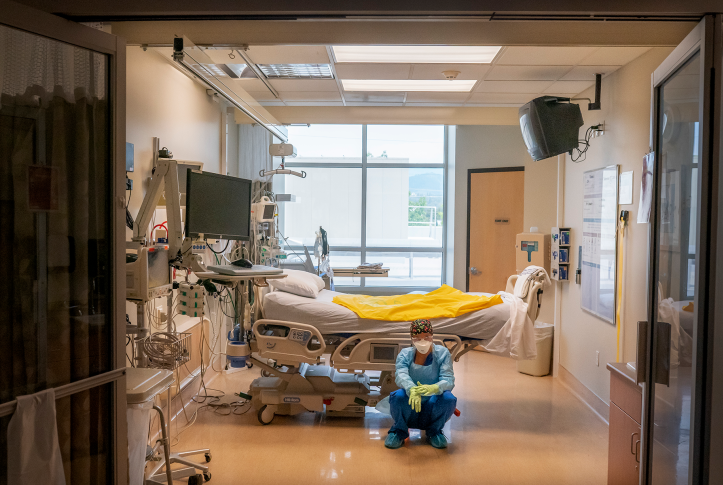
As the COVID-19 pandemic wore on, multiple surveys and news reports described rising levels of burnout and fatigue among clinicians on the front lines. Among the many nurses and physicians reporting they were stressed out and overwhelmed, some said they were ready to leave their jobs. While it’s unclear how many clinicians have quit practicing, workforce shortages continue in some regions.
Burnout can be defined as having too much work and not enough time or resources to do it. In the context of health care, researchers often ascribe it to factors such as increased patient acuity, heavier caseloads, and having insufficient time with patients. The burdens of documentation and performance reporting and barriers like prior authorizations — what are sometimes referred to as administrative harms — can also leave clinicians feeling exhausted and unwilling to continue.
But, increasingly, clinicians are rejecting the term “burnout.” They say they’re not overworked or frustrated, but are instead demoralized by a health care system that puts profits ahead of patients. Nearly every day since Wendy Dean, M.D., and Simon Talbot, M.D., published an op-ed describing physicians’ distress as a form of “moral injury” in Stat, in 2018, they’ve heard from physicians who’ve faced systemic problems that keep them from helping patients. One, an emergency department (ED) physician, had for years warned hospital administrators about the dangers of understaffing. Eventually, a patient died in the ED while he was covering an emergency in an inpatient ward.
Eric Reinhart, M.D., who published “Doctors Aren’t Burned Out From Overwork. We’re Demoralized by Our Health System” in the New York Times, in February, says some clinicians have begun to question the role they play in a health care system that accepts inequitable access to care and fails to address the root causes of disease. “Many physicians are now finding it difficult to quash the suspicion that our institutions, and much of our work inside them, primarily serve a moneymaking machine,” he writes. Discontent is now bubbling up among health care providers in ways not seen since the spread of managed care — including efforts to unionize by physicians and medical trainees.
In this issue of Transforming Care, we explore the manifold causes of burnout and moral injury among clinicians and identify ways in which health care leaders have begun to respond. “Burnout, demoralization, and administrative harm are much more than hot topics of the day,” says Joseph Betancourt, M.D., the Commonwealth Fund’s president and a practicing physician. “They are a clear and present danger to the future of health care, and we ignore them at our own peril.”