Key Findings
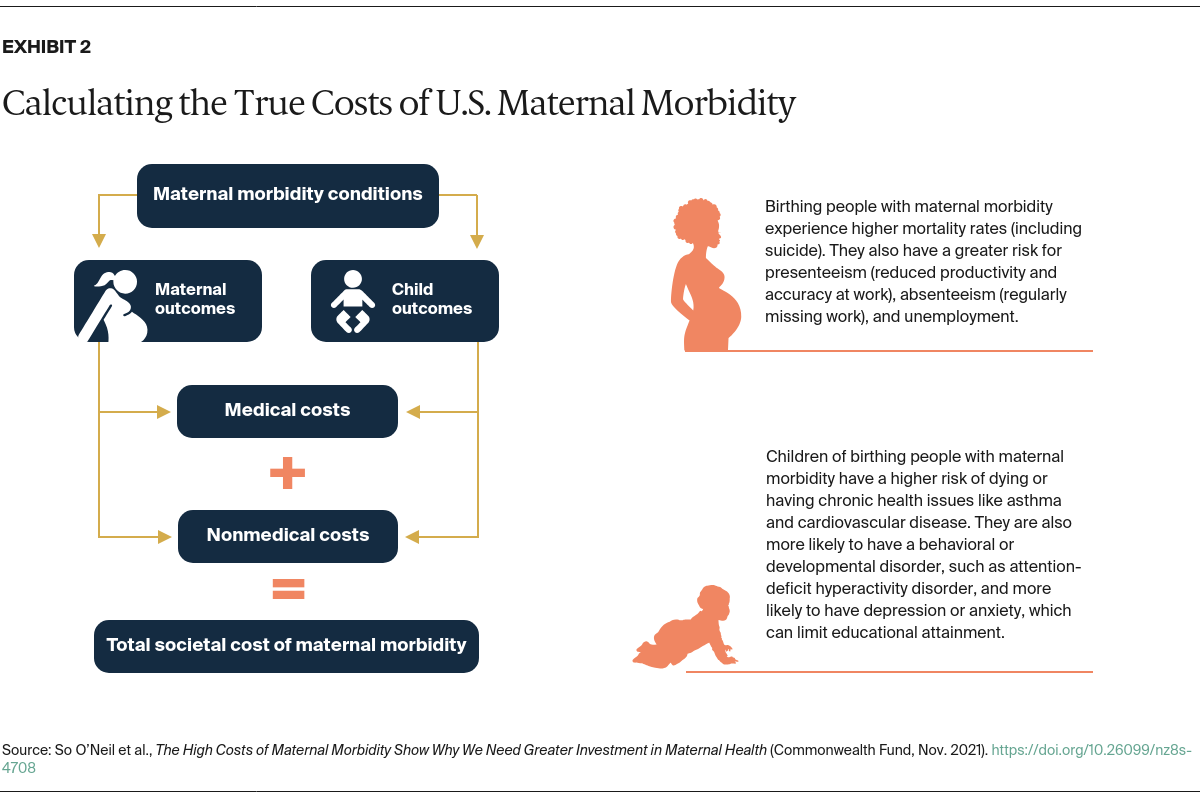
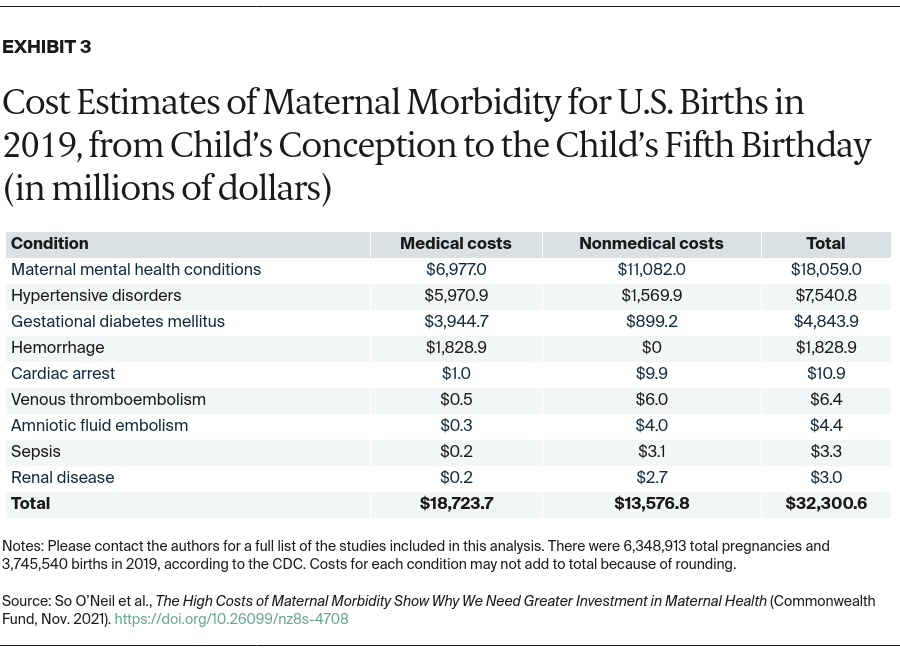
Of the 31 maternal morbidity conditions identified in the literature, we found nine with documented outcomes and associated costs (Exhibit 3).8 The nine conditions include: amniotic fluid embolism, cardiac arrest, gestational diabetes mellitus, hemorrhage, hypertensive disorders, maternal mental health conditions, renal disease, sepsis, and venous thromboembolism.
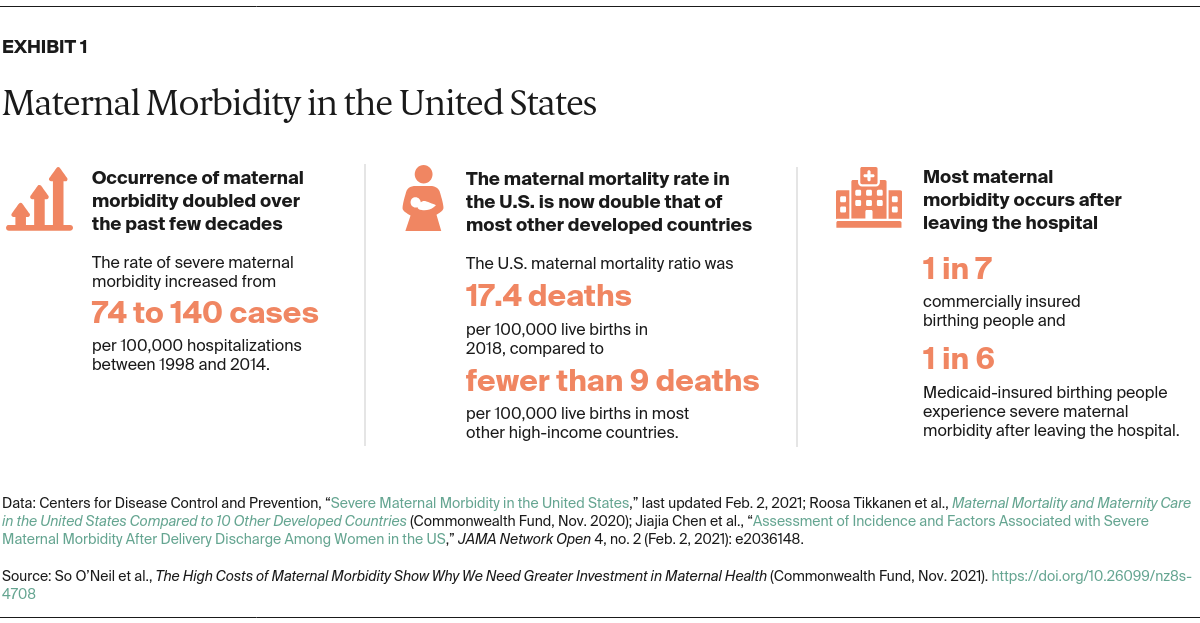
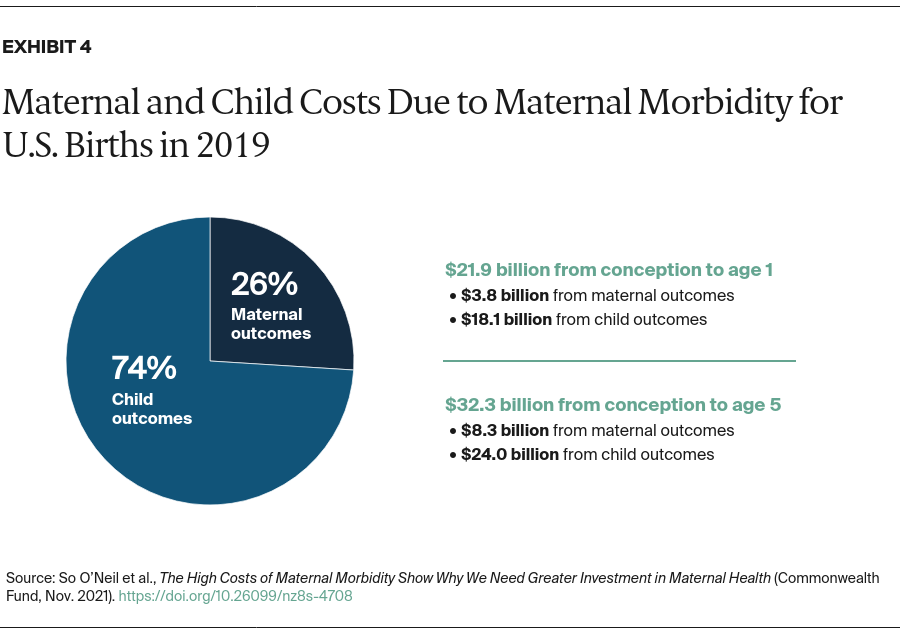
Using prevalence estimates for each condition, we estimated that the total costs of these nine maternal morbidity conditions for all U.S. births in 2019 reached $32.3 billion from conception through the child’s fifth birthday (Exhibit 4). This amounts to roughly $8,624 in additional costs to society for each maternal–child pair associated with 6.3 million pregnancies and 3.7 million births in the U.S. annually. Two-thirds of these costs occurred within the first year postpartum.
The largest costs included maternal mental health conditions ($18.1 billion), hypertensive disorders ($7.5 billion), gestational diabetes ($4.8 billion), and postpartum hemorrhage ($1.8 billion). These conditions also represented the most prevalent conditions among those with documented cost information.
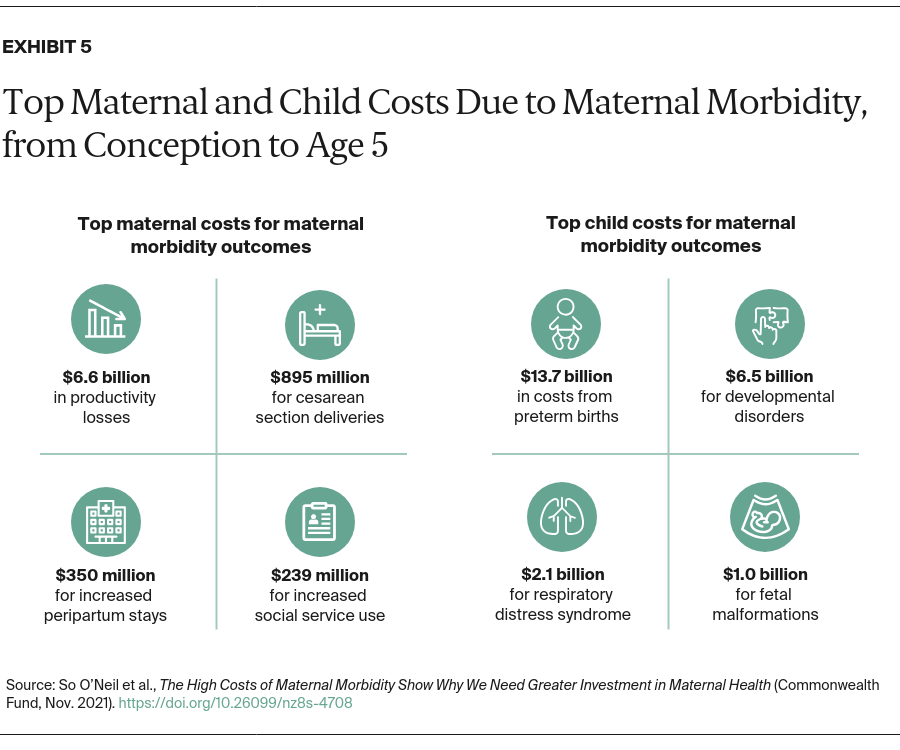
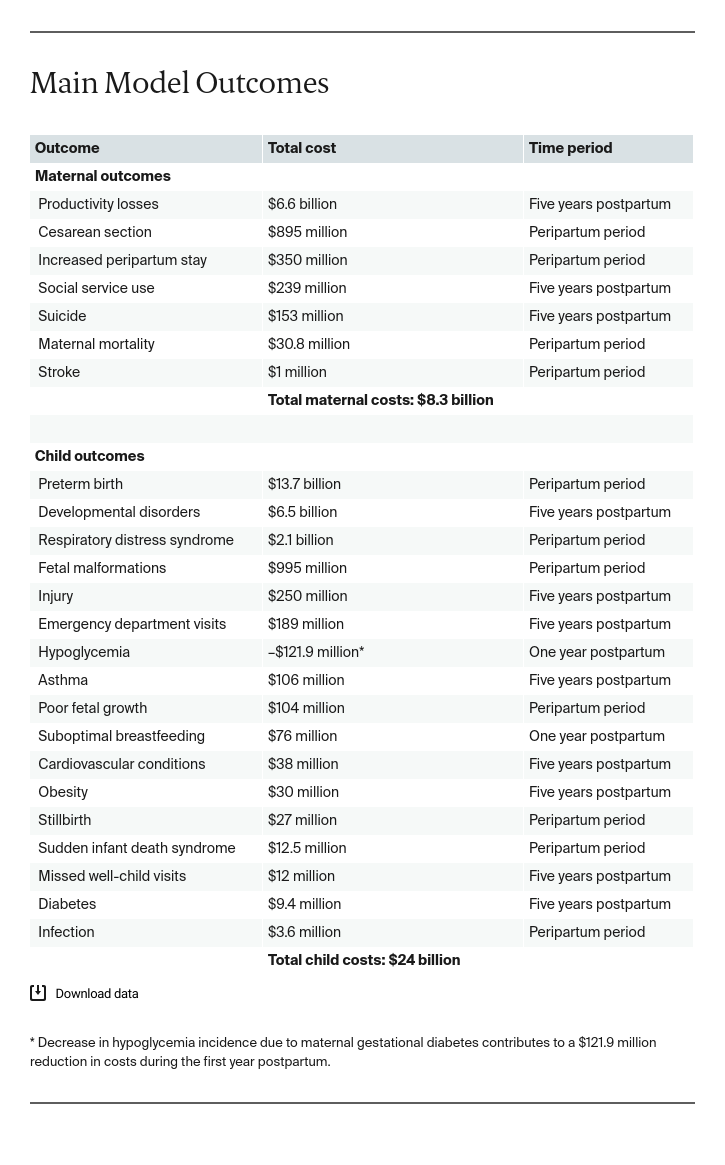
The child outcomes with the highest costs were preterm birth ($13.7 billion), developmental disorders ($6.5 billion), and respiratory distress syndrome ($2.1 billion) (Exhibit 5). The maternal outcomes driving the costs of these conditions included productivity losses ($6.6 billion), cesarean section delivery ($895 million), and increased peripartum stay ($350 million).
The costs of child outcomes ($24.0 billion) far outweighed the costs of maternal outcomes ($8.3 billion) from the beginning of pregnancy through a child’s fifth birthday (Exhibit 4). If there were better data available on maternal morbidity conditions and outcomes, our estimates of the costs of maternal outcomes might have been substantially higher.
The health care system bore more than half these costs (58%), with the rest shouldered by employers, public social services programs, and other nonmedical sectors. These nonmedical costs included losses in productivity ($6.6 billion), costs associated with behavioral and developmental disorders in children ($6.5 billion), and increased use of social programs like SNAP, WIC, Medicaid, and TANF ($239 million).
Limitations of the Study
Our model likely underestimates the true societal costs of maternal morbidity, because data on the many nonmedical costs associated with the nine conditions included in the model were lacking in the research literature. Also missing was supporting evidence for many of the morbidity–outcome connections from our original conceptual model.
In addition, to avoid duplicating cost estimates, we intentionally chose not to model secondary outcomes. For example, one of the outcomes in our model is child developmental disorders, which often require social services, such as Supplemental Security Income payments, to address. Our model did not include this set of costs.
Finally, we designed this model to focus on a six-year period (pregnancy through five years postdelivery) to measure the immediate impacts of maternal morbidity. We recognize, however, that maternal morbidity can have long-term effects on the birthing person and the child. Our estimates may therefore represent only a fraction of lifetime costs.
Discussion
Our model estimated that nine common maternal morbidity conditions associated with births in a given year (2019) cost society $32.3 billion from the beginning of pregnancy through five years postpartum. The lack of comprehensive data for other conditions suggests that maternal morbidity has the potential to exact a much higher toll on society than what we have found, rivaling that of expensive chronic conditions like diabetes, whose costs run into the hundreds of billions of dollars.9
Of the costs documented, medical costs made up the majority (58%). This preponderance of medical costs is likely driven by the relative availability of hospital discharge data compared with other cost information. The focus of these costs on the delivery period also implies our estimates might further miss costs associated with later and longer-term physical and mental health consequences of maternal morbidity for birthing people and their children, including consequences for subsequent pregnancies.10 For example, our maternal mortality cost estimate ($30.8 million) included medical costs due to hospitalization and only the nonmedical costs of maternal funerals; there was no additional information in the research literature on the longer-term physical and psychological costs for other household members.
Nonmedical costs accounted for the other 42 percent of total costs, which mainly stemmed from maternal mental health conditions — the maternal morbidity for which we had the most complete information on outcomes and costs. While the literature contained fewer documented nonmedical costs for the eight remaining maternal conditions in this model, studies of other health conditions have found that nonmedical costs attributable to lost earnings, productivity loss, and other indirect costs can account for more than half of overall costs.11 Additional information on nonmedical costs related to maternal morbidity could raise our estimate of nonmedical and total costs.
Studies also tended to focus on severe maternal morbidity, a more narrowly defined subset of life-threatening maternal conditions. For these conditions, the CDC has published a clear definition of indicators and diagnosis codes that allows researchers to develop medical cost estimates through claims data. Of the nine conditions with sufficient evidence for inclusion in this model, six were included on the list of CDC indicators.12 Development of a broader set of maternal morbidity indicators could improve the data needed to generate medical cost estimates for maternal morbidity. For example, complications during delivery increase medical costs of a vaginal and cesarean delivery by 20 percent and 25 percent, respectively. In addition, our model does not account for medical costs of readmissions linked to maternal morbidity, which could substantially increase our estimate.13
Nevertheless, our cost estimates confirm the substantial toll maternal morbidity has on society and signify further opportunities to invest in maternal health. These investments could support evidence-based maternal health initiatives, such as: midwifery models of care that extend beyond birth; comprehensive gender-specific primary health care that provides seamless transitions in and out of pregnancy; community-based models of care; and telehealth integration for maternal health.14 These initiatives could be supported through various state or federal policies, such as incentives for extended postpartum coverage or expansion of insurance coverage more broadly. Policy also can address reimbursement for measuring and addressing social determinants of health associated with maternal morbidity, such as unstable housing and lack of transportation. Such interventions must specifically address root causes of inequities in maternal health, including structural racism.
Reducing maternal morbidity requires tackling the multiple factors that can influence whether a birthing person experiences maternal morbidity. This starts with measurement to capture, beyond medical care, the social and other factors influencing maternal outcomes. National entities driving measurement, such as the National Quality Forum and CMS, are exploring equity-centered measures that could specifically focus on those related to maternal health. These measures will support the development of better policy and program decisions that comprehensively address the multitude of complex factors underlying maternal morbidity.15 Even without these measures, some states have been spurred to take a more comprehensive, team-based approach to perinatal care, such as by introducing pregnancy medical homes and group prenatal care.16 Although evidence on the effectiveness of cross-sector, place-based initiatives are scarce, these efforts represent a trend toward holistically addressing the social and clinical determinants of maternal and child health.17
Conclusion
The cost of maternal morbidity has significant implications for delivery system leaders and policymakers. System failures that result in today’s severe maternal morbidity can result in tomorrow’s maternal death, which makes preventing morbidity even more critical to addressing the U.S. maternal health crisis.
Affordable, continuous health insurance coverage is one part of the equation — albeit an important one. This includes an extension of postpartum Medicaid coverage for up to one year to help ensure that key physical and mental health needs following birth are identified and met. Health systems and payers can further address maternal health outcomes by increasingly monitoring maternal morbidity measures and undertaking root-cause analyses to address any inequities or adverse outcomes and to drive improvement. The growing recognition of the serious effects of maternal morbidity on families and society provides an opportunity to further invest in measurement to promote evidence-informed policy change and programming for maternal health.