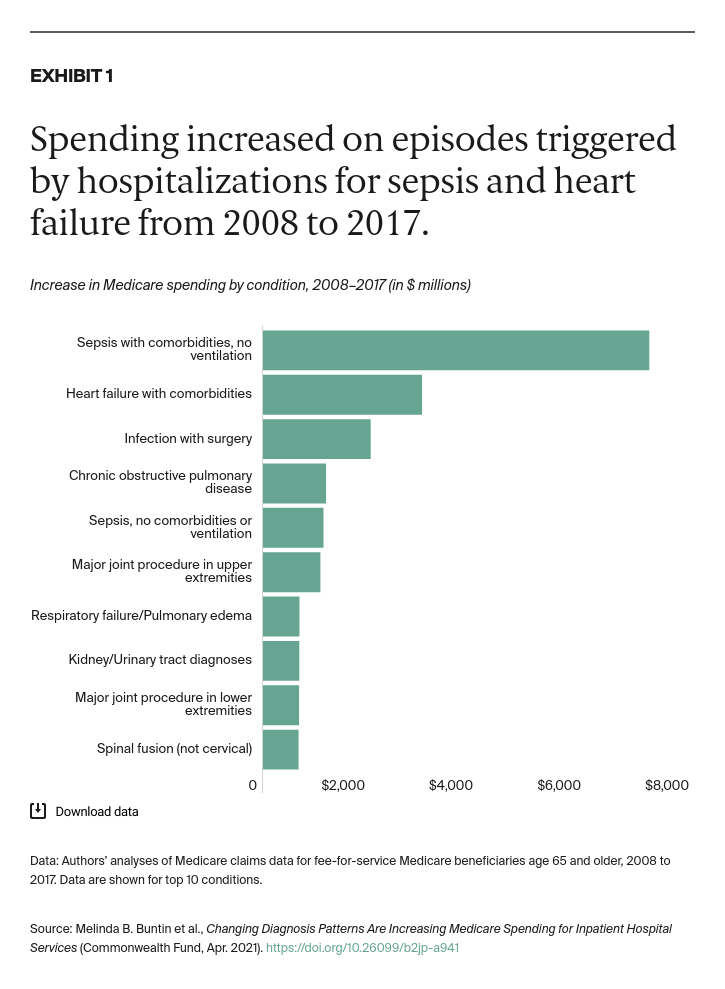
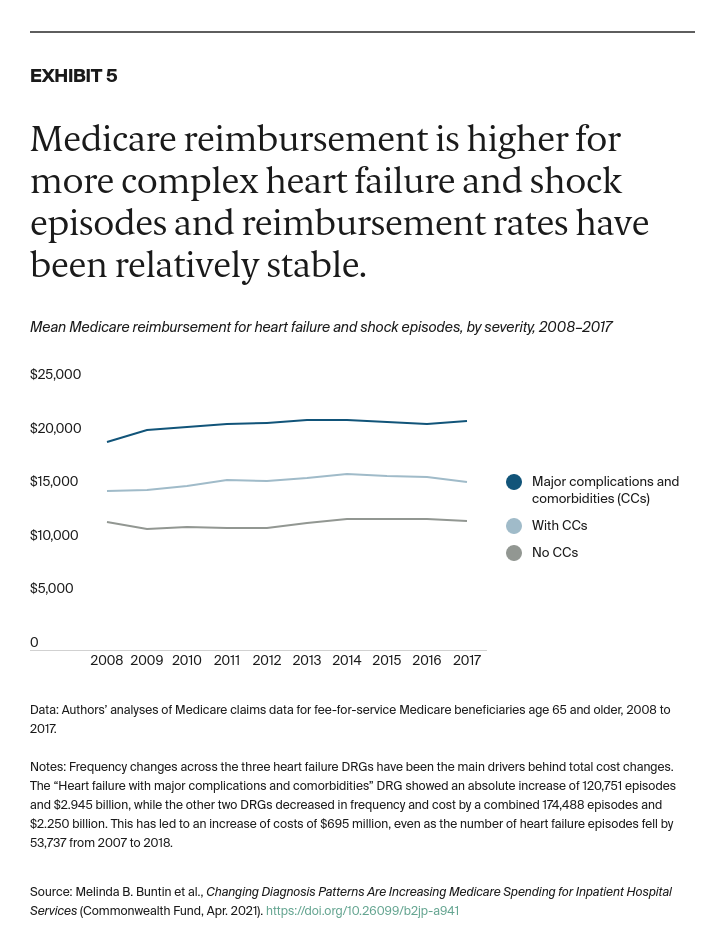
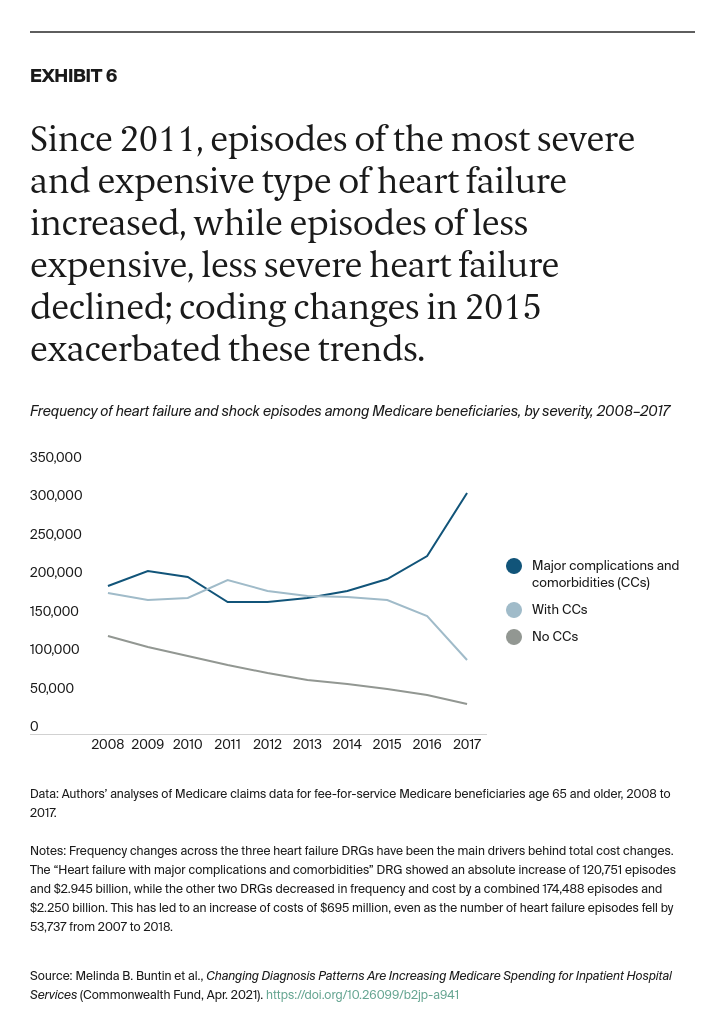
Changes in diagnosis patterns are leading to an increase in Medicare spending for inpatient care. As the charts that follow illustrate, in examining some of the most frequent and fastest-growing episodes, we find high episode growth rates for DRGs (diagnosis-related groups) with higher reimbursement. This implies that overall Medicare spending increases are being driven more by rising volumes of these highly reimbursed services rather than by growth in payments per se. Incentives related to Medicare reimbursement may therefore be spurring changes in medical coding.
Key Findings
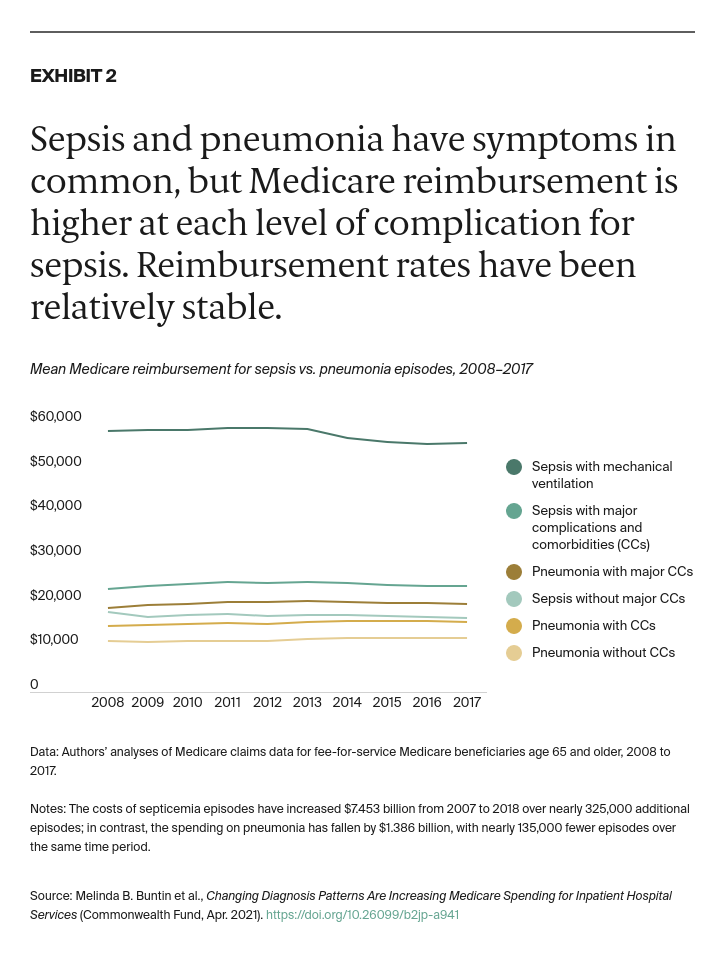
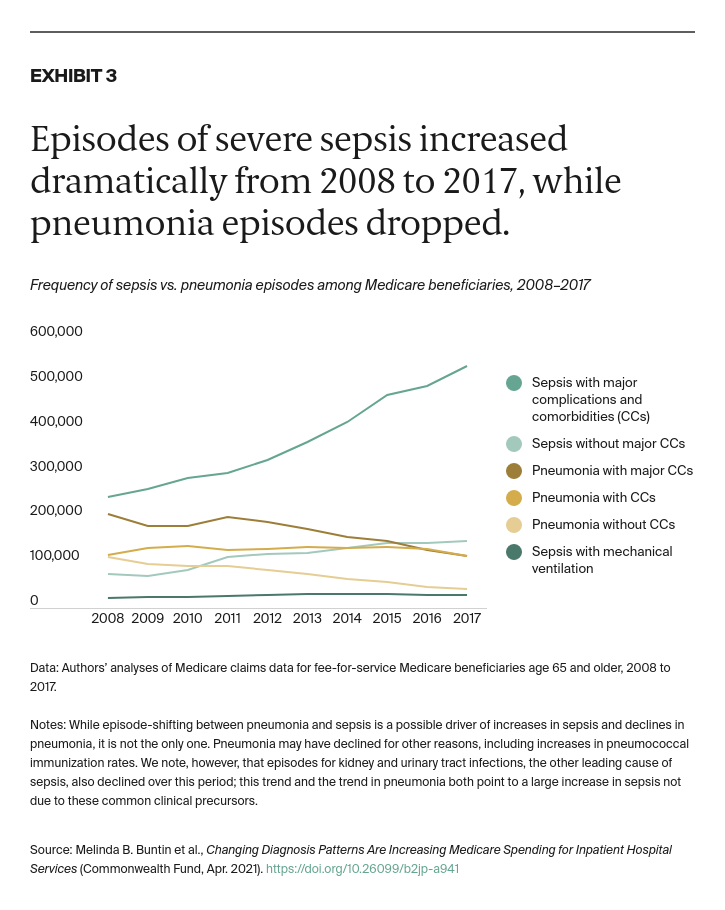
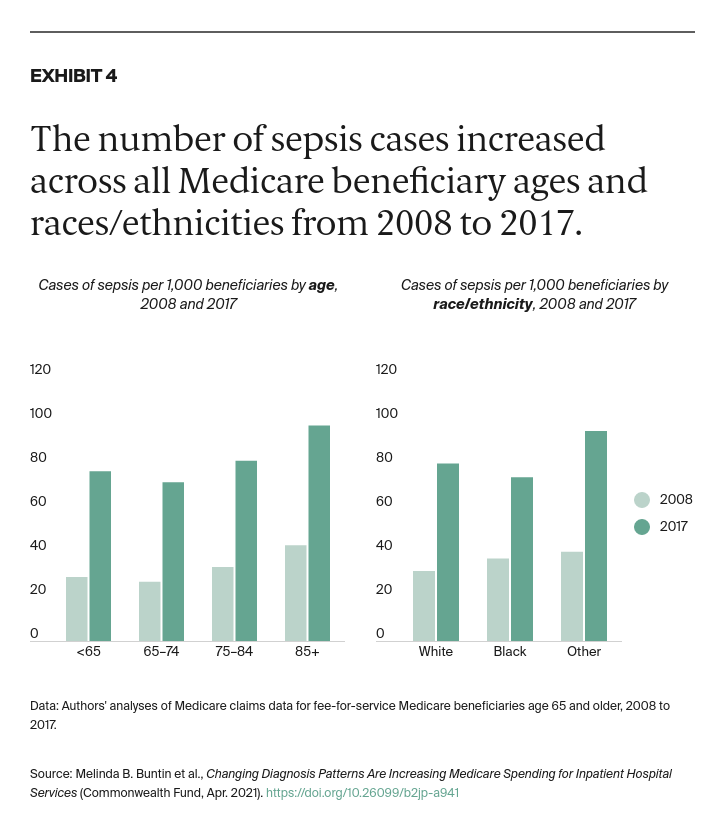
- The frequency of sepsis and severe heart failure has increased, while coding for pneumonia and less severe heart failure has declined.
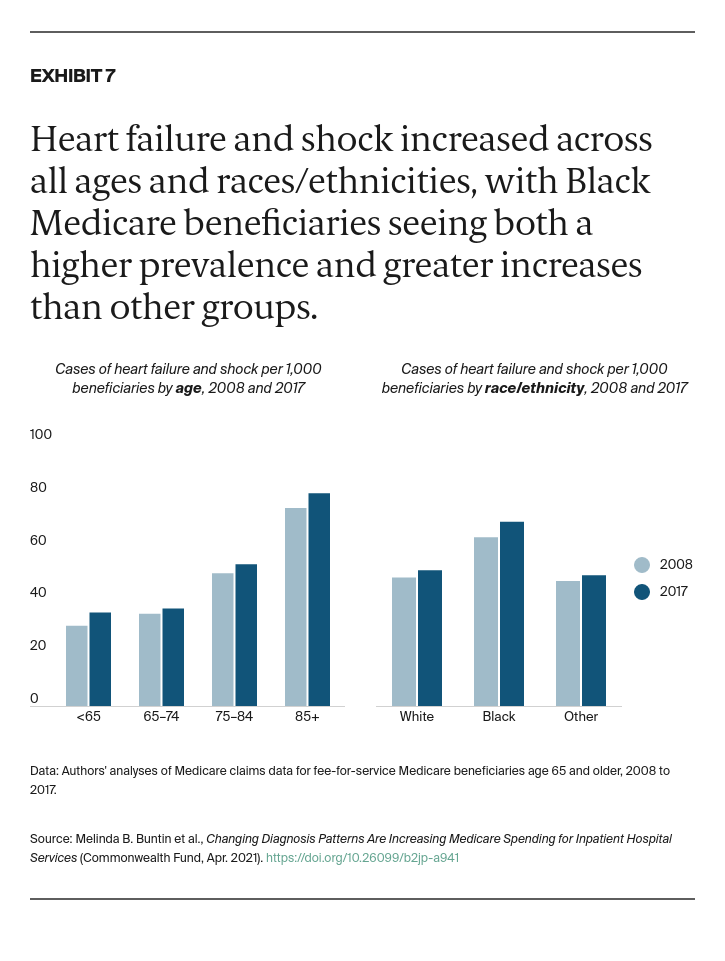
- These shifts in diagnoses are not the result of demographic changes.
- The increase in the frequency of episodes is higher for those with higher reimbursement, suggesting that payment incentives and coding may be contributing to spending increases.