What does it mean for a health system to achieve carbon neutrality?
Among the various GHGs that play a role in climate change, carbon dioxide plays the biggest, and the amount of carbon emissions are expected to only increase in the near future. Focusing on them is therefore a natural starting point.
While it’s impossible for a health system to generate zero carbon emissions, health systems could seek to achieve carbon neutrality. They can start by reducing carbon emissions as much as possible, by, for example, using renewable energy, greener models of care delivery, and low- and zero-emission transportation.
Why is it important that U.S. health care reduce its carbon footprint?
In a nutshell, it’s important because:
- Climate change causes numerous negative health impacts. Over the long term, everyone’s health will benefit from efforts to lower carbon emissions.
- The negative health effects of climate change and climate-induced crises disproportionately impact groups that are already at risk, including people of color, people with low income, people with preexisting health conditions, older adults, and children.
- Climate change disrupts the health system’s ability to deliver safe, effective care.
- Caring for the victims of climate change and repairing health facilities following climate events are expensive, and health systems bear much of these costs.
Where are we now, and what do we need to do?
A necessary first step is increasing awareness of the health system’s impact on climate change. At the federal level, the newly established Office of Climate Change and Health Equity is charged with protecting Americans’ health in the face of climate change. While the office has a lot of potential, it has yet to receive the funding it needs.
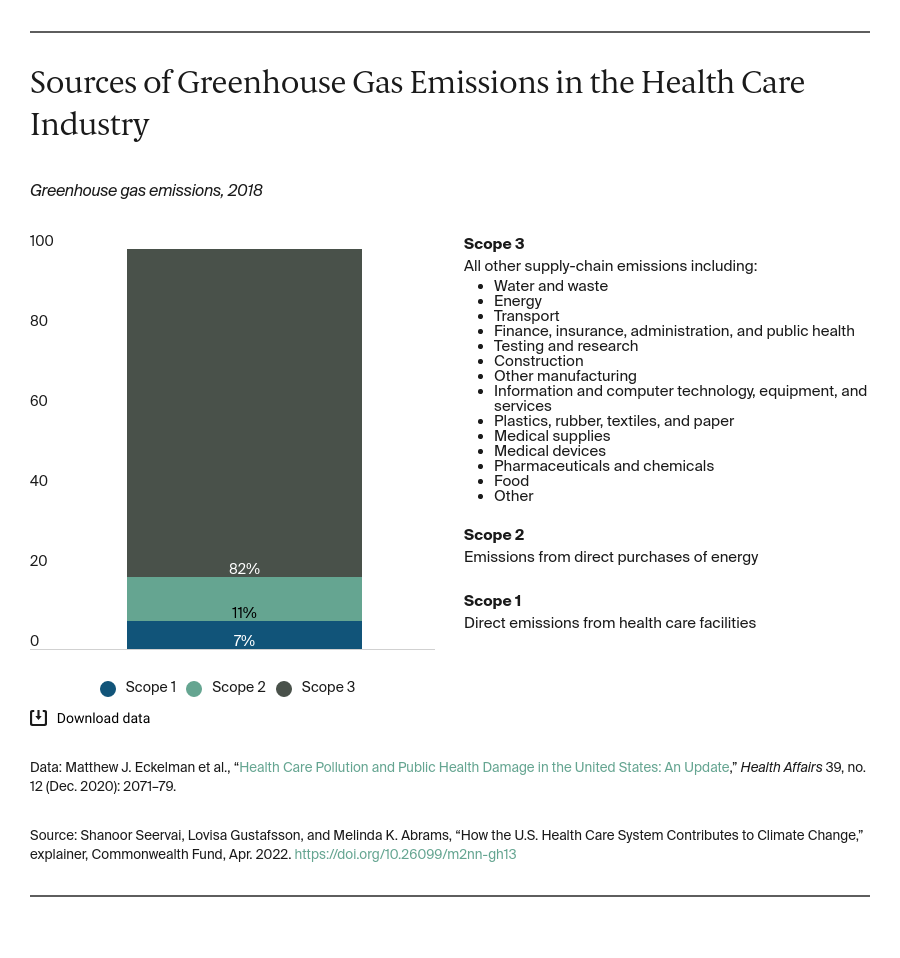
To some extent, health systems must learn to adapt to a changing climate and shore up their resilience. But they also can make an effort to mitigate the levels of GHG emissions they release. A handful of U.S. health systems are making progress, but most others will need to step up and make a stronger commitment. The government could take these further actions:
- Develop standardized metrics of health system performance at the facility, state, and federal levels.
- Enact policies that remove barriers and create incentives for health systems to reduce their GHG emissions.
- Create roadmaps for health systems that show them what to do and how to do it.
Climate change is already devastating the planet. The time to act is now, and health systems must do their part.