Women in the United States have long lagged behind their counterparts in other high-income countries in terms of access to health care and health status. This brief compares U.S. women’s health status, affordability of health plans, and ability to access and utilize care with women in 10 other high-income countries by using international data.
Highlights
- U.S. women report the least positive experiences among the 11 countries studied. They have the greatest burden of chronic illness, highest rates of skipping needed health care because of cost, difficulty affording their health care, and are least satisfied with their care.
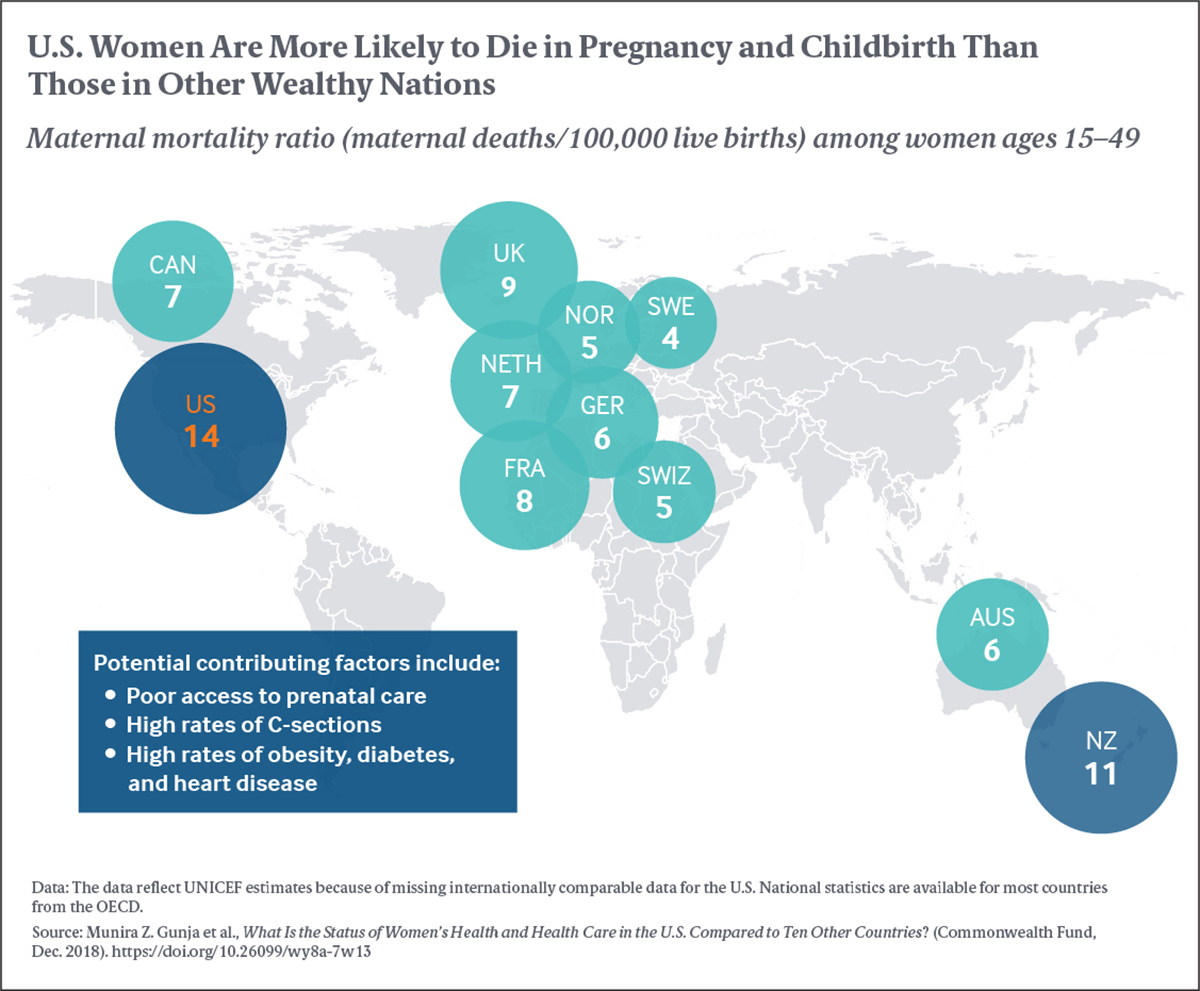
- Women in the U.S. have the highest rate of maternal mortality because of complications from pregnancy or childbirth, as well as among the highest rates of caesarean sections. Women in Sweden and Norway have among the lowest rates of both.
- Women in Sweden and the U.S. report the highest rates of breast cancer screening among countries surveyed; women in Norway, Sweden, Australia, and the U.S. have the lowest rates of breast cancer–related deaths.
- More than one-quarter of women in the U.S. and Switzerland report spending $2,000 or more out of pocket on medical costs for themselves or their family in the past year compared to 5 percent or fewer in most of the other study countries.
- More than one-third of women in the U.S. report skipping needed medical care because of costs, a far higher rate than the other countries included in the study.
- U.S. women are less likely to rate their quality of care as excellent or very good compared to women in all other countries studied.
Background
Compared to women in other high-income countries — like, for instance, Germany or Australia — American women have long struggled to access the health care they need. The United States spends more on health care than other countries do, but Americans report high rates of not seeking care because of costs, as well as high instances of chronic disease. Prior research has found that poor access to primary care in the United States had led to inadequate management and prevention of diagnoses and diseases.
With the Affordable Care Act (ACA) now in place, most women in the U.S. have guaranteed access to health coverage (Appendix 2); more than 7 million working-age women have gained insurance since the implementation of the law. Millions of others who had been insured now receive additional benefits and cost protections through the law’s reforms. But recent changes by the Trump administration and Congress may jeopardize this progress. These changes include repeal of the law’s individual mandate penalty; expansion of plans that do not have to comply with the law’s consumer protections and benefit requirements, including the requirement to provide maternity care; threats to remove guaranteed coverage of preexisting conditions; and proposed changes to Title X funding. In the future, these changes may raise costs and limit access to health insurance and services for people who do not qualify for subsidized care, especially those with health problems. They could reduce the recent gains U.S. women have made and widen differences between women in the U.S. and those in other countries.
Using data from the Commonwealth Fund International Health Policy Survey (2016) and measures from the Organisation for Economic Co-operation and Development (OECD) and the United Nations Children’s Fund (UNICEF), this brief compares U.S. women’s health status, affordability of health plans, and ability to access and utilize care with women in 10 other industrialized countries.
For an overview of each country’s health care system, see Appendix 1, and for further detailed information on each country’s health system, see the Commonwealth Fund International Health Care System Profiles here.
Women in the U.S. reported a higher rate of having multiple chronic diseases compared to women in the 10 other countries, with German women reporting the lowest rates. One of five U.S. women reported having two or more chronic conditions, compared to one of 10 or less in Germany, the Netherlands, and Australia. Chronic diseases include a diagnosis of joint pain or arthritis, asthma or chronic lung disease, diabetes, heart disease, or high blood pressure.
The relationship between emotional distress and health is complex, but some research shows emotional distress can exacerbate physical illness as well as lead to difficulties managing other aspects of life, such as the ability to work. One-quarter or more of women in Australia, Norway, New Zealand, Switzerland, Sweden, Canada, and the U.S. reported having experienced emotional distress — that is, anxiety or sadness that was difficult to cope with alone in the past two years. Only 7 percent of women in Germany reported having emotional distress and only 11 percent of women in France.
Women in the U.S. had the highest rate of maternal mortality because of complications from pregnancy or childbirth; women in Sweden and Norway had among the lowest rates. High rates of caesarean sections, lack of prenatal care, and increased rates of obesity, diabetes, and heart disease may be contributing factors to the high rate in the U.S.
Caesarean sections are generally not recommended for younger mothers with uncomplicated births and are often more costly than vaginal births because of the costs of the operating room and medical personnel, longer recovery, and hospital stays. Australia, Switzerland, and the U.S. have the highest rates, while women in Norway and the Netherlands have the lowest rates — approximately half the rate of the highest-ranking countries. The reasons behind the wide variation observed in caesarean section rates across developed countries warrants further investigation; however, some researchers suggest it is a combination of a country’s specific health system, physician and patient preferences, cultural factors, population characteristics, and payment incentives.
It is recommended that women have screenings for breast and cervical cancers. The U.S. fares well compared to other countries on these indicators. Older women in the U.S. and Sweden are screened for breast cancer more often than women in the other countries analyzed; women in Switzerland are screened at the lowest rate.
Women in the U.S. had among the lowest rates of breast cancer–related deaths, after Norway, Sweden, and Australia. Women in the Netherlands and Germany had the highest rates.
High health care costs create significant financial burdens on U.S. household budgets, even among insured families. Over one-quarter of women in Switzerland and the U.S. reported spending $2,000 or more in out-of-pocket medical costs for themselves or their family in the past year. In comparison, no more than one of 20 women reported such high costs in most other countries included in the study.
U.S. women most often reported problems paying or disputing medical bills or spending time on related paperwork. Nearly half (44%) of women in the U.S. faced such problems compared with only 2 percent in the U.K. U.S. women had the highest rates of having payment denied by their insurers or receiving a smaller insurance payment than they expected, compared to women in other countries (Appendix 4).
Many women in the U.S. skip needed medical care because of costs, likely because of high out-of-pocket costs and the fact that 11 million women still have no insurance coverage. Thirty-eight percent of women in the U.S. reported they went without recommended care, did not see a doctor when sick, or failed to fill prescriptions because of costs in the past year. This is the highest rate among the 11 countries in our analysis (Appendix 5). Before the implementation of the ACA in the U.S., the rate was even higher, 43 percent. In the U.K. and Germany, only 5 percent and 7 percent of women, respectively, reported forgoing care because of cost.
Having a regular doctor or place of care, such as a primary care physician, is important for preventing disease, managing chronic conditions, and coordinating specialist visits. Majorities of women in all 11 countries reported having a regular doctor or place of care. But somewhat fewer women in the U.S. and Switzerland reported having a regular doctor, compared to those in the other nine countries. In contrast, all women in the Netherlands reported having a regular doctor or place of care.
More than one of three women in Canada, the U.S., and Sweden reported emergency department (ED) visits in the past two years; rates were lower in other countries. Women in Germany had the lowest rate of ED visits.
Women in the U.S., Switzerland, and the Netherlands had quicker access to specialist care. Among women who needed to see a specialist in the past two years, only a quarter of women in these countries had to wait more than four weeks for an appointment, compared to the majority of women in Canada and Norway.
U.S. women were the least likely to rate their quality of care as excellent or very good compared to women in all other countries studied. More than 60 percent of women in the U.K. and Switzerland rated the quality of their health care as high, compared with one-quarter in the U.S. Further analyses showed that women with multiple chronic conditions or emotional distress, and those who faced high out-of-pocket costs, medical bill or cost-related access problems, long specialty wait times, or had emergency department visits were significantly less likely to rate their quality of care as good (data not shown).
Conclusions and Policy Implications
Women in the United States continue to be disadvantaged by their relatively poorer health status and higher costs of care, while benefiting from higher rates of preventive screenings and quicker access to specialty care. While this study did not investigate the reasons behind these findings, they might be viewed in the context of lower rates of health insurance coverage in the U.S., as well as differences in health care delivery systems and the level of social protection across countries.
Consistent with other research, we find that U.S. women have the highest rate of maternal mortality among high-income countries. What’s more, this rate has been steadily rising in the past decades. Considerable racial, rural-urban, and other socioeconomic disparities also persist. U.S. maternal mortality is three times higher among African American mothers — with rates similar to those found in developing countries — compared to white mothers.
It is notable that U.S. women face fewer barriers to accessing specialist care relative to women in most of the 10 other countries analyzed. The U.S. also outperforms most countries in terms of breast cancer screenings. This, coupled with relatively low rate of breast cancer deaths, may be associated with the high quality of cancer care delivered in the U.S., including extensive screenings, treatments, and technology.
Despite the significant gains the United States has made in health insurance coverage since the implementation of the ACA, the U.S. remains the only country in this study without universal coverage. Uninsured adults most often cite concerns about affordability as the reason they do not shop for coverage. Coverage is out of reach for people with low incomes who live in states that have not expanded Medicaid and those who are undocumented and therefore ineligible for coverage. In addition, many people in the U.S. have insurance plans with high levels of cost-sharing. More than one-third of women in the U.S. continue to skip needed care because of costs. While the rates of going without needed care because of costs and problems paying medical bills have decreased since 2010, they are still the highest among all 11 countries included in the 2016 Commonwealth Fund International Health Policy Survey.
The continued efforts by Congress and the Trump administration to weaken the ACA, rather than improve the quality and affordability of health insurance, may increase the cost of insurance and make it more difficult for some women to afford comprehensive health coverage. These actions include the administration’s support for ending the ACA’s guaranteed issue and preexisting conditions protections, which ensure every individual has access to insurance regardless of their health status, and expanding the availability of plans which are not required to comply with the law’s consumer protections. A recent analysis of 24 short-term insurance policies found that none provided coverage for maternity care.
The administration’s recently proposed changes to the Title X program — including cuts to funding for family planning services, counseling, and routine exams and cancer screenings — will reduce access to health services among low-income women and minorities. The proposed regulations would block federal funding to family planning providers that provide abortion services. Nearly 4,000 health centers across the country receive such Title X funding, and over 4 million women, the vast majority of whom have incomes below 150 percent of the federal poverty level, annually receive services from these centers. Many women also receive routine primary care and behavioral health services at women’s health centers. But states can take steps toward prioritizing women’s health. For example, California successfully reduced the rate of maternal mortality by 55 percent in less than a decade, through the statewide Pregnancy-Associated Mortality Review (CA-PAMR) program that introduced surveillance, public health, and quality improvement initiatives for maternal care.
Given the substantial maternal mortality gap between U.S. women and their counterparts in other countries, policymakers might also look at the organization of health systems of these countries. For example, in many other countries compared in this brief, maternal care is free at the point of delivery, including postpartum care (Appendix 1). Furthermore, most countries deliver maternal care in primary care or community-based settings by nurses or midwives, rather than in specialty or inpatient settings using obstetricians, as is often the case in the U.S. This not only makes care more expensive, but also limits women’s choices around childbirth. Midwives attend only 12 percent of U.S. vaginal births. Other countries also provide greater social protection for women of reproductive age. The U.S. remains the only country in the developed world that does not guarantee paid maternity leave, despite International Labor Organization standards recommending that new mothers should be provided at least two-thirds of previous earnings for a minimum of 14 weeks.
Finally, since research suggests that the differences in health spending between the U.S. and the rest of the world stem largely from higher prices, payment and delivery system reform must be at the top of the nation’s policy agenda. For example, international data show that the average costs of a normal delivery or a caesarean section are about twice as high in the U.S. as in Australia and about 40 percent to 60 percent higher than in Switzerland. Bringing health costs under control will help improve access to health insurance and health care.
How We Conducted This Study
This brief includes data from the 2016 Commonwealth Fund International Health Policy Survey of Adults in 11 Countries, conducted by SSRS and country contractors in Australia, Canada, France, Germany, the Netherlands, New Zealand, Norway, Sweden, Switzerland, the U.K., and the U.S. between March and June 2016. The survey was administered by telephone (mobile and landline) using a common questionnaire that was translated and adjusted for country-specific wording. Response rates ranged from 11 percent in Norway to 47 percent in Switzerland. The analysis weighted final samples to reflect the distribution of the adult population in the country, adjusting for age, sex, region, education, and additional variables consistent with country standards. This brief restricts the analysis to 9,254 women ages 18 to 64. Sample sizes for each country are included in Appendix 3. The U.S. sample includes women who reported being uninsured for some of part of the previous calendar year (12 months; 8.3%).
The Organisation for Economic Co-operation and Development (OECD) is an international organization representing 36 industrialized countries that share a commitment to democracy and a market economy. The OECD produces reports and data on a wide range of economic and social issues, including the OECD Health Data series, an annual release of data on various aspects of health and health care in the member countries. Working with statistical offices in each member country, the OECD produces the most accurate and comprehensive international health care data available on its member nations. Each year, the OECD releases health data on a range of topics, including spending, hospitals, physicians, pharmaceuticals, prevention, mortality, quality, and safety.
Commonwealth Fund staff analyzed data from the Commonwealth Fund International Health Policy Survey of Adults in 11 Countries as well as data extracted from the OECD on August 6, 2018, and the UNICEF database (maternal mortality only) on June 6, 2018, for the 11 countries. As of December 5, 2018, the UNICEF and OECD data were unchanged.
Acknowledgments
The authors thank Yaphet Getachew, Corinne Lewis, and Arnav Shah of the Commonwealth Fund for assistance with verifying data.
