By Douglas McCarthy
Summary: Worksite health clinics that focus on comprehensive primary care and wellness have helped lower costs and improve care for employees of the Wisconsin printing company Quad/Graphics. This approach transforms the role of employers from mere purchasers of health insurance to investors in employee health and productivity.
Issue: Employers can play a key role in improving the value of health care that they purchase and arrange for employees and their family members by establishing onsite health clinics. Recently, employers have shown renewed interest in such clinics as a way to boost worker productivity, enhance convenient access to care, improve prevention and wellness, and control health care costs.1 Such an approach has the potential to act as what Harvard Business School Professor Clayton Christensen calls a "disruptive innovation" in the marketplace for employer-sponsored health care—one that can dramatically lower costs and improve care for patients.2
Quad/Graphics, a Wisconsin-based printing company, was one of the first employers to offer comprehensive worksite health clinics in recent decades. Nearly 20 years ago, the founder of this family-owned business, Harry Quadracci, noticed his employees were complaining of problems with medical claims or the quality of care while at the same time the company's medical costs were soaring.3 Taking a cue from the company's business strategy, which integrates printing activities from design to distribution, he set out to create a more reliable and efficient health care system for his employees by "cutting out the middleman" and bringing the provision of primary health care in-house.
Objective and Intervention: Quad/Graphics invests in employee health and productivity and promotes health care value by integrating worksite primary care services and wellness programs with a directly contracted specialty care and hospital provider network as part of a self-funded employee health care benefits plan. Quadracci framed the objective of this approach from the employee's perspective: "We'll keep you well; and by the way, if you get sick, we'll take care of that, too."
Organization: Founded in 1971, Quad/Graphics is the nation's largest privately held commercial printing company with 9,000 non-unionized employees, 10 printing plants in six states, and more than $2 billion in annual revenues. QuadMed, LLC, a subsidiary of Quad/Graphics, operates the worksite clinics, related fitness and rehabilitation facilities, and wellness programs on behalf of Quad/Graphics and other employer clients. QuadMed participates in the Institute for Healthcare Improvement's Triple Aim initiative, the goal of which is to help health care organizations simultaneously achieve improvements in the individual experience of care, the health of the population, and the per capita cost of care.
Implementation and Leadership: QuadMed began with a single physician and a single nurse staffing a small worksite clinic at the company's Pewaukee, Wisc., plant in 1990. As the clinic gained acceptance with employees, Harry Quadracci (the late founder and CEO) recruited his brother, Leonard Quadracci, M.D., a kidney specialist, to run the unit and expand its scope and capacity companywide. QuadMed's current president, Raymond Zastrow, M.D., took over when Leonard Quadracci retired in early 2008. Thomas Van Gilder, M.D., J.D., M.P.H., medical director for quality initiatives, joined QuadMed over three years ago and practices internal medicine at the clinic located in Quad/Graphics' West Allis, Wisc., plant.
Target Population: QuadMed delivers care to more than 20,000 employees, family members, and some retirees of Quad/Graphics. About 85 percent of the Quad/Graphics workforce gets care at QuadMed clinics, which are located at or near three plants in the Milwaukee, Wisc., area, Saratoga Springs, N.Y., and Martinsburg, W.Va. (Exhibit 1).
QuadMed has operated clinics for workforces (unionized and non-unionized) at the MillerCoors plant in Milwaukee and at Briggs & Stratton plants in Milwaukee and Poplar Bluff, Mo. for a number of years. (Employees at Briggs & Stratton and MillerCoors may use Quad/Graphics' onsite clinics for care as well.) In September 2009, QuadMed also began operating two on-site clinics for the Milwaukee-based financial services provider Northwestern Mutual.
Exhibit 1.
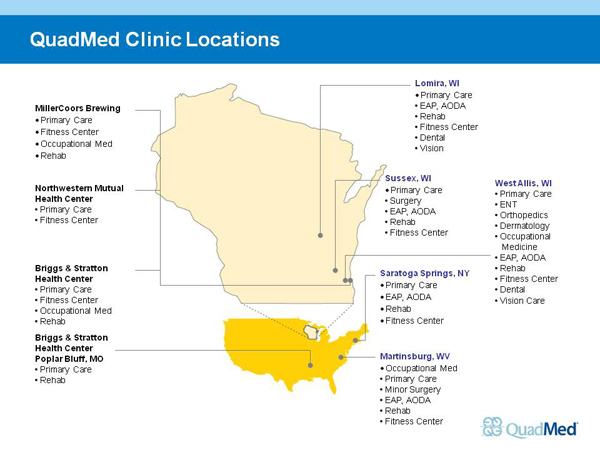
Source: QuadMed
Services Offered: QuadMed clinics offer a full range of primary care, dental and vision care, and occupational medicine as well as selected specialty care such as cardiology, dermatology, obstetrics/gynecology, and orthopedic surgery. Onsite ancillary services include pharmacy, X-ray, laboratory, rehabilitation clinics, and fitness centers. Clinic patients with mental and behavioral health needs also have access to an employee assistance program (EAP) and alcohol and other drug abuse services. QuadMed directly contracts with a "high-performance network" of local hospitals, specialists, and radiology practices to provide services not offered at the onsite clinics. Participation in the network is determined based on providers' pricing and their reputation for quality and responsiveness.
Quad/Graphics' point-of-service plan gives employees a choice of providers with variable cost-sharing requirements that encourage (but do not require) the use of worksite clinics. For those who use QuadMed clinics for their primary care, copayments are $6 for any visit to a QuadMed clinic and $30 for visits to specialty physicians in the network, plus a $100 deductible. (Patients do not need a referral to visit a specialist.) Employees who do not use QuadMed clinics pay 20 percent coinsurance after a $200 deductible for care within the network or 30 percent coinsurance after a $300 deductible for care outside the network. (Family deductibles are twice the employee level.)
Practice of Care: QuadMed's worksite clinics offer more than just convenience for patients. According to Van Gilder, the clinics provide a holistic approach to care made possible by unhurried visits lasting 30 minutes or longer, along with short waiting times and integration of onsite ancillary services such as pharmacy and laboratory services. Patients "know that they will get in, see the doctor after a very brief wait, and end the visit ready to go" without having to travel across town for a lab test or X-ray, he says. During the time employees might have spent traveling to a doctor's office, they can instead actually be seen by and talk with their doctor. Patients also may see midlevel practitioners (physician assistants or nurse practitioners) for urgent care and ongoing chronic care needs.
"When somebody comes in for a sore throat, it's expected that we'll not only address the sore throat, which may take just a few minutes, but we'll address all of their health concerns and all of their appropriate health screenings at that visit," Van Gilder explained. "That allows a doctor-patient relationship to develop, so that when either more complex problems come around or when some of the more difficult prevention topics come up—whether physical activity or diet or smoking cessation—we've developed a relationship that people feel they can trust and come to us for their care and wellness needs."
Protecting medical privacy is key to maintaining employees' trust: QuadMed promises not to share patients' medical records with the company's human resources department. "We emphasize that we are very protective of their health information, and we monitor who has access to the charts," said Van Gilder. Clinicians wear a different uniform than plant employees to emphasize they are not "company doctors" but patient advocates. "It's a daily struggle to maintain that trust, because any breach [of privacy] would be a serious threat to our ability to continue to do the work that we do," Van Gilder said.
QuadMed has used an electronic medical record (EMR) system for more than 10 years. It recently converted to General Electric's Centricity system and is currently installing functionality that will provide real-time prompts to physicians in the exam room when a patient is due for preventive care. The system will also supports monthly reporting so that physicians can track their performance for an entire patient panel. Most physicians enter progress notes directly in the EMR, but a few continue to dictate and the transcription is then entered in the EMR.
Care Coordination: In Wisconsin, QuadMed has established a close relationship with one of the region's hospital systems (Wheaton Franciscan Healthcare), whose hospitalists care for QuadMed patients when they are admitted. QuadMed clinicians can use a portal into Wheaton Franciscan's information system to view admission and progress notes and the results of inpatient laboratory and imaging studies. The hospital also faxes discharge notes to QuadMed when patients leave the hospital. Quad/Graphics' claims adjudicators also alert the clinic when a patient has a major medical issue that appears to require follow-up.
To promote good care coordination, QuadMed periodically hosts receptions with area medical specialists and informally evaluates their patients' experiences with referrals and the specialists' communication with the primary care providers. QuadMed also encourages patients to have laboratory testing done at the clinic prior to specialty consultations and elective surgery, so that test results will be captured in the clinic's EHR.
Population Health: To support this emphasis on comprehensive care, QuadMed has developed wellness programs (such as "Lean You," described below) that engage patients at the worksite and outside the clinic. Wellness is considered the foundation of the QuadMed program, part of the company's "social contract" with its employees. "There's a real sense of taking care of each other—not just to make an extra buck, but to make sure everyone's doing all right, both for the health of the company and for the community," Van Gilder observed.
Wellness programs are coordinated by appointed (volunteer) wellness champions and paid fitness coordinators throughout the company. Employees and their spouses are eligible and encouraged to sign up during the annual open enrollment period (when they select benefit options) as well as throughout the year. Clinicians routinely assess their patients' body mass and exercise habits during clinic visits, encourage them to participate in wellness programs, and perform physical evaluations as part of program enrollment.
The goals of the "Lean You" wellness program are to promote physical activity, weight loss, smoking cessation, and early identification and control of diabetes as well as risk factors for cardiovascular disease. Participants receive a $2 discount off their weekly health insurance premium; those who promise not to smoke or who quit smoking (and attest to being tobacco free) earn an additional $8 weekly discount (worth a total of $520 per year). Participants track their progress on a personalized Web page and can earn annual cash incentives of $400 for meeting all of the program's goals, $175 for meeting some goals, and $50 for making some progress toward meeting the goals (Exhibit 2).
Diabetic patients participating in "Lean You" can qualify for a "Well You for Diabetes" program that provides quarterly consultations (face-to-face and virtually) with a certified diabetes educator to support disease control. Copayments for diabetes medications and supplies are waived (a benefit worth about $400 annually) if participants meet program criteria, including regularly refilling medications, getting all diabetic tests and attending physician visits, quarterly contacts with the diabetes educator, and meeting outcome goals for glucose, blood pressure, high cholesterol, weight loss, exercise, and smoking.
The certified diabetes educator, Diane Collelo, R.N., works in close partnership with primary care physicians. For example, she and Van Gilder often see diabetic patients during the same clinic visit, with Collelo engaging patients in self-management education so that Van Gilder can focus on clinical management, including identification and treatment of comorbid conditions. Collelo keeps a registry of diabetes patients and follows-up with those who fail to make regular clinic appointments or quarterly contacts.
Exhibit 2: Participant Goals for the "Lean You" Wellness Program
1. Be tobacco free by July 1 of enrollment year.
2. Be at or reach body mass index (BMI) of less than 27, or lose 10 percent of body weight in one year, whichever is less.
3. Exercise a minimum of three times a week for a duration of 30 minutes each time (does not have to be at a Quad/Graphics fitness center).
4. Control blood pressure and LDL-cholesterol within national guidelines and have normal glucose (or, if diabetic, at hemoglobin A1c goal).
5. Complete an annual preventive health exam with a primary care professional who attests that all health maintenance is up to date.
6. Complete an online health risk appraisal (www.HowsYourHealth.com).
Source: QuadMed
The use of data is a critical management tool for evaluation and benchmarking at QuadMed. All clinic visits are captured as encounters in the company's claims system and combined with data on care received from community providers. A 2005 analysis, for example, found that obesity was a major contributing factor to health care spending: costs for overweight, obese, and morbidly obese employees were 35 percent, 54 percent, and 94 percent higher, respectively, than for normal weight employees. This insight led the company to adopt a "value-based" benefit design that eliminates copayments for weight management services and diabetes medications (the latter as part of the "Well You for Diabetes" program) to encourage better disease prevention and control.4
Staffing: QuadMed employs 40 full-time-equivalent health care providers. At the West Allis plant, for example, the clinic staff includes four internal medicine physicians, two family physicians, a pediatrician, two physician assistants, and a nurse practitioner. The company also contracts with several specialists to provide care on a part-time basis at the onsite clinics. Employed providers are paid market-competitive salaries, with incentive bonuses (worth about half of a potential 10 percent annual bonus) for meeting quality targets based on national clinical guidelines and patient satisfaction and for participation in clinic governance. Staffing is not determined by fixed patient-to-physician ratios but based on meeting patient scheduling demand.
QuadMed initially hired experienced community physicians who were attracted to the opportunity to move away from production-oriented care to patient-centered care. As its model has gained a track record, the company has had success hiring physicians from residency programs. Newly hired physicians receive on-the-job training to become conversant in QuadMed's approach to care. "I think in part we retain people because the people get hooked on being able to take care of patients in an atmosphere that really fosters wellness instead of a crazy paperwork-driven production model where you have to see somebody every seven or 10 minutes," Van Gilder said.
QuadMed providers meet as a group four times per year, supplemented by smaller meetings, to engage in peer education and peer review. "We look at how quality targets are being met and we try to do so in a very collegial way without penalties and without untoward incentives. We have the standards and we help each other meet them and by and large we all do," Van Gilder said. During the recent novel H1N1 pandemic, for example, staff members from adult and pediatric medicine, along with lab personnel, reviewed national, state, and local guidelines to provide clearer, more clinically relevant recommendations to all QuadMed staff and help ensure consistent, evidence-based care for flu patients and their families.
Results: Participation in the "Lean You" wellness program has increased from 22 percent of Quad/Graphics employees in 2005, the first year it was offered, to 70 percent today. About 25 percent of the participants achieve all programs goals and qualify for the full incentive reward. QuadMed estimates that the "Lean You program more than pays for itself. In 2005, for example, the estimated program costs were $240,000, compared with estimated savings of almost $2 million from early diagnosis of four cases of cancer detected during enrollment exams.5
More than 200 of the 732 diabetic patients in Quad/Graphics' workforce are participating in the "Well You for Diabetes" program and have reduced their hemoglobin A1c levels (a measure of blood glucose control) from 8 percent to 7.5 percent on average. Observation suggests that participants have improved emotional well-being as well.
Quad/Graphics spends more on primary care per patient than the average employer, but makes up the difference in lower costs for emergency department visits and hospitalizations. In 2008, for example, Quad/Graphics' outpatient visit rate was 15 percent higher for employees and family members in Wisconsin compared with the Midwest norm (434.2 vs. 377.5 visits per 100 lives), while its inpatient visit rate was more than 9 percent lower (55.7 vs. 61.5 per 1000 lives).
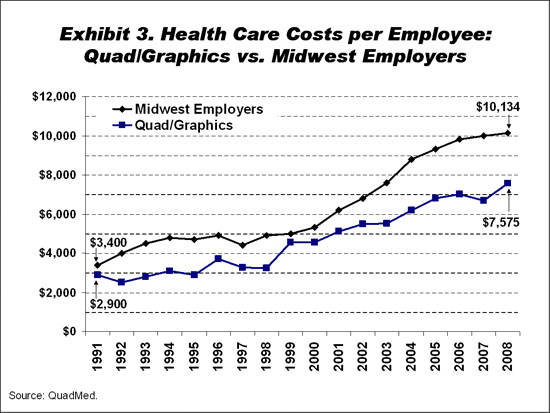
The difference in dollars between Quad/Graphics' health care costs and those of other Midwestern employers has widened from $500 per employee (including family members) in 1991 to more than $2,500 lower in 2008 (Exhibit 3). Since 1999, costs have risen at an average annual rate of 6 percent at Quad/Graphics versus 8.3 percent at other Midwestern employers (medical inflation in Milwaukee was almost 1 percent lower than average for Midwestern cities represented in the Consumer Price Index). Although Quad/Graphics' employees are somewhat younger than the regional average, an actuarial analysis by Mercer Consulting found that Quad/Graphics’ costs were below the benchmark after adjusting for differences in demographics and benefit designs, widening from 18 percent lower in 1998 to 31 percent lower in 2008. This widening difference in costs suggests that QuadMed’s approach has been successful in "bending the cost curve."
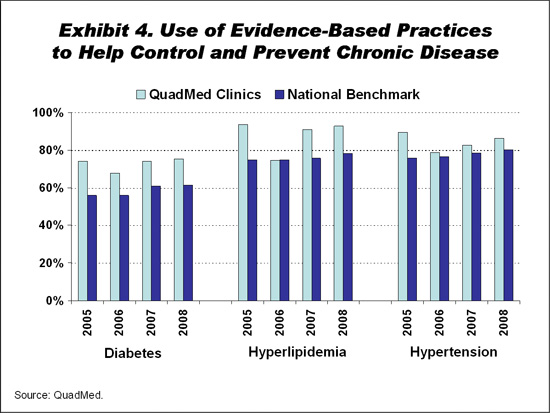
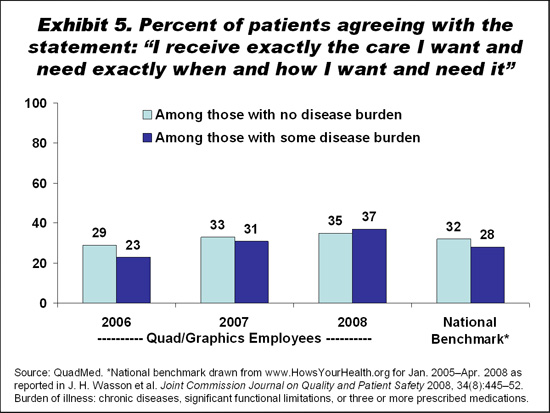
Quality results for Quad/Graphics' patients treated at QuadMed clinics are at or above national employer benchmarks for the use of evidence-based practices to help control diabetes (75.3% vs. 61.4%), blood pressure (86.4% vs. 80.1%), and high cholesterol (92.6% vs. 78.0%) (Exhibit 4). Patient satisfaction has been increasing, with the proportion reporting that "I receive exactly the care I want and need exactly when and how I want and need it" rising by 14 percentage points among patients who are burdened by disease from 2006 to 2008, surpassing the national benchmark and the satisfaction level among healthy patients (Exhibit 5). Four of five QuadMed patients say that they would recommend QuadMed.
Lessons Learned: QuadMed appears to have achieved widespread acceptance in a family-oriented workplace by providing comprehensive onsite primary care in a way that prioritizes patient health and convenience. The critical success factor is organizing care so that it is oriented toward outcomes rather than production, with key ingredients including salaried physicians, extended patient visits, and integrated wellness programs, according to John Neuberger, vice president of operations. "We can't find a primary care model in any market that is as generous and as considerate of what we want to accomplish for our employees and their families," he said.
The payoff is more than financial, said Van Gilder: "Investing in employee health—and not simply paying health care claims or premiums—can really have returns: not only in terms of costs, but also in quality, wellness, retention of employees, and productivity. People think of these [returns] as being only very long-term, but we see that some of these things start helping almost immediately. As Joel Quadracci (son of the founder and current CEO) said, 'Who would have thought that health care would become a competitive advantage for a printing company?'"
QuadMed has not found that obese individuals are more likely (than non-obese individuals) to participate in wellness programs, suggesting that multifaceted approaches are needed to reach all segments of the workforce. Imposing a requirement for complying with lifestyle changes means that some workers postpone joining the diabetes wellness program until they get weight under control and are ready to make a commitment to quit smoking, Collelo said. This experience suggests that employers offering similar wellness programs should consider ways to help people work through stages of readiness for change.
"Treating the whole person makes us more successful" in helping patients control their diabetes, Collelo observed. "We can teach anybody a standard; it doesn't mean they'll follow it. Nobody gets up and says, 'I'm going to be noncompliant today.' We have to figure out why they are noncompliant and how can we overcome their noncompliance... whether it's financial (which can be addressed by waiving copayments), do they not like to stick their fingers, do they have difficult work schedules or a tough family life, do they need an EAP consult, things like that."
Implications: It is unclear how many companies are likely to adopt Quad/Graphics' hands-on approach to "in-sourcing" the provision of comprehensive worksite health care. Some companies prefer to outsource the operation of worksite clinics to outside vendors, as MillerCoors and Briggs & Stratton have hired QuadMed to do. Fuld & Company reports that 24 vendors currently manage 2,200 worksite clinics for 1,200 employers. Its market research suggests that the number of worksite clinics could grow by up to 20 percent year and that they could serve 10 percent of the under-65 population (employees and their families) by 2015.6
Company size is a limiting factor in the spread of worksite clinics. QuadMed finds that a company needs to have 1,000 to 2,000 employees before an onsite health clinic will be cost-effective. (There were 5,510 private-sector establishments employing 1,000 or more workers at one location in the U.S., representing 11.6 million workers or 10 percent of the private-sector workforce in 2007.7 ) Still, smaller companies can adopt portions of the model, such as a part-time onsite nurse practitioner or wellness programs with incentives that are tied to chronic disease management.
Successfully providing care in different work environments requires being attuned to their particular culture, according to Van Gilder. At unionized companies, for example, gaining employees' trust is especially critical to overcome skepticism about management-led initiatives. The union can become an advocate for onsite clinics if its members perceive that they are genuinely oriented to improving employees' health and well-being. Offering employees the choice of using onsite clinics or other community providers also helps build acceptance and distinguishes this approach from company-run clinics of the past.
Should worksite health care spread widely as part of a larger movement toward primary care "medical homes," it could help induce a shift in emphasis toward primary care and away from more costly specialty and hospital care, which could require changes in the composition of the health care workforce. "I think we offer a better way of practicing medicine: the way that we wanted [to practice] when we started into primary care," Van Gilder noted. "And we removed some of the administrative and other overhead-type hassles. In exchange, folks get a chance to flourish as physicians and develop lasting and trusting relationships with patients."
Some observers have expressed concern that widespread use of worksite health clinics could have a detrimental effect on the viability of other community physician practices, in which the patient mix would shift toward a greater proportion of those covered by Medicare and Medicaid, which tend to pay lower rates than commercially insured patients.8 On the other hand, competition for privately insured patients might induce community physicians to undertake changes in their practices to match the perceived value offered by worksite clinics. In today's market, Neuberger doesn't think worksite clinics are a threat to primary care practices, which are often overwhelmed by demand for their services. Worksite clinics may help relieve some of this pressure so that community physicians are able to provide better care to their remaining patients.
For Further Information: Contact Thomas Van Gilder at [email protected].
Notes
1. Mercer's 2008 National Survey of Employer-Sponsored Health Plans found that 32 percent of large employers (500+ employees) had worksite clinics that offered occupational health services and 13 percent had clinics that provided primary care services at or near the worksite. For more on worksite clinics, see: Watson Wyatt Worldwide, Realizing the Potential of Onsite Health Centers, 2008; and Mercer, Survey on Worksite Medical Clinics, 2008.
2. C. M. Christensen, J. H. Grossman, and J. Hwang, The Innovator's Prescription: A Disruptive Solution for Health Care (New York: McGraw Hill, 2009).
3. V. Fuhrmans, "Radical Surgery—One Cure for High Health Costs: In-House Clinics at Companies," Wall Street Journal, Feb. 11, 2005, A1.
4. A. Helwig, D. Schultz, and L. Quadracci, "Obesity and Corporate America: One Wisconsin Employer's Innovative Approach," Wisconsin Medical Journal, 2005 104(5):15–18.
5. R. J. Zastrow and L. Quadracci, "Engaging Quad/Graphics Employees in the Improvement of Their Health and Healthcare," Journal of Ambulatory Care Management, 2006 29(3):225–9.
6. Fuld & Company, The Growth of On-Site Health Clinics, Feb. 2009.
7. U.S. Bureau of Labor Statistics, Employment and Wages, Annual Averages 2007, Table 3.
8. K. Terry, Worksite Clinics—The Next Threat? Physicians Practice, May 2009.
This study was based on publicly available information and self-reported data provided by the case study institution(s). The Commonwealth Fund is not an accreditor of health care organizations or systems, and the inclusion of an institution in the Fund's case studies series is not an endorsement by the Fund for receipt of health care from the
institution.
The aim of Commonwealth Fund–sponsored case studies of this type is to identify institutions that have achieved results indicating high performance in a particular area of interest, have undertaken innovations designed to reach higher performance, or exemplify attributes that can foster high performance. The studies are intended to enable other institutions to draw lessons from the studied institutions' experience that will be helpful in their own efforts to become high performers. It is important to note, however, that even the best-performing organizations may fall short in some areas; doing well in one dimension of quality does not necessarily mean that the same level of quality will be achieved in other dimensions. Similarly, performance may vary from one year to the next. Thus, it is critical to adopt systematic approaches for improving quality and preventing harm to patients and staff.