification of viral proteins in an antigen test. Either the test detects them in the sample or it doesn’t.” Sure enough, the FDA just approved the first antigen test for COVID-19! Sensitivity? 85 percent. Out of 100 people with COVID-19, 15 of them will have false negative test results. They actually have COVID-19, but the test clears them.
Poor sensitivity sounds bad. Maybe an indication for sensitivity training. By the way, people keep talking about sensitivity and specificity. What is sensitivity when it comes to a virus?
Glad you asked. In medical diagnosis, test sensitivity is the ability of a test to correctly identify those with the disease (true positive rate), whereas test specificity is the ability of the test to correctly identify those without the disease (true negative rate). These are inherent properties of a test.
In general, people worry most about false positives and false negatives, but numbers of false positives and false negatives depend not just on the test, but also on the prevalence or frequency of the disease in the population. Let’s say you have a test that looks in CQC’s wallet for a $20 bill. If you your test comes up negative, that is likely a false negative because there is always at least one $20 bill. It’s there every time CQC is looking for a single to tip someone. Now do a test that looks for $1,000 bill. If you get a positive result, that is called a serious surprise. Hand back the wallet pronto! The prevalence of $1,000 bills in the wallet is zero. Always has been and always will. So CQC knows that the positive $1,000 bill test result will always be a false positive. No calculation needed.
Speaking of empty wallets, you will be pleased to know that Felicity Huffman’s daughter just got admitted to a top school with a great drama program. Prisoner Huffman was released after 11 days. So that must be one big happy stay-at-home family household again. And what a relief for the rest of us to focus on something other than coronavirus for 10 seconds.
Since we’re all stuck in our homes, with minimal interaction with others (and others’ germs), I was curious if we’ll be more susceptible to other colds and flus when we are able to move around a bit more freely. I was also wondering about next year’s flu season. Assuming this year is not that bad because we’re all under house arrest, will next year’s flu be much worse?
As of May 12, 2020.
Comparing flu seasons is an American pastime and also a scientific project involving lots of data, sluggish reporting, later adjustments, and this annual graph.
This graph uses data from death certificates, surveillance clinics, and hospital testing to create a picture of the percent of all deaths each week that were due to pneumonia and influenza. Why both? Because most, but not all, deaths from influenza are a result of pneumonia. The graph covers five seasons over five years numbering the weeks of the year.
Every winter, the percentage of deaths due to influenza rises, and then it falls again in the spring. The lower black wavy line is the seasonal baseline. The upper black line is what defines an “epidemic” of deaths. Those are estimated based on historical patterns, sort of like the average expected high and low temperature each month. You might have checked a weather planner before your vacation. This graph is sort of the flu death planning equivalent.
The red line represents the actual percentage of deaths due to influenza and pneumonia. You can see at the left that the 2015 flu season was average. The red line stayed within the black lines. 2016 was a little worse, but not bad. Based on that red peak, 2017 was not a great year, with many more deaths than usual. 2018 settled down a bit. 2020 was . . . Holy cow!! What on earth happened in 2020?
We now know that the excess deaths due to pneumonia were not flu deaths, but new COVID-19 deaths. One reason epidemiologists didn’t see COVID-19 coming? It slipped into the U.S. under cover of the flu season. Health departments started to see a surge in pneumonia deaths, but thought it was just another one of those especially late and bad flu seasons. Then the sh*t really hit the fan.
This graph is going to be useful going forward. But not in the way we usually expect. First, the red line is going to stay much higher as those excess deaths pile up. Even as we physically distance in some states, the red line is going to stay high. The true challenge arrives when we begin to emerge from our homes. We don’t know when or how much or for how long, but as we do start to move around again, the virus will spread. Maybe in a controlled way, but it will spread enough to keep that red line high, probably for the rest of this year and into the next.
And the flu and other germs also will resume spreading. But they will spread less than they used to because we have learned so many new tricks: physical distancing, hand washing, face coverings, and cleaning stuff all the time. Those new tricks mean we can worry less about the “good old pathogens” that cause what are known affectionately as “the sniffles.”
But don’t worry about losing your edge battling viruses. We all have memory B cells. I bet you didn’t know you had memory B cells, but you do. Their purpose is to fight viruses. Memory B cells are like the national guard reserve, except that the reserve is made up of librarians. You have approximately 10 billion of these handy librarian soldiers in your stockpile. Each one remembers a specific viral marker. As soon as that marker appears anywhere in the body, that B cell is tipped off, triggered, and multiplies, swarming in with antibodies to destroy the intruding virus. B cells are different from T cells.
B cells are like the soldiers described by Henry V, in Shakespeare’s Henry V (homeschooling tip: learn this soliloquy):
“I see you stand like greyhounds in the slips,
Straining upon the start. The game’s afoot”
Unfortunately, we don’t have B cells that remember this novel coronavirus. Our B cells do remember other coronaviruses though, which might help. This is speculation, but those people who have mild or asymptomatic COVID-19 infections? Some of their B cells may be especially quick to jump in and readily trained to start killing virus right away. Once trained, those B cells will go back to the librarian national reserve barracks where they may be with you for decades, waiting for no-longer-novel coronavirus to return.
The good news is that our memory B cells don’t go away just because we are stuck at home. When we get back outside our houses into the Zoom-free environment where we can start sharing viruses again, our memory B cells will be there at the ready, in the slips, ready to race. You need not worry that staying indoors will make them any less effective. They don’t need CrossFit or yoga or running or free weights to stay sharp.
About that future flu season? If I were CDC Director Robert Redfield, I wouldn’t worry about next year’s flu season. You would be taking your eye off the ball in two ways. First, whatever damage flu season does will be tiny in comparison to the ongoing COVID-19 battle. Remember that red line above? CDC should be so lucky to think that flu season may interfere in the COVID-19 assault. And second, you are driving in fog right now. When driving in fog at night, you don’t focus on some phantom a mile down the road. You can’t possibly see that. Instead you focus on the hazards that are right in front of your headlights.
Today’s question is from a younger reader: If mosquitoes carry viruses and diseases and give them to us when they bite us, can they give us coronavirus?
As of May 7, 2020.
This tender youth has an uncanny talent for looking ahead to where the real threats lie. Send this one to statistical modeling school! The rest of us are already dreaming about the lazy days of summer and those long outdoor dinner picnics with the cousins at sunset when we gather around to . . . RUN AWAY FROM MOSQUITOES!!!

One thing about coronavirus — it can make you nostalgic for the strangest experiences. CQC would eagerly jump at the opportunity to sit around the picnic table offering a sumptuous meal for those little bloodsuckers. But then the dance music stops and we wonder whether coronavirus is also going to invade the picnic. Heck, maybe ants carry it. What about bats? They carry rabies. And before we know it, we’re back to our usual state of coronavirus panic.
But good news on mosquitoes and coronavirus. They can’t transmit it. How do we know? The World Health Organization and independent experts say such transmission is virtually impossible. Joseph Conlon, a former U.S. Navy entomologist and technical adviser for the American Mosquito Control Association, said the possibility of mosquito transmission of the coronavirus is “nil.” Nil is not a word that experts use lightly. When scientists say “nil” they mean zero, less than zero, zilch.
That doesn’t mean the conspiracy theories aren’t spreading. Disinformation is rampant. It turns out the U.S. Department of Agriculture doesn’t believe WHO or independent experts. Are you surprised? USDA is said to be studying whether the novel coronavirus can be spread by mosquitoes. USDA won’t say how much they are investing in this attempt to confirm that nil means nil.
Getting back to reality, mosquitoes are zoonotic transmitters (animals that carry infectious diseases to humans). As most people know, they carry malaria. Fewer people know they carry flaviviruses. And now you are learning they don’t carry coronaviruses. Why? It turns out only certain types of viruses can make it through the digestive tract of a mosquito. It takes a special virus to get through that complicated maze. So what about flaviviruses? What are they? Should we be worried about them?
You have heard about one famous flavivirus: Zika! If you are old enough (old enough to read a children’s guide to zoonotic viral transmission) you will remember the Zika panic of 2016. Zika was puttering along in Africa for decades, but in 2016 a major outbreak started in Latin America, carried by mosquitoes. This was scary stuff. Some pregnant women infected by Zika had children with serious neurologic problems. It seemed like this disease would grow and spread into the United States. Cases began to appear in the south where the mosquito is found. Climate change was going to bring the mosquitoes north. Everyone was gearing up vaccine development, drugs, environmental control, mosquito control, tennis court control, picnic control, beach control, and of course southern border control.
And then, a miracle. One year later, it just stopped. Went away. Nil.
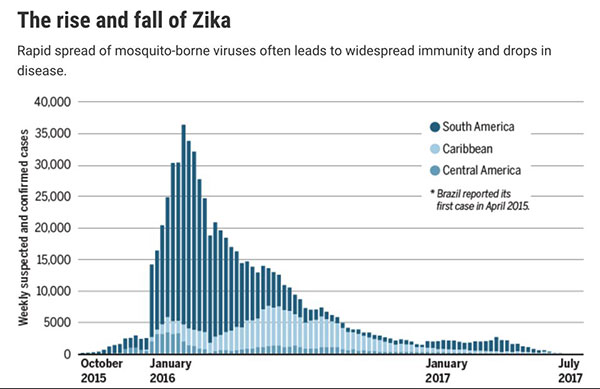
Image credit: J. You/Science (Graphic); Pan American Health Organization/World Health Organization (Data)
You can see that same petering out here. Vaccine testing had to stop. Not enough cases to prevent. What happened? For the answer, this tale is an interesting weekend read. A hint: the answer rhymes with “turd in unity.” (No, that is not the name of an '80s punk band.)
The report includes an oddly familiar cast of characters: “Anthony Fauci, director of the U.S. National Institute of Allergy and Infectious Diseases in Bethesda, Maryland, says he’s not ‘entirely surprised’ about the precipitous drop, ‘but I am impressed by how steep it has been.” You will also be reintroduced to that Imperial College Modeler God, Neil Ferguson.
Neil Ferguson nailed it on Zika. In 2016, his team’s model said Zika would be over by 2018. Boom! Nailed it. But there was a caveat: “I think it’s highly unlikely we will see any resumption of significant transmission for at least a decade.”
Um, okay. We have five years to get past coronavirus before we have to deal with Zika again. But let’s celebrate the defeat of Zika by dancing once more to Loleatta Holloway’s “Runaway!” Don’t worry about the mosquitoes! We’ll be staying inside this summer. The mosquitoes will starve. By July they will have gone the way of Zika!
We keep hearing how prevalent and infectious the coronavirus is. Up to 80 percent of people might contract COVID-19 before this is all over. With more than 300,000 cases , it seems like all New Yorkers likely know someone who has had the virus. But then we also hear that if you have symptoms, they are still more likely to be caused by the common cold, allergies, or even seasonal flu. I’m having trouble squaring those two outlooks. How can both be true?
As of May 5, 2020.
Fabulous question with several lines of evidence available to answer it. First, the Census Bureau estimates there are 20 million New Yorkers (minus the ones who fled the state last month). If you do the math, more than one of every 100 New Yorkers has a confirmed case of COVID-19. That number is probably higher in New York City, where most of New York’s cases have appeared. Do you know 100 New York residents? If so, you may very well know at least one person who had COVID-19, especially if your friends live in NYC. And if you believe in Kevin Bacon’s six feet of separation approach (I believe this used to be six degrees), you know someone who knows many someones who know an unbelievably large number of COVID-19-infected New Yorkers. That’s how spread and social networks work.
Speaking of networking, CQC spotted Kevin Bacon at Café Luxembourg last year. What CQC would not give for a Luxemburger and fries right now, with added Bacon. Gin and whiskey at home are okay, but stay-at-home orders mean no celebrity sightings and no Luxemburgers.

How about those asymptomatic cases — the ordinary noncelebrity people you know, but Kevin Bacon does not — who might have become infected and didn’t know it? This week Iceland weighed in with some useful data on COVID-19. Iceland tested a lot of people. Easily done because only 364,000 people live in Iceland. That’s half the population of South Dakota. But unlike South Dakota, Iceland is exposed to the world — 7 million travelers pass through Reykjavik each year. Iceland’s first cases came from overseas, then they spread among the Icelanders. Less than 1 percent of people tested positive. But the relationship between symptoms and infection was interesting: two of five people with a positive test result had no symptoms at the time of the test. That is the group that can transmit the virus even without symptoms. But researchers also found one of three people with symptoms of COVID-19 had a negative test. Their symptoms were due to some other cause.
But Iceland is not New York. Iceland did shutdown and testing early so they have fewer cases. And Reykjavikers are not New Yorkers. So with all that COVID-19 circulating in New York, how can cold and flu symptoms not be coronavirus? For that we turn to the common cold. The common cold is a viral infection of the upper respiratory tract. Coronaviruses are not alone in causing the common cold. The most commonly implicated virus is a rhinovirus. Frequently more than one virus is present. In total, more than 200 viral types are associated with colds.
So the common cold arises from 200 highly contagious viruses circulating in the population all the time. The average adult has two to four colds per year. A rich menu of 200 viral options is available to you for catching those colds. But if you want COVID-19 this year, you have only one viral option — SARS-CoV-2. That’s right, one per customer. So COVID-19 is fearsome and large in our imagination, like that tall bully on the playground. But there was only one big bully. If someone was stealing your lunch money, chances are it was one of those other petty criminals you called classmates. Same with the viruses. CQC doesn’t mean to disappoint, but your symptoms are still more likely to be the common cold.
SARS-CoV-2 may be a one-off, but it is truly accomplished. It managed to shut down the global economy. It is like the genius composer Beethoven, who famously said, “There are many princes, but there is only one Beethoven!”
The majority of coronavirus cases in NYC were traceable to the strains seen in Europe, and likely resulted largely from infected patients who flew in from Europe, genome scientists say. They can say this with confidence because the SARS-CoV-2 consists of about 30,000 genetic bases, or letters, and it “mutates about twice a month.” Didn’t CQC say there wasn’t a lot of evidence that the virus was mutating? When would a “minor mutation” (or a collection of them) be large enough to warrant additional concern?
As of April 30, 2020.
We recently celebrated the 50th anniversary of the rescue of the Apollo 13 crew. What better time to recall that in that quaint crisis of yore, all Mission Control had to do was to calculate a new orbit for the spacecraft, fire up a few thrusters, and the crew was back on course toward earth.

Men in Mission Control in Houston watch as the astronauts of the Apollo 13 mission are recovered by the USS Iwo Jima in the South Pacific on April 17, 1970. Apollo 13 was damaged during flight and was forced to make an emergency return.
That’s rocket science!!
But biology is not rocket science. Rocket science has the laws of physics. Biology has the laws of . . . replication? Virology seems like it should be much simpler. A coat of proteins covers a strand of DNA (or RNA). That strand of DNA or RNA is like a ticker tape that can be read as the chemical instruction code for life. What’s a ticker tape, you say? Well, it’s like the groove in a vinyl record. It contains the musical instructions read by a stylus dragged through the groove on a turntable.
Way too analog, you say. How about a digital analogy? Maybe Morse code? Or that weird spelling label tool some of us used in elementary school to mark our cubbies?

You used to punch a code on a piece of plastic tape. Imagine the virus is a really long label looking for a cubby to attach itself to.
Seems simple, right? Wrong. Viruses come in many different flavors. Fortunately, this paper contains a handy illustration. Coronavirus is an RNA virus (the lemon-flavored circle). For reference, you and CQC are the “higher eukaryotes” referenced in the blueberry-flavored circle to the right side of the picture. We have the biggest genome size (the longest punch label tape) — larger than all the other living things. But we higher eukaryotes don’t usually brag about genome size. You can see that RNA viruses (the lemon-flavored circle) are simpler — they have a smaller genome size.
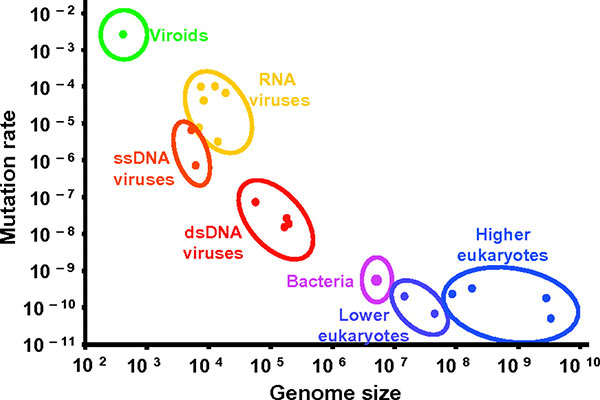
Relationship between mutation rate per nucleotide site and genome size for different genomic systems including viruses. Reproduced from: Gago S, Elena SF, Flores R, Sanjuán R (2009) Extremely high mutation rate of a hammerhead viroid. Science 323:1308.
But as you inspect this, you see that RNA viruses have a higher mutation rate than most other living things. So if RNA viruses mutate so easily and genome scientists can tell where a mutation came from, how is it possible to say that coronavirus is a dud when it comes to mutation?
Well, the problem with mutations is that they are nearly always lethal — to the virus. Especially for coronavirus, the key to replication success is to unlock a specific protein on the surface of a cell inside a human nose. The virus literally IS a key. One mutation makes the key inoperable on that particular lock. Remember the last time you lost your key and tried to get back into your apartment? You called a locksmith. But coronavirus can’t call a locksmith. It’s game over for coronavirus.
CQC is saying that coronavirus can mutate like crazy, but it can only tolerate a limited number of those mutations — the ones that don’t affect its ability to unlock those cells in your nose.
Those few mutations that don’t kill the virus provide just enough variety to enable virology mission control to track the virus across the planet. That’s how we know most of the coronavirus came to the U.S. from Europe, and some of it came from China.
Don’t get the wrong idea about mutation. Mutation is good. We higher eukaryotes need mutation and we can tolerate a lot of it. The more complex the DNA, the more mutations an organism can tolerate. Mutations, slow and steady, are what provides all the beautiful variety and diversity of our biological world.

It may not be rocket science, but virologists have a more colorful cast of characters. Some people are hoping the coronavirus will mutate its way out of our lives altogether. Virologists know it is not that simple, but they won’t rule it out. Pandemics do not follow the laws of physics. CQC will drink to that!
Why aren’t we doing more to identify infected people and how can we build a registry and use the advanced data technology available at universities or companies like Google as part of the arsenal in fighting COVID-19?
As of April 28, 2020.
This question poses two scientific dilemmas: action (“Why aren’t we doing more?”) and a technology (“Could advanced technology be brought to bear on the weird hole we somehow find ourselves in?”).
As Americans, we place our faith in innovation. Jump to the technological solution. Testing? We have the technology. Maybe it was slow to be deployed, but the machines are there. Then, why are we still testing fewer than 250,000 a day in a country of 330 million when 2 million tests per day are needed? Turns out it’s not technology at all, unless you consider cotton swabs a miraculous technical achievement. And those chemical reagents that make the tests flash green or red. We lack stuff that is idiotically simple to make if you’re a manufacturer but can’t be knit or turned out on our sewing machines. Somehow this crucial stuff is just not worth making if you are an American manufacturer. Maybe the price gouging hasn’t gone high enough? The U.S. market doesn’t seem interested in supplying it to us mere humans right now. Ask an economist if you want to understand supply chain breakdowns.
And apps. Google and Apple are teaming up to teach your smartphone how to determine whether it got too close to another smartphone in the unlucky hands of someone who tested positive for COVID-19 virus. Pretty cool tech surveillance gear!
Exposed? You get an alert! Tag, you’re it! You stew for 14 days in isolation wondering which of those passing friends and strangers was spewing a cloud of SARS-CoV-2. Was it the grocery store person bagging your groceries for Amazon, or the delivery guy from Amazon that lingered outside your door a little too long, or that youthful and reckless runner with the athletic stride of an Amazon? Meanwhile, everyone whose smartphone got too close to yours is now stewing. It’s a big data research project come true. And if big data can’t solve things, what hope is there for little data like you and CQC?
Wait a minute, you say. The smartphone thing only works if your test results are available to the phone. But almost no one can get tested at this point unless they are in a hospital. And if you go near a hospital — automatic smartphone alert! You didn’t need a sophisticated algorithm to know that walking into a hospital will trigger the COVID alarm on your smartphone. Who goes to a hospital now unless they work there, have COVID-19, or are about to give birth? How does the app help? If nobody can get tested and input the result, that app thing is a hill of beans.
We come to the sad conclusion: the technology wasn’t as cool as it sounded. Plus, when it comes to problem-solving, nothing beats simple motivation and simple solutions. For motivation, you might think that the loss of nearly as many Americans each day, day after day, as we lost on a single day in 2001 might prompt some type of useful federal response.
But do not despair in the midst of unnecessary death. Nurses and doctors learn early in their careers that one can be enveloped in human suffering, tragedy, grief, and death for hours on end. Then in an instant, they can step outside the doors of the hospital, where the searing beauty of the natural world can be blinding, especially in the spring.

The natural world carries on without us. What they didn’t teach in nursing or medical school was how to react to an urban landscape devoid of people. Or a mighty river flowing past the greatest city on earth without a boat in sight — not even a lifeboat beating against the current, borne back ceaselessly into the past.
Does the virus affect men more than women? Are we in a “war” where we risk losing our middle-aged men?
As of April 28, 2020.
On your question about the risk of losing middle-aged men, what leads you to believe they aren’t already lost? Many a middle-aged man muses about how life might have turned out if it weren’t for those awful choices along the way: the one that got away, the one that didn’t get away, not preparing for that once-in-a-century disease pandemic that seemed so far away . . . “All my troubles seemed so far away,” the Beatles sang.
Does the virus affect men more than women? Good question. One recently published study says “maybe”: “Although sex-disaggregated data for COVID-19 show equal numbers of cases between men and women so far, there seem to be sex differences in mortality and vulnerability to the disease.” Perfect scientific writing. Tell you there’s a difference but don’t spoil the punch line. Is this men or women? “Emerging evidence suggests that more men than women are dying, potentially due to sex-based immunological or gendered differences, such as patterns and prevalence of smoking.” Well, there you have it.
Except in a pandemic, a study from one month ago could be completely out of date. Let’s go back to the literature. Here’s a case series study. Finding? “In the case series, men tend to be more serious than women.” In the pigsty of scientific methods, case series studies are considered the runt of the litter. That is, really weak. Never believe a case series result. Men are definitely not more serious than women.
One more dip into the sty turns up a larger case series of 1,500 people living in China. Still a methodological runt, even with a larger sample size. More men than women were hospitalized. Sounds promising. But after controlling for other factors, gender differences were the result of other factors like other diseases. In plain English, men are sicker and more likely to have a bad outcome. But the jury is still out since there are too few rigorous studies. Bah!
The lesson is to admit what is unknown. And while science is working on the answer, sports can fill the void. Some reruns are worth watching over and over again — like the U.S. women’s national soccer team victories.

If you missed filling out your Final Four bracket last month, you can still fill out your census! It’s not a bracket, but you can’t lose either. You will be supporting your state’s political power. Your state needs YOU as it fights the COVID war.
If a person transfers virus particles from hands to face, how do they migrate to mucous membranes in eyes, nose, mouth? What moves them?
As of April 23, 2020.
When we last left Achilles, his friend Patroclus lay slain. Grief weighed heavily on him. So heavily, that he challenged Hector to a 1:1 meeting (not on Zoom) outside the walls of Troy. It ended badly for Hector. But the Trojans still had those insurmountable walls, so the war went on. Eventually, the Greeks realized their corporate initiative was futile. Only then did the innovator Odysseus come up with a solution. The Greeks boarded their ships and sailed out of sight, leaving behind a large wooden horse. The Trojans mistook it for a parting gift. They unwittingly dragged the wooden horse and its secret cargo of hidden Greek soldiers right through the front gates of their impregnable fortress. That night, the Greeks emerged from the belly of the horse, opened the gates of Troy and livestreamed their returned comrades. The end of Troy was under way.
Why is CQC going on about Troy? Because the biological defenses of the human body are like the walls of Troy. As coach Normal Dale says in the 1986 film Hoosiers: “I’ve seen you guys can shoot but there’s more to the game than shooting. There’s fundamentals and defense.”

In a nutshell (or a wooden horse), SARS-CoV-2 has to get past your mask, but like the Greeks, it faces other formidable defenses. Add to that, viruses are lazy. They have no way of moving without help.
To answer your question, CQC turns to physiology and anatomy — just two of the available defensive strategies — and describes how the virus tricks you into opening the gates. Let’s start with the outer chamber of your respiratory system: the nasopharynx — a.k.a. your nose. Your hands are like the wooden horse. Your face, the high walls of Troy. First, thousands (or millions) of viral particles are ferried by your unwashed hands to the skin of your face. Once there, they have to wait patiently for you to do what the Trojans did. Unwittingly, you touch your face again, aerosolizing the virus. As you do that you yawn, cough, or sneeze. Each of those three actions ends with a strong inhalation. The airflow pulls the aerosolized virus through your nose. Bingo, the viral Navy SEAL team has made it into the mudroom of your fortress — the nasal cavity.
But that was the easy part because you failed to wash your hands! It is difficult to fully appreciate the many barriers ahead for the SARS-CoV-2 Navy SEALs. They have a special key that enables them to latch on to a protein called ACE2 on the surface of the cells of your nasal mucous membrane. Getting the key to the lock is not child’s play. First, the SEALs are confronted with sneezing. Just as they rode in on a puff of air, one sneeze and they are expelled back to the outside. Second, mucous. Tons of it in allergy season. Viruses get trapped in mucous. It is quicksand for viruses. And it contains chemicals that can degrade viruses. In the diagram you see turbinates, which look like the air baffles on a sports car. Those baffles create air turbulence in your nasal cavity that filter and crash the viral particles into the mucus.
Behind the turbinates there are adenoids, tonsils, and what is called Waldeyer’s ring. This is the immune response crisis center — sort of a 911 for the immune system. Once the virus is detected there, white blood cells come racing like a fire crew.
Beyond Waldeyer’s ring, heading around the bend to the lungs? More coughing and more mucous. But that’s not the end. In the bronchioles, the tubes leading to the lungs, the virus must face the cilia!
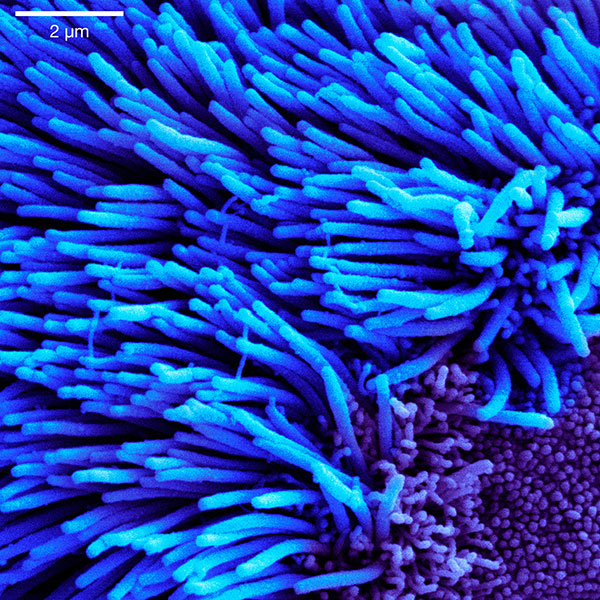
These special cells line the bronchioles. They beat back and forth in a regular rhythm like seaweed, creating another trap for viruses and an escalator that pushes mucous, viruses, and other crud up and out of the bronchioles before they ever reach the lungs.
That is just the briefest of introductions to only a few of the complex defenses that human biological evolution has created to keep SARS-CoV-2 out of your living room. If you want the ultimate biological defensive machine, honed to perfection by weeks of stay-at-home shutdown, you have to check out this cool cat.
Public health warnings say it’s OK for me to walk my dog, as long as I stay six feet away from other people. I’ve read it’s unlikely that dogs can harbor the coronavirus. But what about people petting my dog? (She’s cute, people want to.) Is that dangerous to the other person or to me? What about my dog interacting with other dogs? (She likes to play, even at the end of a leash.) I’m embarrassed to ask such questions, but one authority said, “If you think you’re overreacting, you’re probably doing the right thing.” So, I worry about the dog.
As of April 21, 2020
So, what about pets? Can pets catch COVID-19? Should they be tested? Anecdotes from Asia raised the question about cats. Hard evidence is limited one way or the other, though it is beginning to emerge. The first animal tests were recently developed, but they are not yet widely available. (Sound familiar?) That said, testing may not be indicated for pets. Think about it. More than 1,000,000 cases of COVID-19 worldwide and 70,000 deaths. You would guess a lot of pets have been exposed to owners’ coughing, sneezing, and spitting SARS-CoV-2. Yet the global media, always on the hunt for animal stories, have turned up only a couple of infected cats and an unlucky Pomeranian in Hong Kong. In the U.S. alone, there are 150 million cats and dogs. That’s nearly one-half of a pet for each American. With over 800,000 COVID-19 cases in the U.S., half a pet per American should yield 400,000 COVID-exposed cats and dogs, on average. Yet there are no reports of sick half-pets in the U.S.
This is good, not just because we love our pets but also, they are really terrible at physical distancing. You’ve seen the nose-to-nose, nose-to-butt, rolling-together-in-the-grass stuff.

CQC wonders how dogs survive. They must be especially good at fighting microbes. But what if they just have good armor? Could they keep the virus on their fur? Their owner coughs on their dog, who nuzzles with your dog, then you nuzzle, and bingo — COVID-19! That’s so-called fomite transmission. We know fomites are a rare but real transmission risk. That’s why we wipe everything in sight now. One expert says treat your pets like you treat yourselves. “If you’re sick, restrict your access to your pet as much as you can,” she says. “When you walk your dog, stay six feet away from other animals. Don’t pet other people’s dogs. Always wash your hands,” she says. “It’s really important that people don’t panic.” It sounds like your caution is warranted as long as you don’t panic.
Scientists use the term zoonosis to refer to human diseases that involve animals. Despite names like “swine flu” and “avian flu,” viral pandemics tend to afflict only one species at a time. Others are bystanders. Humans are the preferred host for SARS-CoV-2. CQC was about to write that animals have little to worry about. But then an anecdote showed up. Scientists really dislike anecdotes. They are like the aunt who calls with juicy and probably false gossip just as you are settling in to watch a movie. This anecdote? The tiger thing. Not the Tiger King. (Fire up the popcorn maker!) Not Tiger Woods. (Does anyone watch golf reruns?) The Malayan Tiger in the Bronx Zoo.

This poor Bronx tiger may be the first known case of human-to-animal transmission of SARS-CoV-2. How unlucky. Here you are, a Tiger in the Bronx, when your baseball team is located in Detroit. You probably are subjected to drunk fans showering coronavirus-laden Bronx cheers on you from the Yankee Stadium bleachers. And now you have COVID-19. And stay-at-home means living in a zoo (that last part is familiar to families with children).
Tiger anecdote aside, for most animals, humans are not a disease threat. But, as we are looking out for the animals, the animal kingdom is worried about us. This bear was concerned enough to look in. Are we okay?

No problem, bear. Just another day at the office, signing into another Zoom conference or classroom, waiting for the COVID-19 wave to break.
We older people are finding that some people, particularly younger, healthy ones, aren’t considerate in adhering to social distancing. Are there different distances that should be adhered to depending on the situation? For instance, a jogger came around a corner from behind me when I was sneaking out with my garbage. She went past with about a three- to four-foot distance, heavily huffing and puffing. Shouldn’t a greater than six-foot distance be practiced in this situation?
As of April 16, 2020
CQC understands your impatience with young people. They are sure they have health and beauty. They believe they will live forever. The rest of us know better, especially about the living forever part. But patience is a virtue, especially when faced with young people. Good time to revisit Homer’s Iliad, that famous war dispatch from the 10th year of the war between the Greeks and the Trojans. The Greek commander Agamemnon became impatient with the young Achilles. Agamemnon stole Achilles’s slave Briseis. In retribution, Achilles sulked in his tent and refused to fight on the field of battle. As the Greeks began to lose, his close friend Patroclus became impatient and joined the fight wearing Achilles’s armor. Patroclus was quickly slain. In the end, the Greeks won, but nothing happy came of it. Not for Agamemnon, not for Patroclus, and not for Achilles. Impatience is like gasoline on the bonfire of tragedy.
But the core of your question is more meteorological. Why does distance matter? See the crude scientific diagram below. A review of aerosol transmission reveals that viruses have many ways of Dancing with the Stars from an infected person to a susceptible one. Don’t ask CQC why that infected person in the middle is coughing on what may be a laptop. Or why these people lack bodies. Odd shortcuts are part and parcel of science illustrations.
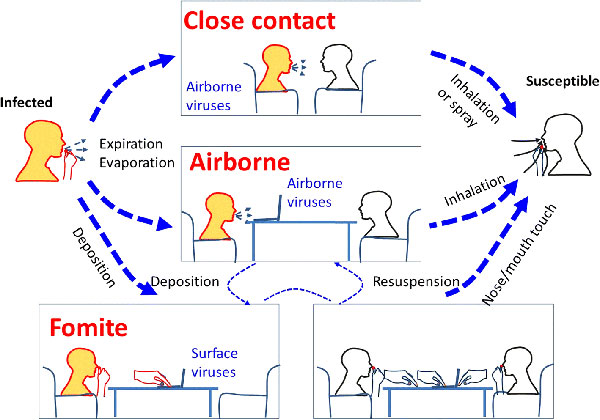
Recognition of aerosol transmission of infectious agents: A commentary - Scientific Figure on ResearchGate. Available from: https://www.researchgate.net/figure/An-illustration-of-various-possible-transmission-routes-of-respiratory-infection-between_fig1_330770553 [accessed 16 Apr. 2020]
A few key points from this review and other sources:
- A violent sneeze can propel a virus up to 26 feet!
- Most normal huffing and puffing probably gets to about six feet.
- Some talkers inadvertently spit more than others. They call it bluster for a reason!
- Wind speed and direction really affect the distance of dispersion.
Every Boston Red Sox fan watching a towering pop fly heading toward Fenway Park’s notorious Green Monster knows that distance, wind speed, and direction make the difference between a homer, a wall-ball double, or an out. Baseball is very sensitive to weather.

The California Angels meet the Boston Red Sox in a game at Fenway Park on August 17, 1996. Courtesy: WikiCommons.
What goes for a baseball, mostly goes for SARS-CoV-2. Track the invisible virus ball and try to plot where it lands. Everyone should be wary of wind. Slipstreams are especially treacherous right now. What’s a slipstream, you ask? One definition is “an assisting force regarded as drawing something along behind something else.” Ever driven behind a truck on the highway? That wobbling you feel is a slipstream. Or, used in a sentence: “When the U.S. economy booms, the rest of the world is pulled along in the slipstream.” Maybe not the best example right now.
Anyway, to avoid COVID-19 while outdoors, consult a wind vane at all times. Those joggers who menace unsuspecting seniors holding trash bags should pay close attention to distance, wind speed, and direction.

The rules you propose make sense. Here is another one. If you are downwind of a blusterer, hold your breath and don’t exhale until you are out of range.
You could also follow the friendly advice of Albert Camus: “Don’t walk behind me, I may not lead. Don’t walk in front of me, I may not follow. Just walk beside me and be my friend.” As with many quotes attributed to famous writers, there is no evidence that Camus wrote or said these words. Fact-checking is an important role of science, especially when a saying seems too cute or tailor-made for an inspirational greeting card.
Having an appreciation for distance, wind speed, and wind direction is key to the war on coronavirus. Getting others to appreciate it seems eminently reasonable. (Like getting governors to protect the citizens of their states with stay-at-home orders or expanded Medicaid insurance.) You have a right to be angry if people of any age don’t seem able to learn the obvious.
But in a pandemic war, patience with others is key to victory. Patience is needed because war involves waiting in the same trench for a while. The war on Troy lasted 10 years. The war in Afghanistan has lasted 17 years and counting. The war on drugs — who knows? Even the narcotraffickers have lost count. Soldiers will tell you that war is about waiting.
And where better to wait and learn patience than in a baseball stadium? Those endless baseball games are patience boot camp. Patience is power! This message from Vin Scully about our current war on COVID-19 tells it all. Vin missed the 1918 influenza season (he was born in 1927 — give him a break), but he called Dodgers games for 67 years. No stranger to disaster, Vin survived the Great Depression, World War II, AND the Dodgers move from Brooklyn to Los Angeles. By one account he’s no saint, but nothing beats calm and steady patience right now. CQC is betting this codger does not “sneak out” with his trash but takes it to the curb with authority. After checking the wind direction, of course. And, since there is no baseball today, you might consider an “opening” alternative: classic theater live-streamed every Thursday from England, starting on opening day.
Any idea how long COVID-19 germs live in the refrigerator? I’m wondering about cleaning refrigerator-bound grocery items when they’re delivered. What about the microwave?
As of April 14, 2020

Let’s focus today on a place where there is little air and no sunshine: your refrigerator. Biology labs have refrigerators and freezers. Why? Not just to store lunch. Biologists keep both lunch and biological specimens fresh for experiments by stowing them in the old icebox. But in your refrigerator, biological specimens don’t stay fresh for experiments. You have wilted lettuce, moldy bread, spoiled milk, shriveled blueberries, and jars of expired condiments with rusty lids. The nonbiological specimens like coffee, popcorn, beer, champagne, and Diet Coke never seem to expire. Is that because they lack biology? Or you consume them more quickly? Not totally clear.
Face it. If you leave food in the fridge for a month or more, you’re asking for trouble. So it sounds like SARS-CoV-2 wouldn’t last long either, right? Even refrigerators can’t protect biology from the passage of time forever. For that you need freezers. And if you want to go all in — preserved forever or until the electricity fails — you have to follow the famous deceased baseball slugger Ted Williams to Alcor Cryonics of Scottsdale, Arizona.
Now that CQC has established the cooling intensity options, let’s examine your ordinary overcrowded refrigerator. Can viruses live longer in a refrigerator than in Central Park? Careful with that question — we established that viruses are not really alive. They are just little instructions, coded into a tiny biochemical thread. That thread can only make more copies if it finds a human. Imagine the virus is like a shopping list sitting on your kitchen table. It is inert. It can’t shop. It needs you to pick it up, take it to the grocery store, and generate groceries. Until then, it will just sit there, gathering dust.
So CQC, are you saying that the virus is like the shopping list — it can sit there forever and still be used? Not quite. Imagine a shopping list written with ink that fades. Once the ink is totally faded, no more instructions, no more groceries.
Okay, a virus is a biochemical that breaks down over time. But what about in the refrigerator? Is CQC implying that the virus can live (err, stay legit) longer in the fridge?
The world’s scientific literature is ready with the answer in a paper titled: “Stability of Bovine Coronavirus on Lettuce Surfaces Under Household Refrigeration Conditions.” It all sounds good except for one thing, what’s a bovine?
That’s a cow. And in this study, “. . . bovine coronavirus, diluted in growth media or in bovine fecal suspensions to simulate fecal contamination, was used to spike romaine lettuce.”
Say what? They spiked the lettuce with cow poop. Then they watched, with powerful microscopes:
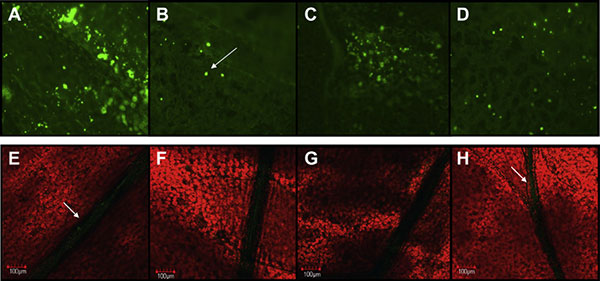
Image courtesy of Elsevier Ltd./National Center for Biotechnology Information.
The red stuff is the lettuce and the green stuff is the virus — Confusing!
Read the paper for the details. The bottom line is that cow poop on romaine lettuce is bad news, especially if it is contaminated with coronavirus and especially if it is refrigerated, where it may remain legit for up to 30 days! Refrigeration is good for coronaviruses — at least the cow kind that causes the common cold.
So, what’s a person to do with lettuce from the grocery store? To answer, extrapolate. If SARS-CoV-2 doesn’t come from cows, how would it get on your lettuce? That would require a human with COVID-19 sneezing on it. That’s not the cow poop scenario though. We have to assume that SARS-CoV-2 acts like common coronavirus on lettuce even though the spike was from a human rather than a cow. (Touchdown!) One option is to leave your lettuce sitting out for a day or two before you refrigerate it. Another is to wash the lettuce well as soon as you take it out of the bag. Then wash your hands. Don’t touch your face ever! Will washing remove every viral particle? No. But it will reduce your risk. And who wants cow poop on their lettuce?!
Science can only take you so far. For truly practical advice on kitchen hot spots, cold spots, microwave spots, and germ spots, check out this parenting advice.
Enough. We need distraction. Something uplifting. It’s time to introduce the new...
Corner Feature: Life Goes On!
In this feature, CQC highlights human resilience (science occasionally included). Wedding plans busted? Turn lemons into lemonade — like this couple who relocated their wedding vows to a classy medical historic setting, the Ether Dome of Massachusetts General Hospital. For playwrights, tragedies end in death, but comedies end with weddings.

Jen Andonian, project manager for the Massachusetts General Hospital Center for Disaster Medicine, and Matt Shearer, senior analyst at the Johns Hopkins Center for Health Security and Research Associate at the Johns Hopkins Bloomberg School of Public Health, get married at the MGH Ether Dome in Boston on March 27, 2020. Photo by Suzanne Kreiter/The Boston Globe via Getty Images.
We can never know whether each day might be our last. Every day is a good day to tell COVID-19 that you will not let it spoil your happy moments. Like this couple, who elbow-bumped their way to happiness. Think about something you have always wanted to do and make it happen, today, wherever you may be!
I’m wondering if we have any sense of what drugs, if any, seem to be helpful for treating patients so far. I get the sense that we don’t know what works, and I’m wondering why that might be. Didn’t we have a chance to collect a lot of information, given almost half a million worldwide confirmed cases?
As of April 9, 2020
You are understandably focused on drugs, specifically antivirals — antibiotics don’t work against viruses. Americans believe in medicine for every ailment. A century ago, Sir William Osler observed that the desire to take medicine distinguished humans from all other animals. We have had this drug obsession for a long time. We embarrass our dogs.
All the information from the overseas cases? Let’s go overseas! As England entered World War II in 1940, Winston Churchill gave his famous “We Shall Fight on the Beaches” speech. To be sure, he was not talking about spring break in Florida. But the speech contained these famous words: “You ask, what is our policy? I will say: It is to wage war, by sea, land, and air.” If Churchill were alive today and leading the U.S. against the invisible enemy, SARS-CoV-2, he might have ditched the sea and the land and focused exclusively on the air. Open air, to be precise.
Before antivirals, and before electron microscopes offered the power to see viruses, public health officials understood that open air could reduce transmission of infectious diseases. In 1918, at the height of the influenza epidemic, Boston public health officials evacuated influenza-infected sailors from ships anchored in Boston Harbor to outdoor tents.

Emergency hospital at Brookline, Massachusetts to care for influenza cases. Courtesy: National Archives
Tuberculosis was also trouble then. TB is more contagious than SARS-CoV-2. TB’s reproductive number (R0) is a 10! On average, one person with TB will infect 10 others. Take that, SARS-CoV-2 with your puny R0 less than three! Also, don’t mess with that field hospital nurse. She looks tough.
Who says history does not repeat itself? On Sunday, the first tent hospitals began to rise in northern Central Park near 5th Avenue and Mount Sinai Hospital. Or perhaps those were aliens from Area 51 in Nevada. They finally traveled to New York City, using this moment as cover to build their planned summer colony.

A view of a temporary hospital being built by the Samaritan's Purse at Central Park, East Meadow NYC on March 30, 2020. (Photo by John Nacion/NurPhoto via Getty Images)
You think that CQC is pulling your leg with talk about aliens and the healing properties of fresh air. But there is a long and storied history of ventilation as therapy. Florence Nightingale’s 1859 book Notes on Hospitals featured an innovation: open wards with large windows to let in light and air. For a long, long scientific review of the topic, CQC commends you to this publication. Indeed, what was true 100 years ago is still true today. Kirkland, Washington, near Seattle, had very few infections among first responders. Why? Their first responders didn’t charge into nursing homes. Instead, they waited outside while the elderly patients were brought to them. Once outside, the infection risk was much reduced. Aerosol droplets disperse quickly in the wind. Seattle has started to flatten the curve on COVID-19.
If this weren’t a Seattle story, CQC might also point out the contribution of sunlight to flattening the curve. Sunlight? Yes! Sunlight really is among the best disinfectants when it comes to viruses. Ultraviolet radiation fries viruses. Those decontamination units with the purplish disco mood lighting? UV radiation. Sunlight is powerful. It can also kill dust-dwelling bacteria in your house.
My roommate just got sick. Now what?
As of April 9, 2020
Ugh. The alien invasion finally made it through the front door. Time to panic? No. Time to trigger the CQC action plan:
- Take a deep breath and pause.
- Get the facts, evaluate the situation.
- Make a plan.
- Execute the plan.
- Adjust the plan as needed to respond to new facts.
Scenario planning is a science. Let’s walk through what happens at each of those five steps:
- Om and namaste: oxygen enters your brain. You begin to think clearly!
- Is there an app for this? What does the CDC website say? What is the phone number of my doctor/nurse/clinic? What would CQC do? But, no surprise. If you stay home or work from home with others for weeks or months, eventually somebody will develop cold symptoms, a cough, or fever.
- What’s the plan? The person with symptoms should be isolated from everyone else as much as possible. Keep the windows open for ventilation. The sick person should wear a mask and not share any objects that haven’t been washed with soap and water or wiped down with rubbing alcohol or Lysol wipes. Clothes and linens should be put aside or out in the sun and air if possible.
- Ventilation and sun, wiping and washing, pass food in and out. Wipe the bathroom after every use.
- Stay alert for changes like worsening symptoms or changes to CDC guidance about how to handle sick people.
It sounds tedious. Isn’t it too late anyway? If they have it, surely you have it too. But there are good reasons to isolate sick people. One is that it takes more exposure than you think to transmit a virus. Do not assume you or others are infected already, especially if your roommate has a common cold virus rather than COVID-19. More importantly, even if you catch COVID-19, a smaller dose of virus may produce a milder illness with fewer symptoms and less chance of needing the hospital.
How is that possible? The idea, with some evidence to back it, is that the immune system tends to overreact if it is exposed too quickly to a large number of viral particles. That overreaction can produce a more severe illness. Conversely, being exposed to a smaller number of viral particles over a longer time, your immune system has time to react properly and control the virus. You may still catch COVID-19, but if you do, your symptoms may be fewer, less severe, and less likely to land you in the hospital. And you will develop immunity.
The inability to maintain separation may be one reason health care workers are especially vulnerable to COVID-19 if they don’t have personal protective equipment (PPE). Hospital patients are sick enough that they may shed large numbers of virus particles. Without adequate protective gear health care workers in close contact with infected patients for hours on end may get large doses of virus. Their immune systems may be overwhelmed by that exposure. And that may lead to more severe illness.
The science is still developing on this, but for more, see this excellent essay.
While we wait for scientists to figure out vaccines, antivirals, and other modern miracles, and our government figures out how to get PPE to vital health care workers, this is a good time to rediscover tried and true methods that our grandmother’s grandmother used to get the country back on its feet.
Until then, NYC has Central Park. That beautiful garden has always been mobilized in times of crisis. For example, in 1918, New Yorkers formed “wool brigades,” spinning and knitting the wool needed by soldiers at the front. You can always count on New Yorkers to rally in a crisis. And they like to rally together, in the open air of city parks. And they always do it in style, even if they don’t get the physical distancing quite right!

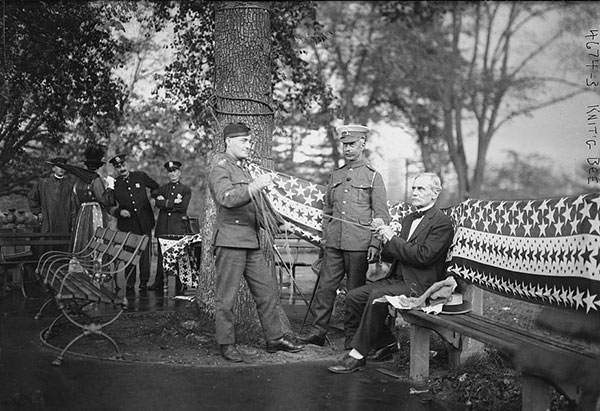
Knitters at the Central Park knitting bee, 1918. Courtesy: National Archives; Attendees of the Central Park knitting bee, including British soldiers and a Civil War veteran, 1918. Courtesy: Library of Congress
Why does the disease seem to be affecting different demographics in different countries? Italy has high fatality rates and Germany has low ones. What do you make of the CDC data reporting that in the U.S. there more severe cases in adults under 50 than were seen in China?
As of April 7, 2020.
The comparative data we have are all over the map — literally. Case counts, hospitalizations, deaths. Every metric shows wild and weird variation between countries. We also see weirdness within the U.S. between states, but that is not so unusual. Studies from different places reveal different patterns of disease by age and even by different blood types. What explains all these differences?
CQC pointed out recently that this coronavirus doesn’t mutate very much. If the virus is the same everywhere, it can’t be blamed for the differences. Who gets sick and how sick they get must be because of something else. Many factors might cause differences. It could be about people: genetics, vaping habits, screen time, twitter habits, cyberbullying, or their preference for paper vs. plastic at the grocery store. It could be their insurance coverage, copayments, or deductibles, or those doctor visits they were skipping. Or, as the virus is slamming New York City, maybe it’s about social determinants. Like how your nearest subway station may be the best predictor of your health outcomes. Or if you are into climate change, maybe this is payback for degrading the environment. We used to do a lot of that before the BIG SHUTDOWN — you know, back when we had actual carbon footprints.
If we compare the U.S. to South Korea, the difference is very stark. They won several Oscars for Parasite AND vanquished COVID-19. We are wondering if we can keep the future body count to less than seven figures.

Okay, okay. CQC can see you are motivated to use science — the method of generating hypotheses, testing them, and falsifying them (aka “shooting them down”) — as a bazooka in your quest for the truth. Karl Popper and CQC are with you. Science rocks!
So, you may be surprised that the experts’ answer is: “It may just be bad luck.” Eureka! That explains everything! Didn’t your mother say once that bad luck comes to everyone who doesn’t listen to her advice? Or was that your dad talking? Childhood was so long ago.
There are different kinds of bad luck. There is the bad luck in that we are fighting an invisible enemy. We should all be wearing x-ray microscope vision goggles. Next, nobody thought to collect the data researchers could use. Data are the lifeblood of science. Without those long overdue test kits, the lifeblood is nowhere to be found. Without lifeblood, those great ideas from research teams just aren’t happening.
Okay. No lifeblood. But there must be data somewhere. This is the digital age and data is the new oil! Americans may not know how to plan, but we sure know how to panic. And when it’s time to panic, we throw everything we have at a problem (including our smartphones, which happen to be within easy reach on the couch). If we don’t spend taxpayer money or have to get off the couch, maybe our smartphones will support the science. Smartphones collect data about our every move.
We also have tech billionaires. Maybe they could finance some really weird pet projects. Like the comprehensive study of the entire global pandemic based on testing everyone who lives in San Miguel County in Colorado. How does the virus affect the 8,000 rich Airbnb owners and ski bums hanging in Telluride? You’ll be dying to know!
The billionaire idea needs work. Still, the smartphone surveillance thing sounds cool and futuristic. But what about George Orwell’s 1984? If the smartphone surveillance is too obvious, wouldn’t people rise up like in Hong Kong last year or like Neo in the Matrix movies. One little red pill and people are wide awake, protesting, shooting stuff, burning stuff, and . . . kissing?

But give credit where credit is due. Those smart phones enabled the New York Times to track the virus from a Wuhan seafood market, to a train station, to gate 74 at Wuhan airport, to gate A20 at JFK, to a taxi to Times Square, to a hotel, dinner, and a performance of Cats (which turned out to be showing in Providence, Rhode Island). Then on to spring break in Fort Lauderdale, but only after a brief side trip to Mardi Gras in New Orleans. Very cool visuals. All those dots marching like ants. The smartphone surveillance system has other neat applications. Have you seen the leaderboard on social distancing practices? States receive scores based on how smartphones are sloshing around within their borders. And you thought March Madness was cancelled this year!
Those variations in COVID-19 you see out there? Nothing really. Bad luck and early days with not enough data. A pandemic is like horse racing; you can’t tell which horse is in the lead when they first come out of the gate.
Is there any evidence that once you recover from coronavirus you are immune and can’t become infected again? Would a reinfection be less contagious and severe because the body has already created antibodies against the virus? Because viruses can mutate and there is no vaccine yet, I’ve been wondering if immunity (herd or individual) would even matter with coronavirus?
As of April 2, 2020.
SARS-CoV-2 is a bummer in so many ways. Try to say SARS-CoV-2 really fast five times. It is a tongue twister, assuming you pronounced it once. And SARS-CoV-2 is also a bummer for pangolins.

Pangolins are a misunderstood and aggrieved lot. You thought they were dragons, but experts tell CQC they are anteaters. Apparently they are trafficked by criminals and unfairly smuggled into China. Now, they have been unfairly smuggled into the narrative of our global COVID-19 pandemic. Along with bats, pangolins were indicted as a transmission vector for SARS-CoV-2. (Turns out typing SARS-CoV-2 is a finger twister, too.) People are accusing pangolins of being viral jumper cables. It is true that these adorable little dragons (err, anteaters) carry viruses like coronaviruses, but scientists who know pangolins know they would never hurt a human being. Also — public service announcement — if your car battery dies while you are in isolation, pangolins are not actually very good jumper cables, either.
SARS-CoV-2 has its own special taste-and-lung-destroying powers. But it shares a lot of features with other viruses like Agent Smith.

Humans and other vertebrates have been dealing with Agent Smith for millions of years. In humans, nearly all viruses generate an immune response. Our immune systems know a thing or two about surveillance and destruction. One of the cleverest viruses was HIV, the virus that causes AIDS. HIV had a special key that switched off T helper cells. Those T helper cells are sort of like the doorbell video camera that guards the front door to your house. Once T helper cells are knocked out, the rest of the immune system stays on coffee break. It’s as if the 911 operator and the police never got the call from your doorbell. They don’t even know your house is being robbed. HIV is very talented.
But SARS-CoV-2 is not so talented. For more on this, see the New York Times expert roundup. Like other coronaviruses, SARS-CoV-2 generates an immune response in most humans. Sometimes too much of an immune response, resulting in severe illness. But for most people, in the days you start to recover, the virus is already crippled and no longer infectious. You have immunity. And even if that immunity fades after a year or two, you are extremely unlikely to get reinfected right away.
The best news of the week was about the mutation (not to be confused with the arm wrestler The Mutant). When it comes to mutation, SARS-CoV-2 is kind of a dud. Scientists have studied the countless generations of SARS-CoV-2 ancestry seeking long-lost celebrity connections somewhere in the past three months. They report that the virus is pretty much the same worldwide even after traveling through half a million humans. In contrast, influenza virus mutates a lot. Flu needs a new vaccine every year because of those mutation powers. If SARS-CoV-2 doesn’t mutate, COVID-19 prevention might be as simple as one vaccine and done for life! Like an overhyped March Madness team, one and done! That’s good news for all of us. Except maybe for the vaccine manufacturer whose potential future global sales just tanked. But don’t worry, with an outrageous launch price, rebates, and pharmacy benefit manager shenanigans, the vaccine maker will be okay.
By now, you may have “herd” about “herd immunity.” But what is that really? How much herding is good? How much is too much? Aren’t herding and social distancing in conflict?
As of March 31, 2020.
Herds are great. We don’t appreciate how much we draw strength and protection from our herds. Herds are comforting. We gravitate toward herds and mostly follow wherever they go.
Here are some awesome things — and some less awesome things — about herds:
- You can get through most of life without too much thought or worry if you follow the herd. Herds can tell us what to wear, what to eat, what shows to watch, which of our social media posts are worthy, and where to spend our vacations. You can even go against the herd and the herd will let you know you did it. Admittedly the herd thing can go south, like when someone calls “fire” in a crowded theater. Stampedes are a bad feature of herds.
- Herds have invisible superpowers that lift other responsibilities from our shoulders. Herd immunity is one example. Herd immunity can make even crappy vaccines seem more effective.
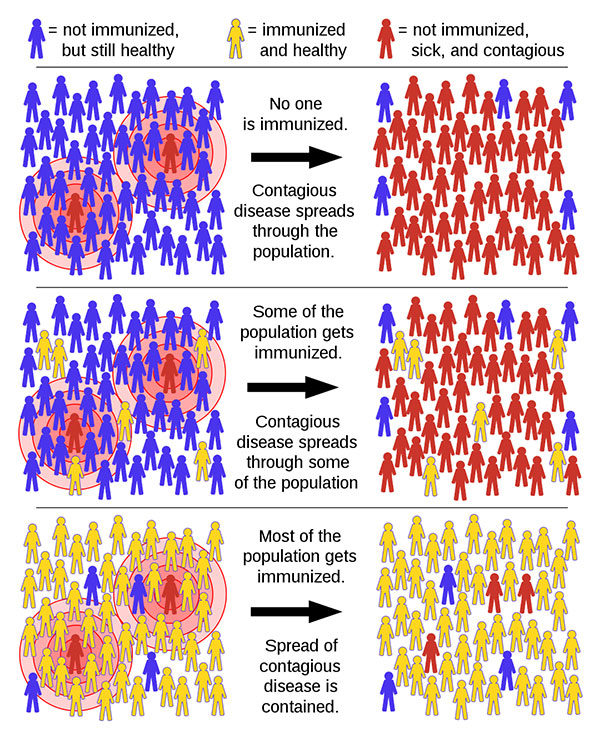
Herd immunity was first described in 1923, but it has probably been around since the beginning of life. Before vaccines and antibiotics were invented, herd immunity was our only defense against infectious diseases.
But how does this work? Imagine you are a virus attacking a new population. You win by replicating and infecting as many people as you can. You lose when you can’t replicate any more. Being contagious helps a lot, but that’s not all it takes to win. You can’t make your humans too sick. If too many people get sick too quickly, you lose quickly. You need the humans to do your replication thing and infect more humans. But the humans have strategies too: one is individual immunity. Humans become immune when they recover. Next time you try to infect them, you hit a wall. The other human strategy is herd immunity. As increasing numbers of humans become immune, you have trouble finding nonimmune humans. The herd strikes back! Best of all, once most of the herd is immune, it's game over for you, virus.
We don’t know the exact number, but once 60 percent of the herd becomes immune, the virus can’t spread easily anymore. Think about this: what if all the healthy young people in the herd (roughly 60% of the population) could get the infection and get immunity before the older and chronically ill people were exposed? In theory, our hospitals and health care workers would be back to normal. However, we have also seen that younger people can contract the virus — and sometimes die.
This is a paradox. We would like to build herd immunity quickly, but the only safe path is to protect the vulnerable while we build it. Social distancing protects us from the virus, but it slows development of herd immunity because fewer people are getting infected. So as of now, we are unable to use our herd superpower. But at this point, it is way more important to protect the vulnerable and our health care workers. The herd superpower won’t go away. It will be there for us later in the pandemic.
A photographer at an event we attended two weeks ago was confirmed by testing to have COVID-19. Should we take extra precautions?
As of March 31, 2020.

Everyone will face this situation eventually. Someone tested positive and we were in the same room at the same time. As scary as it sounds, you only need to worry if you had close contact. Fine, but how close is close? And for how long?
The formal definition of close contact is “within 6 feet of the confirmed case for more than 15 minutes.” Unless you are a supermodel who specializes in close-ups, you probably won’t be that close to any photographer during your lifetime. If you were in the room but didn’t have close contact, you do not need to take extra precautions.
But what if the photographer sat next to you during dinner? In that situation, the usual precautions apply: self-isolate and monitor your symptoms and temperature. If you start to cough, have a fever, or feel malaise, you could call your doctor or nurse.
How long can the virus live on surfaces? Or more precisely, since March Madness was cancelled, if I make a shot with my basketball and it swishes, could it get coronavirus on it from someone else's basketball that also swished in before?
As of March 26, 2020.
CQC is at the white board, mapping this complex technical challenge. First, you seem to be skilled if you are not hitting the rim or throwing air balls. If you are an NBA player or your pick-up game involves NBA players, you can easily calculate your risk. Despite a shortage of tests, all NBA players have been tested. If their tests are negative, your net is safe. But if your game does not involve NBA players with negative test results? Call a timeout. What part of basketball does not involve close contact? All team sports have been banned. Even boxing. Especially boxing. Game over!
You say you are shooting alone. Ahh, the basketball version of Bowling Alone. That book documented a decline since the 1950’s in social capital. Americans don’t gather together like they used to. How ironic that Americans have been preparing for this moment since the 1950s. But no one is an island. Who was on the court before you? Is the virus that causes COVID-19 hanging from the net for dear life while you dribble and set for your shot?
Experts debate whether viruses should be classified as living things or just toxic chemicals. While experts debate whether viruses are alive, let’s go to the journals. A recent study says that for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the virus that causes the COVID-19 disease can “live” for up to three days on plastic and steel, but only for a matter of hours on cardboard and copper. Although the virus that causes COVID-19 can be detected on surfaces for that long, all coronaviruses are very fragile when stored outside the refrigerator in the open air. A study of another coronavirus, influenza, showed that virus on plastic or steel lost its punch after eight hours. On tissues, cloth, and cardboard, it may be infectious for less than 30 minutes. COVID-19 is not the flu. It is more dangerous if you catch it. But catching coronaviruses from surfaces is much more difficult than you might imagine.
On to basketballs and nets. Most basketballs are made of rubber — a plastic. Nets are still nylon. Nylon is a plastic. And if you hit the rim (you never do, right?), that’s made of steel or plastic. If someone’s ball drops the COVID-19 virus on the rim or net, that three-pointer at the buzzer could be a game-changer in more ways than one. CQC would opt for a one-day timeout between shooters on the court, especially in March when the virus may persist more easily because of cold weather.
By the way, this handy evidence applies to a lot of situations. Pumping gas? Wipe that nozzle between users. Groceries? Wipe down the plastic covered ones before you bring them into your house. Rims and nets? Wipe those only if you are slam-dunking like LeBron!

Once a person has a positive COVID-19 test, how long are they a risk to infect others?
As of March 26, 2020.
It appears that people who are infected may be most contagious just before symptoms. They may be contagious even if they never had symptoms. A smattering of small case studies suggest that that people with confirmed COVID-19 are unlikely to transmit the virus 10 days after their first symptoms. Whatever virus they shed after their symptoms go away may be crippled by their immune systems. Crippled virus may not infect others. But what if they have no symptoms? The evidence is thin so we have to wait for better data.
Here is one way data can make a difference: South Korea has done more testing of its population than any other country. Findings were surprising. About half of all cases (people with positive test results) were among people under 50 years of age. Most of these younger people had mild symptoms or never had symptoms at all. Note the contrast with Italy, which found more cases among older people. What gives? The Italian picture is what you see when you only test sick people.
Evidence is accumulating that we need to go full South Korea as soon as possible. If the US ends up with the South Korea trend, closing universities and having working-age adults work from home will have been a brilliant first step. The South Korea experience also implies that in our daily lives we must act as if anyone we come into contact with may be shedding COVID-19 virus. But no need to panic. Just keep washing hands, not touching your face, and staying six feet away from people. Not just from sick people, but from everyone. That is the true mantra of physical distancing (what some call social distancing).