Synopsis
Patients at a large primary care clinic that adopted the patient-centered medical home model, along with improvements in disease management and changes to staffing and physician payment, reported improved satisfaction with their care, including better communication with providers. The findings run contrary to previous research that concluded the care model, which requires practices to undergo intensive and potentially disruptive transformation, can negatively affect patients’ experiences in the short term.
The Issue
Some research indicates that, although the patient-centered medical home (PCMH) has the potential to improve patient care quality and reduce costs, implementing the reforms at the center of the model—including reorganizing staff into care teams and adopting electronic medical records—can lead to declines in patient satisfaction in the short term. Commonwealth Fund–supported researchers compared patients’ experiences in a primary care clinic that implemented the PCMH model, along with lean process changes (which seek to maximize value and reduce waste) and a new approach to physician reimbursement, with patients’ experiences in a similar clinic that did not make such changes. The lean changes focused on improving chronic disease management and reassigning tasks traditionally performed by physicians to medical assistants or nurses. The new payment approach replaced physicians’ fee-for-service–based compensation with a salary and bonus arrangement.
Key Findings
-
 At the intervention site, overall satisfaction was higher following adoption of the new care model: 68 percent of patients rated their care as "very good," compared with 62 percent prior to the intervention.
At the intervention site, overall satisfaction was higher following adoption of the new care model: 68 percent of patients rated their care as "very good," compared with 62 percent prior to the intervention. - At the control site, 63 percent of patients were satisfied during the pre-intervention period compared with 64 percent after.
- The researchers found no statistically significant differences in patients’ overall satisfaction between the intervention and control sites, though there were some trends toward improvement.
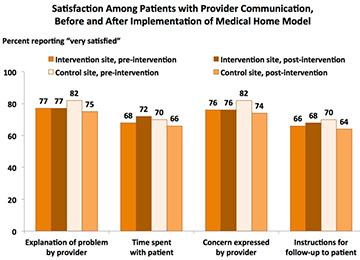
- At the intervention practice, there were patterns of consistent or improved patient satisfaction on measures assessing physician communication. Following the intervention, patients rated their providers the same or more highly on the amount of time they spent with them, their expressions of concern, follow-up instructions, and explanations provided. In contrast, control practice patient ratings fell during the study period.
Addressing the Problem
This investigation did not find evidence that implementation of the patient-centered medical home, when combined with lean changes and provider payment reform, negatively affected patients’ experiences. In fact, the findings suggest that this delivery model may bolster patient–provider relationships. Physicians at the intervention site may have felt reduced time pressure as a result of the workforce changes and their new payment structure, perhaps freeing up time for more in-depth and better-quality conversations with patients. Practices interested in the PCMH model, the authors say, may want to consider reforming physician payment early in the transformation process.
About the Study
The research team surveyed 2,500 patients following their office visits both before and after the intervention clinic implemented the PCMH model (Jan. 2008–June 2009 and July 2009–Dec. 2010). Approximately 1,600 patients were also surveyed at a comparison clinic. Both clinics are part of the same multispecialty group practice and serve a similar demographic of patients. The patient survey included an overall rating of care as well as questions related to enhanced access, visit coordination and care, physician communication, and whole-person orientation of care.
THE BOTTOM LINE
Despite the potential for disruption or frustration in the short term, patients reported higher overall satisfaction at a primary care practice that adopted the patient-centered medical home model along with lean process changes and physician payment reform.
